J Korean Med Sci.
2021 Jun;36(22):e163. 10.3346/jkms.2021.36.e163.
The Performance of the Current Risk Prediction Scoring Systems in Patients Undergoing Anaortic Off-pump Coronary Artery Bypass Grafting
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2516584
- DOI: http://doi.org/10.3346/jkms.2021.36.e163
Abstract
- Background
This study aimed to evaluate the performance of the Society of Thoracic Surgeons (STS) risk model and European System for Cardiac Operative Risk Evaluation (EuroSCORE) II for patients undergoing anaortic off-pump coronary artery bypass grafting (OPCAB).
Methods
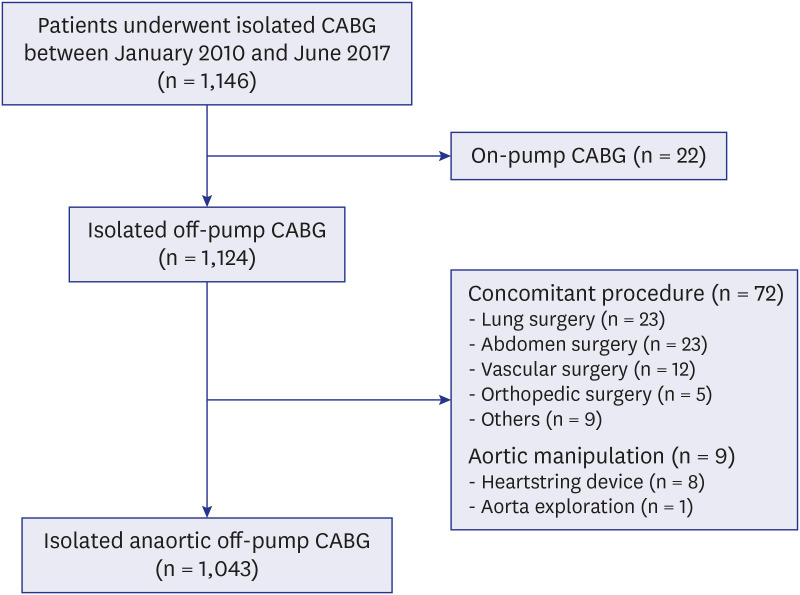
From January 2010 to June 2017, 1,048 patients (isolated anaortic OPCAB: 1,043, on-pump conversion:5) undergoing isolated anaortic OPCAB were enrolled. The STS risk score and EuroSCORE II were calculated with dedicated online software. Calibration of the models were performed by the risk-adjusted event ratio that was defined as observed events divided by expected events (O/E ratio) and Hosmer-Lemeshow test. The discrimination powers were evaluated by the area under the receiver operating characteristic curve (AUC).
Results
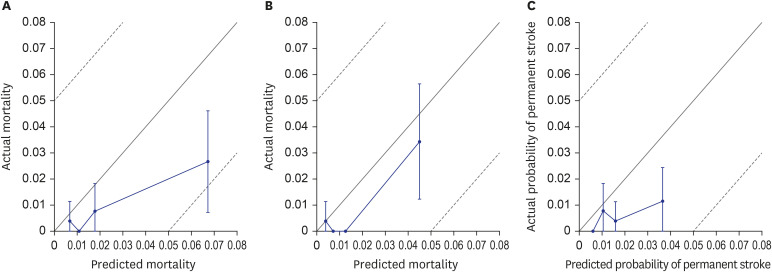
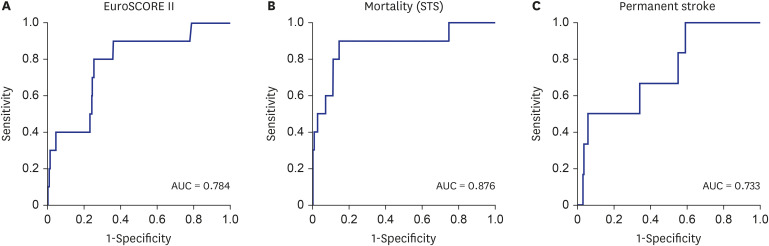
Operative mortality occurred in 10 patients (0.95%). The predicted mortality rates by the EuroSCORE II and STS risk model were 2.58 ± 4.15% and 1.72 ± 2.92%, respectively. The O/E ratio of the EuroSCORE II was 0.370 with significant overprediction of operative mortality (confidence interval [CI], 0.157–0.652; P = 0.003). The STS score also overpredicted the operative mortality (O/E ratio, 0.556) with marginal significance (CI, 0.266–1.023; P = 0.052). Permanent stroke occurred in 6 patients (0.53%). The predicted permanent stroke occurrence rate was 1.73 ± 1.48%. The O/E ratio was 0.332 with significant overprediction of permanent stroke (CI, 0.121–0.722; P = 0.011). Regarding discrimination power for the STS risk model, the operative mortality was excellent (AUC, 0.876) and permanent stroke was acceptable (AUC, 0.740). The EuroSCORE II showed good discrimination power (AUC, 0.784). There was a significant difference in discrimination power for mortality between STS and EuroSCORE II risk models (P = 0.007).
Conclusion
Preexisting risk predicting scoring systems, STS risk model and EuroSCORE II, overpredict the risk of mortality and stroke rate for anaortic OPCAB. These findings suggest the possibility that anaortic OPCAB can lower the operative mortality and occurrence of postoperative stroke than conventional coronary artery bypass grafting.
Figure
Reference
-
1. Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012; 41(4):734–744. PMID: 22378855.
Article2. Shahian DM, Jacobs JP, Badhwar V, Kurlansky PA, Furnary AP, Cleveland JC Jr, et al. The Society of Thoracic Surgeons 2018 adult cardiac surgery risk models: Part 1-background, design considerations, and model development. Ann Thorac Surg. 2018; 105(5):1411–1418. PMID: 29577925.3. O'Brien SM, Feng L, He X, Xian Y, Jacobs JP, Badhwar V, et al. The Society of Thoracic Surgeons 2018 adult cardiac surgery risk models: Part 2-statistical methods and results. Ann Thorac Surg. 2018; 105(5):1419–1428. PMID: 29577924.4. Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, et al. Coronary artery bypass grafting with and without manipulation of the ascending aorta: a network meta-analysis. J Am Coll Cardiol. 2017; 69(8):924–936. PMID: 28231944.5. Misfeld M, Brereton RJ, Sweetman EA, Doig GS. Neurologic complications after off-pump coronary artery bypass grafting with and without aortic manipulation: meta-analysis of 11,398 cases from 8 studies. J Thorac Cardiovasc Surg. 2011; 142(2):e11–7. PMID: 21281950.6. Kim KB, Kim JS, Kang HJ, Koo BK, Kim HS, Oh BH, et al. Ten-year experience with off-pump coronary artery bypass grafting: lessons learned from early postoperative angiography. J Thorac Cardiovasc Surg. 2010; 139(2):256–262. PMID: 20106389.
Article7. European System for Cardiac Operative Risk Evaluation. Accessed February 23, 2020. http://www.euroscore.org.8. Online STS Adult Cardiac Surgery Risk Calculator. Accesssed February 23, 2020. https://riskcalc.sts.org/.9. Nezic D, Borzanovic M, Spasic T, Vukovic P. Calibration of the EuroSCORE II risk stratification model: is the Hosmer-Lemeshow test acceptable any more? Eur J Cardiothorac Surg. 2013; 43:206. PMID: 22728228.
Article10. Hosmer DW Jr, Lemeshow S, Sturdivant RX. 5.2.2 The Hosmer-Lemeshow tests. Applied Logistic Regression. 3rd ed. New York, NY, USA: Wiley;2013. p. 157–169.11. Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Paolasso E, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med. 2013; 368(13):1179–1188. PMID: 23477676.
Article12. Shroyer AL, Grover FL, Hattler B, Collins JF, McDonald GO, Kozora E, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med. 2009; 361(19):1827–1837. PMID: 19890125.
Article13. Borger MA, Peniston CM, Weisel RD, Vasiliou M, Green RE, Feindel CM. Neuropsychologic impairment after coronary bypass surgery: effect of gaseous microemboli during perfusionist interventions. J Thorac Cardiovasc Surg. 2001; 121(4):743–749. PMID: 11279417.
Article14. Patel NC, Deodhar AP, Grayson AD, Pullan DM, Keenan DJ, Hasan R, et al. Neurological outcomes in coronary surgery: independent effect of avoiding cardiopulmonary bypass. Ann Thorac Surg. 2002; 74(2):400–405. PMID: 12173820.
Article15. Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Onnasch JF, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003; 75(2):472–478. PMID: 12607656.
Article16. Navia D, Vrancic M, Vaccarino G, Piccinini F, Raich H, Florit S, et al. Total arterial off-pump coronary revascularization using bilateral internal thoracic arteries in triple-vessel disease: surgical technique and clinical outcomes. Ann Thorac Surg. 2008; 86(2):524–530. PMID: 18640327.
Article17. Houlind K, Kjeldsen BJ, Madsen SN, Rasmussen BS, Holme SJ, Nielsen PH, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients: results from the Danish on-pump versus off-pump randomization study. Circulation. 2012; 125(20):2431–2439. PMID: 22523305.18. Diegeler A, Börgermann J, Kappert U, Breuer M, Böning A, Ursulescu A, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med. 2013; 368(13):1189–1198. PMID: 23477657.
Article19. Lamy A, Devereaux PJ, Prabhakaran D, Taggart DP, Hu S, Straka Z, et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med. 2016; 375(24):2359–2368. PMID: 27771985.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wrapping of an Ascending Aortic Aneurysm with the Multiple Boot-Straps Technique in a Patient Undergoing Off-Pump Coronary Artery Bypass Grafting
- Off-Pump Coronary Artery Bypass Grafting in Moyamoya Disease
- Anaortic Off-pump Coronary Artery Bypass Grafting in Patients with Takayasu's Arteritis
- "On-Pump" CABG on the Beating Heart: Two case report
- Successful Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm in a Patient with Severe Coronary Artery Disease Undergoing Off-Pump Coronary Artery Bypass Grafting