J Korean Med Sci.
2021 May;36(21):e145. 10.3346/jkms.2021.36.e145.
Changing Trends in Liver Cirrhosis Etiology and Severity in Korea: the Increasing Impact of Alcohol
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Hospital School of Medicine, Gwangju, Korea
- 2Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea
- 4Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- 5Department of Internal Medicine, Hallym University College of Medicine, Chuncheon, Korea
- 6Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2516502
- DOI: http://doi.org/10.3346/jkms.2021.36.e145
Abstract
- Background
Chronic hepatitis B is the most common cause of liver cirrhosis in South Korea. However, alcoholic liver disease has shown an increasing trend. Although the clinical implications surrounding liver cirrhosis have been changing over the years, few studies have recently examined cirrhosis epidemiology. Therefore, we aimed to investigate changes in liver cirrhosis etiology and severity in Korea.
Methods
We retrospectively reviewed 16,888 records of cirrhotic patients from six tertiary hospitals in Korea from 2008 to 2017. Continuous and non-continuous variables were processed via linear and Poisson regression, expressed as beta (B) coefficients and as exponentiated values of coefficients (Exp[B]), respectively.
Results
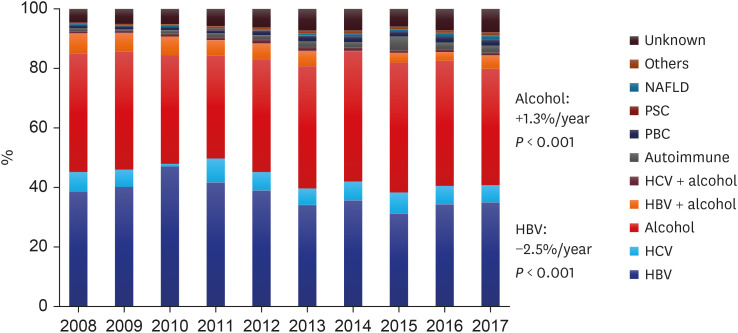
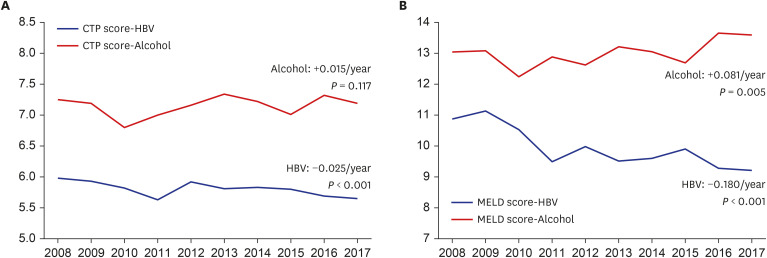
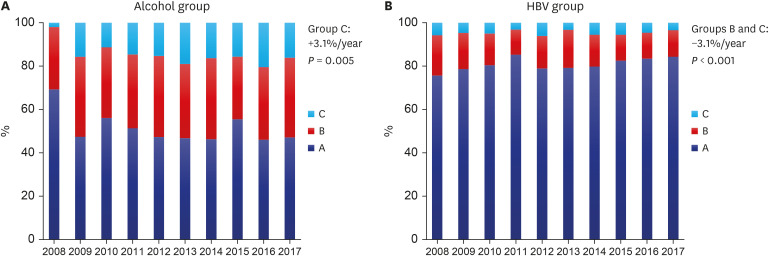
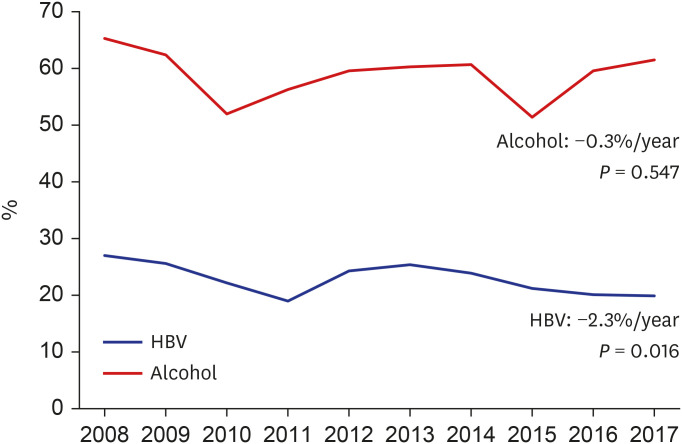
Chronic hepatitis B showed a decreasing trend (Exp[B] = 0.975, P < 0.001), whereas alcohol showed an increasing trend (Exp[B] = 1.013, P = 0.003), occupying the most common etiology in 2017. The Child-Turcotte-Pugh (CTP) score and decompensated liver cirrhosis prevalence did not change over the 10-year period. The incidence of variceal bleeding, severe ascites, hepatic encephalopathy, and spontaneous bacterial peritonitis significantly decreased from 12.3% to 7.7%, 7.8% to 4.1%, 1.0% to 0.5%, and 1.9% to 1.1%, respectively (P < 0.05 for all). In the subgroup analysis, the chronic hepatitis B group showed improving CTP scores (B = −0.025, P < 0.001) and decreasing decompensated liver cirrhosis rates (Exp[B] = 0.977, P = 0.016), whereas the alcohol group demonstrated increasing CTP class C (Exp[B] = 1.031, P = 0.005) and model for end-stage liver disease scores (B = 0.081, P = 0.005) over 10 years.
Conclusion
The chronic hepatitis B group exhibited improved results, whereas the alcohol group still presented poor liver functions and outcomes. Future national policies and systematic approaches addressing the incidence, prevention, and treatment of alcoholic liver cirrhosis are indispensable.
Keyword
Figure
Reference
-
1. Cho EJ, Kim SE, Suk KT, An J, Jeong SW, Chung WJ, et al. Current status and strategies for hepatitis B control in Korea. Clin Mol Hepatol. 2017; 23(3):205–211. PMID: 28942624.
Article2. Yoon JH, Jun CH, Seo JH, Cho HA, Cho SB, Choi SK, et al. Sofosbuvir plus ribavirin for the treatment of hepatitis C virus genotype 2 in Korea: what's the optimal dosage of ribavirin in real-world setting? J Dig Dis. 2019; 20(1):31–37. PMID: 30548199.
Article3. Lee YJ, Heo J, Kim DY, Chung WJ, Tak WY, Kim YJ, et al. An integrated analysis of elbasvir/grazoprevir in Korean patients with hepatitis C virus genotype 1b infection. Clin Mol Hepatol. 2019; 25(4):400–407. PMID: 31132846.
Article4. World Health Organization. Global Information System on Alcohol and Health (GISAH): levels of consumption. Global Health Observatory (GHO) data. Updated 2018. Accessed September 21, 2018. https://www.who.int/gho/alcohol/consumption_levels/en/.5. Jang JW. Current status of liver diseases in Korea: liver cirrhosis. Korean J Hepatol. 2009; 15(Suppl 6):S40–S49. PMID: 20037279.
Article6. Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol. 2017; 67(4):862–873. PMID: 28642059.
Article7. Park SH, Plank LD, Suk KT, Park YE, Lee J, Choi JH, et al. Trends in the prevalence of chronic liver disease in the Korean adult population, 1998–2017. Clin Mol Hepatol. 2020; 26(2):209–215. PMID: 31679316.
Article8. Schramm C, Lohse AW. Autoimmune hepatitis on the rise. J Hepatol. 2014; 60(3):478–479. PMID: 24295874.
Article9. Lu M, Zhou Y, Haller IV, Romanelli RJ, VanWormer JJ, Rodriguez CV, et al. Increasing prevalence of primary biliary cholangitis and reduced mortality with treatment. Clin Gastroenterol Hepatol. 2018; 16(8):1342–1350.e1. PMID: 29277621.
Article10. Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964; 1:1–85. PMID: 4950264.11. Runyon BA; AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009; 49(6):2087–2107. PMID: 19475696.
Article12. Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for liver cirrhosis: ascites and related complications. Clin Mol Hepatol. 2018; 24(3):230–277. PMID: 29991196.13. Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for liver cirrhosis: varices, hepatic encephalopathy, and related complications. Clin Mol Hepatol. 2020; 26(2):83–127. PMID: 31918536.14. Yim SY, Kim JH. The epidemiology of hepatitis B virus infection in Korea. Korean J Intern Med. 2019; 34(5):945–953. PMID: 30919608.
Article15. Hosaka T, Suzuki F, Kobayashi M, Seko Y, Kawamura Y, Sezaki H, et al. Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virus infection. Hepatology. 2013; 58(1):98–107. PMID: 23213040.
Article16. Wong GL, Chan HL, Mak CW, Lee SK, Ip ZM, Lam AT, et al. Entecavir treatment reduces hepatic events and deaths in chronic hepatitis B patients with liver cirrhosis. Hepatology. 2013; 58(5):1537–1547. PMID: 23389810.
Article17. Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol. 2017; 23(47):8263–8276. PMID: 29307986.
Article18. Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019; 71(4):793–801. PMID: 31279902.
Article19. Jeong SH. Current epidemiology and clinical characteristics of autoimmune liver diseases in South Korea. Clin Mol Hepatol. 2018; 24(1):10–19. PMID: 29307132.
Article20. Kim BH, Choi HY, Ki M, Kim KA, Jang ES, Jeong SH. Population-based prevalence, incidence, and disease burden of autoimmune hepatitis in South Korea. PLoS One. 2017; 12(8):e0182391. PMID: 28771543.
Article21. Jang JW. Current status of liver diseases in Korea: liver cirrhosis. Korean J Hepatol. 2009; 15(Suppl 6):S40–9. PMID: 20037279.
Article22. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018; 14(2):88–98. PMID: 29219149.
Article23. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018; 67(1):123–133. PMID: 28802062.
Article24. Fleming KM, Aithal GP, Card TR, West J. The rate of decompensation and clinical progression of disease in people with cirrhosis: a cohort study. Aliment Pharmacol Ther. 2010; 32(11-12):1343–1350. PMID: 21050236.
Article25. Samonakis DN, Koulentaki M, Coucoutsi C, Augoustaki A, Baritaki C, Digenakis E, et al. Clinical outcomes of compensated and decompensated cirrhosis: a long term study. World J Hepatol. 2014; 6(7):504–512. PMID: 25068002.26. Yatsuhashi H, Ohnishi Y, Nakayama S, Iwase H, Nakamura T, Imawari M. Anti-hypoalbuminemic effect of branched-chain amino acid granules in patients with liver cirrhosis is independent of dietary energy and protein intake. Hepatol Res. 2011; 41(11):1027–1035. PMID: 21951974.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Cause and Complication of Liver Cirrhosis during the Reccent 5 Years
- Nutritional Status in Alcohol- and Virus-Related Liver Cirrhosis
- Clinical Usefulness of Corrected QT Interval As an Index of the Severity in Liver Cirrhosis
- Epidemiology of Alcoholic Liver Disease in Korea
- Family Support, Alcohol Consumption and Drinking Motives in Patients with Liver Cirrhosis