Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):251-258. 10.14701/ahbps.2021.25.2.251.
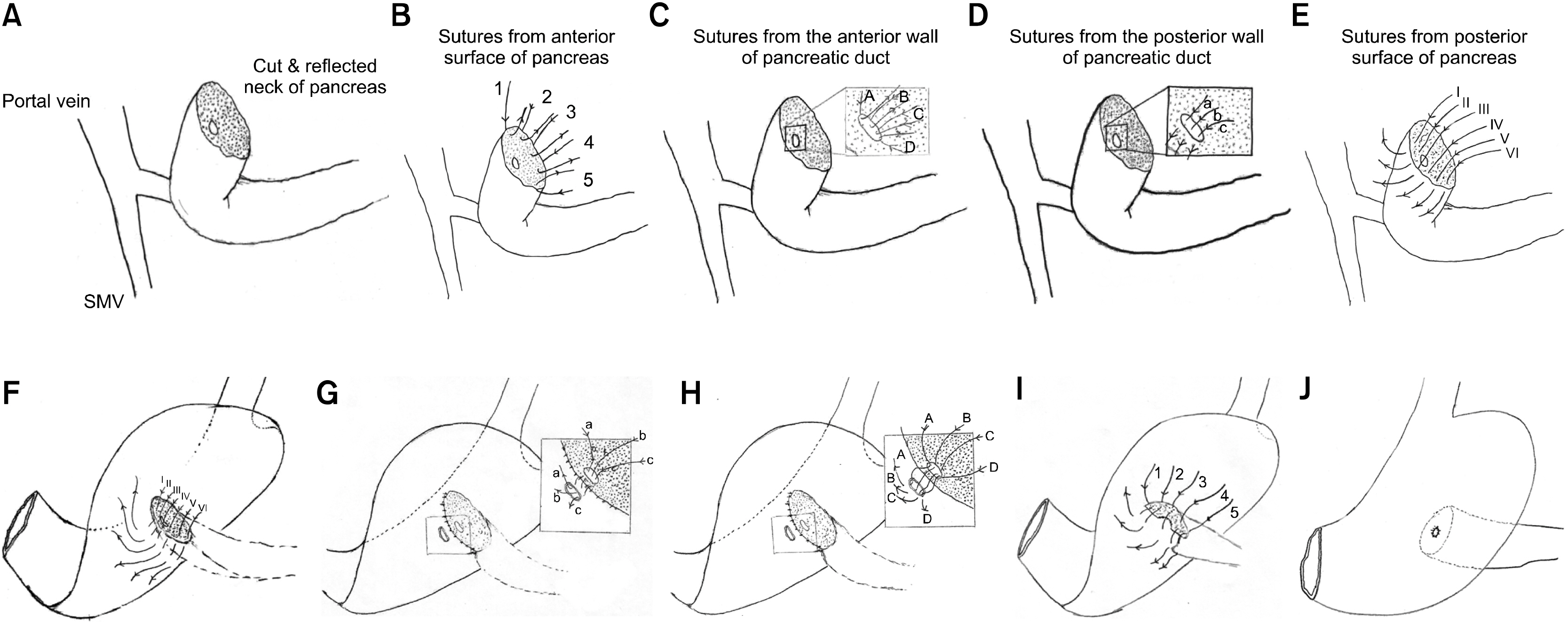
Clinical outcomes and technical description of unstented end to side pancreaticogastrostomy by small posterior gastrotomy
- Affiliations
-
- 1Department of Surgical Oncology, All India Institute of Medical Science, New Delhi, India
- KMID: 2516246
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.251
Abstract
- Backgrounds/Aims
Morbidity following Whipple’s surgery largely depends upon the pancreatic stump anastomosis leak. Pancreaticogastrostomy is one of the techniques of pancreatic stump reconstruction and is described variously in the literature. Duct to mucosa pancreaticogastrostomy is described either by a large 3-4 cm posterior gastrotomy or by small gastrotomy of 2-3 mm with the use of internal stents along with. We describe clinical outcomes and technique of 2 layer end to side pancreatico-gastrostomy by a small posterior gastrotomy without the use of internal stents.
Methods
Hospital records of 35 patients where the technique of, small posterior gastrotomy end to side duct to mucosa pancreatico-gastrostomy without internal stents, was used for pancreatic stump reconstruction were studied retrospectively. The data were analyzed for demographic details, stage of the disease, and short term outcomes related to surgical procedure.
Results
The mean duration of surgery was 7.4 hours. Grade A, B, and C POPF were observed in 10 (28.5%), 3 (8.5%), and 1 (2.8%) of patients respectively. The mean time to remove pancreatic drain was 9 days, and the mean time to start oral feeds was 8.9 days. The mean hospital stay was 12.9 days (07-26). Thirty days mortality was 2.8%.
Conclusions
Unstented duct to mucosa end to side pancreatico-gastrostomy technique is comparable with other pancreatico-gastrostomy techniques in outcomes in terms of POPF, morbidity, mortality, and hospital stay. However, to establish the superiority or inferiority of this technique, a larger study is recommended.
Figure
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. 2018; Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 68:394–424. DOI: 10.3322/caac.21492. PMID: 30207593.
Article2. Rawla P, Barsouk A. 2019; Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol. 14:26–38. DOI: 10.5114/pg.2018.80001. PMID: 30944675. PMCID: PMC6444111.
Article3. Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, et al. 2013; Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol. 14:655–662. DOI: 10.1016/S1470-2045(13)70126-8.
Article4. Pulvirenti A, Ramera M, Bassi C. 2017; Modifications in the International Study Group for Pancreatic Surgery (ISGPS) definition of postoperative pancreatic fistula. Transl Gastroenterol Hepatol. 2:107. DOI: 10.21037/tgh.2017.11.14. PMID: 29354764. PMCID: PMC5763010.
Article5. Chan C, Franssen B, Rubio A, Uscanga L. 2008; Pancreaticoduodenectomy in a Latin American country: the transition to a high-volume center. J Gastrointest Surg. 12:527–533. DOI: 10.1007/s11605-007-0274-0. PMID: 17763915.
Article6. Waugh JM, Clagett OT. 1946; Resection of the duodenum and head of the pancreas for carcinoma; an analysis of thirty cases. Surgery. 20:224–232.7. Costa RM, Lucas L. 2016; Ten years experience with 150 pancreaticoduodenectomy with pancreaticoenteric reconstruction using sleeve pancreaticogastrostomy (Montenegro's binding technique). HPB. 18:e434. DOI: 10.1016/j.hpb.2016.03.138.
Article8. Zhao Y, Zhang J, Lan Z, Jiang Q, Zhang S, Chu Y, et al. 2017; Are internal or external pancreatic duct stents the preferred choice for patients undergoing pancreaticoduodenectomy? A meta-analysis. Biomed Res Int. 2017:1367238. DOI: 10.1155/2017/1367238. PMID: 28466004. PMCID: PMC5390541.
Article9. Langrehr JM, Bahra M, Jacob D, Glanemann M, Neuhaus P. 2005; Prospective randomized comparison between a new mattress technique and Cattell (duct-to-mucosa) pancreaticojejunostomy for pancreatic resection. World J Surg. 29:1111–1119. discussion 1120–1121. DOI: 10.1007/s00268-005-7875-0. PMID: 16091984.
Article10. Payne RF, Pain JA. 2006; Duct-to-mucosa pancreaticogastrostomy is a safe anastomosis following pancreaticoduodenectomy. Br J Surg. 93:73–77. DOI: 10.1002/bjs.5191. PMID: 16273533.
Article11. Fang WL, Shyr YM, Su CH, Chen TH, Wu CW, Lui WY. 2007; Comparison between pancreaticojejunostomy and pancreaticogastrostomy after pancreaticoduodenectomy. J Formos Med Assoc. 106:717–727. DOI: 10.1016/S0929-6646(08)60033-9.
Article12. Aranha GV, Hodul P, Golts E, Oh D, Pickleman J, Creech S. 2003; A comparison of pancreaticogastrostomy and pancreaticojejunostomy following pancreaticoduodenectomy. J Gastrointest Surg. 7:672–682. DOI: 10.1016/S1091-255X(02)00432-8.
Article13. El Nakeeb A, Hamdy E, Sultan AM, Salah T, Askr W, Ezzat H, et al. 2014; Isolated Roux loop pancreaticojejunostomy versus pancreaticogastrostomy after pancreaticoduodenectomy: a prospective randomized study. HPB (Oxford). 16:713–722. DOI: 10.1111/hpb.12210. PMID: 24467711. PMCID: PMC4113253.
Article14. Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, et al. 1995; A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 222:580–588. discussion 588–592. DOI: 10.1097/00000658-199510000-00014. PMID: 7574936. PMCID: PMC1234894.
Article15. Yap PY, Hwang JS, Bong JJ. 2018; A modified technique of pancreaticogastrostomy with short internal stent: a single surgeon's experience. Asian J Surg. 41:250–256. DOI: 10.1016/j.asjsur.2017.01.003. PMID: 28286020.
Article16. Fernández-Cruz L, Cosa R, Blanco L, López-Boado MA, Astudillo E. 2008; Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 248:930–938. DOI: 10.1097/SLA.0b013e31818fefc7. PMID: 19092337.17. Keck T, Wellner UF, Bahra M, Klein F, Sick O, Niedergethmann M, et al. 2016; Pancreatogastrostomy versus pancreatojejunostomy for RECOnstruction after PANCreatoduodenectomy (RECOPANC, DRKS 00000767): perioperative and long-term results of a multicenter randomized controlled trial. Ann Surg. 263:440–449. DOI: 10.1097/SLA.0000000000001240. PMID: 26135690. PMCID: PMC4741417.18. Duffas JP, Suc B, Msika S, Fourtanier G, Muscari F, Hay JM, et al. 2005; A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg. 189:720–729. DOI: 10.1016/j.amjsurg.2005.03.015. PMID: 15910726.
Article19. Topal B, Fieuws S. 2013; Pancreaticogastrostomy after pancreaticoduodenectomy? Lancet Oncol. 14:e340–e341. DOI: 10.1016/S1470-2045(13)70282-1.
Article20. Wellner UF, Sick O, Olschewski M, Adam U, Hopt UT, Keck T. 2012; Randomized controlled single-center trial comparing pancreatogastrostomy versus pancreaticojejunostomy after partial pancreatoduodenectomy. J Gastrointest Surg. 16:1686–1695. DOI: 10.1007/s11605-012-1940-4. PMID: 22744638.
Article21. Figueras J, Sabater L, Planellas P, Muñoz-Forner E, Lopez-Ben S, Falgueras L, et al. 2013; Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg. 100:1597–1605. DOI: 10.1002/bjs.9252. PMID: 24264781.
Article22. Bassi C, Falconi M, Molinari E, Salvia R, Butturini G, Sartori N, et al. 2005; Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg. 242:767–771. discussion 771–773. DOI: 10.1097/01.sla.0000189124.47589.6d. PMID: 16327486. PMCID: PMC1409871.23. Price LH, Brandabur JJ, Kozarek RA, Gluck M, Traverso WL, Irani S. 2009; Good stents gone bad: endoscopic treatment of proximally migrated pancreatic duct stents. Gastrointest Endosc. 70:174–179. DOI: 10.1016/j.gie.2008.12.051. PMID: 19559842.
Article24. Ortega PM, Zozaya-Larequi G, Arredondo J, Martí-Cruchaga P, Bellver M, Sánchez-Justicia C, et al. 2015; Distal migration of a transanastomotic pancreatic stent resulting in bowel perforation 19 years after pancreatoduodenectomy: report of a case. Surg Today. 45:374–377. DOI: 10.1007/s00595-014-0897-1. PMID: 24752691.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An easy and secure pancreaticogastrostomy after pancreaticoduodenectomy: transpancreatic suture with a buttress method through an anterior gastrotomy
- Pancreaticogastrostomy as a Beneficial Alternative to a Pancreaticojejunostomy
- A Case of a Traumatic Pancreatic Neck Transection Treated with a Binding Pancreaticogastrostomy
- A Stduy on the Standardization of the Description of Orthopedic Diseases for Electroic Data Processing System (EDPS)
- Two cases of primary urethral end to end anastomosis for posterior urethral rupture