J Korean Med Sci.
2021 Jun;36(22):e161. 10.3346/jkms.2021.36.e161.
Clinical Features of Olfactory Dysfunction in COVID-19 Patients
- Affiliations
-
- 1Division of Rhinology, Department of Otorhinolaryngology-Head and Neck Surgery, Ansan, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Division of Infectious Diseases, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- KMID: 2516582
- DOI: http://doi.org/10.3346/jkms.2021.36.e161
Abstract
- Background
The aim of this study was to evaluate the subjective and objective olfactory function in coronavirus disease 2019 (COVID-19) patients and the effect of olfactory training.
Methods
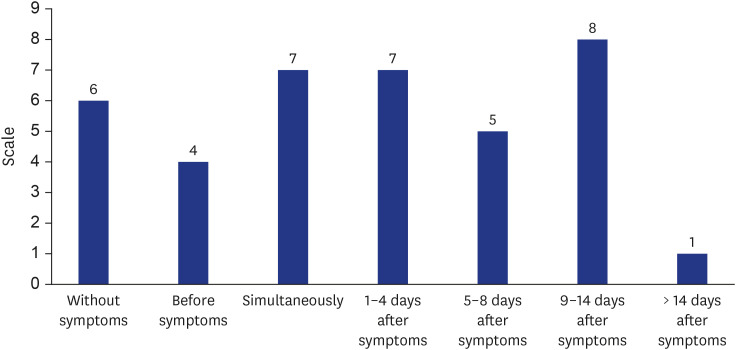
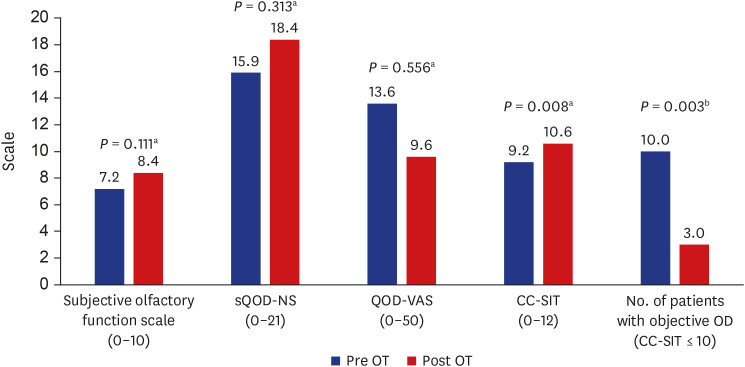
A prospective cohort study was performed in 53 patients who recovered from COVID-19 and visited our tertiary hospital. Subjective olfactory function was evaluated using the 11-point Likert scale (0–10) and the Korean version of the Questionnaire of Olfactory Disorders (QOD). Objective olfactory function was evaluated using Cross-Cultural Smell Identification Test (CC-SIT). Confirmed patients were followed up after 2 months of olfactory training.
Results
The median, interquartile range (Q1–Q3) score of subjective olfactory function significantly deteriorated in patients with olfactory dysfunction (OD) than in those without OD, even after 3 months of onset (11-point Likert scale, 8, 6–9 vs. 10, 10–10; short version of QOD-negative statements, 19, 16–21 vs. 21, 21–21; QOD-visual analogue scale, 7, 1–13 vs. 0, 0–0; all P < 0.001). However, the objective olfactory function was not significantly different between the two groups (median, interquartile range; 11, 9–11 vs. 11, 9–11, P = 0.887). The percentage of patients with objective hyposmia (CC-SIT ≤ 10) was also not significantly different (47.4% vs. 40%,P = 0.762). OD in COVID-19 was normalized after 2 months of olfactory training in 70% of patients even after 3 months of olfactory impairment.
Conclusion
Although subjective olfactory function is significantly decreased in the OD group, the objective olfactory function was not significantly different. Moreover, olfactory training is effective in COVID-19 patients with OD.
Keyword
Figure
Reference
-
1. World Health Organization. Coronavirus disease (COVID-19) pandemic. Updated 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.2. Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020; 382(22):2081–2090. PMID: 32329971.
Article3. Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020; 382(10):970–971. PMID: 32003551.
Article4. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.
Article5. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223):507–513. PMID: 32007143.
Article6. Borsetto D, Hopkins C, Philips V, Obholzer R, Tirelli G, Polesel J, et al. Self-reported alteration of sense of smell or taste in patients with COVID-19: a systematic review and meta-analysis on 3563 patients. Rhinology. 2020; 58(5):430–436. PMID: 32626853.
Article7. Cho RHW, To ZWH, Yeung ZWC, Tso EYK, Fung KSC, Chau SK, et al. COVID-19 viral load in the severity of and recovery from olfactory and gustatory dysfunction. Laryngoscope. 2020; 130(11):2680–2685. PMID: 32794209.8. Seo MY, Seok H, Hwang SJ, Choi HK, Jeon JH, Sohn JW, et al. Trend of olfactory and gustatory dysfunction in COVID-19 patients in a quarantine facility. J Korean Med Sci. 2020; 35(41):e375. PMID: 33107232.
Article9. Chiesa-Estomba CM, Lechien JR, Radulesco T, Michel J, Sowerby LJ, Hopkins C, et al. Patterns of smell recovery in 751 patients affected by the COVID-19 outbreak. Eur J Neurol. 2020; 27(11):2318–2321. PMID: 32677329.
Article10. Chary E, Carsuzaa F, Trijolet JP, Capitaine AL, Roncato-Saberan M, Fouet K, et al. Prevalence and recovery from olfactory and gustatory dysfunctions in COVID-19 infection: a prospective multicenter study. Am J Rhinol Allergy. 2020; 34(5):686–693. PMID: 32527141.
Article11. Hummel T, Rissom K, Reden J, Hähner A, Weidenbecher M, Hüttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009; 119(3):496–499. PMID: 19235739.
Article12. Damm M, Pikart LK, Reimann H, Burkert S, Göktas Ö, Haxel B, et al. Olfactory training is helpful in postinfectious olfactory loss: a randomized, controlled, multicenter study. Laryngoscope. 2014; 124(4):826–831. PMID: 23929687.
Article13. Doty RL, Marcus A, Lee WW. Development of the 12-item Cross-Cultural Smell Identification Test (CC-SIT). Laryngoscope. 1996; 106(3 Pt 1):353–356. PMID: 8614203.14. Choi WR, Jeong HY, Kim JH. Reliability and validity of the Korean version of the Questionnaire of Olfactory Disorders. Int Forum Allergy Rhinol. 2018; 8(12):1481–1485. PMID: 30039926.
Article15. Kim DW, Kim JY, Kim SW, Jeon SY. Postoperative olfactory results in chronic rhinosinusitis with nasal polyposis according to wound healing status. Clin Exp Otorhinolaryngol. 2013; 6(3):146–151. PMID: 24069517.
Article16. Kim BG, Kim BY, Shin JH, Kim SW, Kim SW. The effect of olfactory training using Korean version odorants: a preliminary study. Korean J Otorhinolaryngol-Head Neck Surg. 2018; 61(10):522–527.
Article17. Mastrangelo A, Bonato M, Cinque P. Smell and taste disorders in COVID-19: from pathogenesis to clinical features and outcomes. Neurosci Lett. 2021; 748:135694. PMID: 33600902.
Article18. Lv H, Zhang W, Zhu Z, Xiong Q, Xiang R, Wang Y, et al. Prevalence and recovery time of olfactory and gustatory dysfunction in hospitalized patients with COVID-19 in Wuhan, China. Int J Infect Dis. 2020; 100:507–512. PMID: 32950734.
Article19. Brandã Neto D, Fornazieri MA, Dib C, Di Francesco RC, Doty RL, Voegels RL, et al. Chemosensory dysfunction in COVID-19: prevalences, recovery rates, and clinical associations on a large Brazilian sample. Otolaryngol Head Neck Surg. 2021; 164(3):512–518. PMID: 32867582.
Article20. Kosugi EM, Lavinsky J, Romano FR, Fornazieri MA, Luz-Matsumoto GR, Lessa MM, et al. Incomplete and late recovery of sudden olfactory dysfunction in COVID-19. Braz J Otorhinolaryngol. 2020; 86(4):490–496. PMID: 32534982.
Article21. Le Bon SD, Konopnicki D, Pisarski N, Prunier L, Lechien JR, Horoi M. Efficacy and safety of oral corticosteroids and olfactory training in the management of COVID-19-related loss of smell. Eur Arch Otorhinolaryngol. Forthcoming. 2021.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contemporary Review of Olfactory Dysfunction in COVID-19
- A review on photobiomodulation therapy for olfactory dysfunction caused by COVID-19
- Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- Characteristics and Prognosis of COVID-19 Induced Olfactory and Gustatory Dysfunction in Daegu
- The Sniffing Bead System as a Useful Diagnostic Tool for Olfactory Dysfunction in COVID-19