Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):215-220. 10.14701/ahbps.2021.25.2.215.
Clinicopathological correlation and post-resection outcomes of hepatic angiomyolipoma
- Affiliations
-
- 1Departments of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Departments of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2516242
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.215
Abstract
- Backgrounds/Aims
Angiomyolipoma is a rare neoplasm of mesenchymal origin derived from perivascular epithelioid cells. Due to rarity, hepatic angiomyolipoma (HAML) has been often misdiagnosed as hepatocellular carcinoma (HCC) or other hypervascular liver tumors based on imaging studies. This study investigated the clinicopathological correlation and post-resection outcomes of HAML.
Methods
This retrospective observational study included 40 patients who underwent hepatic resection (HR) for HAML between 2008 and 2018.
Results
Mean age of the patients was 42.6±11.4 years and there were 30 (75.0%) females. Hepatitis B and C virus infection was present in 8 patients (20.0%) and 1 patient (2.5%), respectively. Preoperative diagnoses on imaging studies were HCC in 23 (57.5%) patients, HAML in 14 (35.0%) patients, focal nodular hyperplasia in 2 (5.0%) patients, and hepatic adenoma in 1 (2.5%) patient. Percutaneous liver biopsy was performed in 10 (25.0%) patients and HAML was diagnosed in all patients. Only 3 patients (7.5%) showed a slight elevation in the level of liver tumor markers. Major HR was performed in 10 (25.0%). Laparoscopic HR was performed in 9 (22.5%). The mean tumor size was 4.8±3.9 cm and single tumor was present in 38 (95.0%) patients. Currently, all the patients are alive without tumor recurrence during the follow-up observation period of 75.7±37.3 months.
Conclusions
HAML is a rare form of primary liver tumor and is often misdiagnosed as HCC or other hypervascular tumors. Although HAML is benign in nature, it has malignant potential, thus resection is indicated if the tumor grows or malignancy cannot be excluded.
Keyword
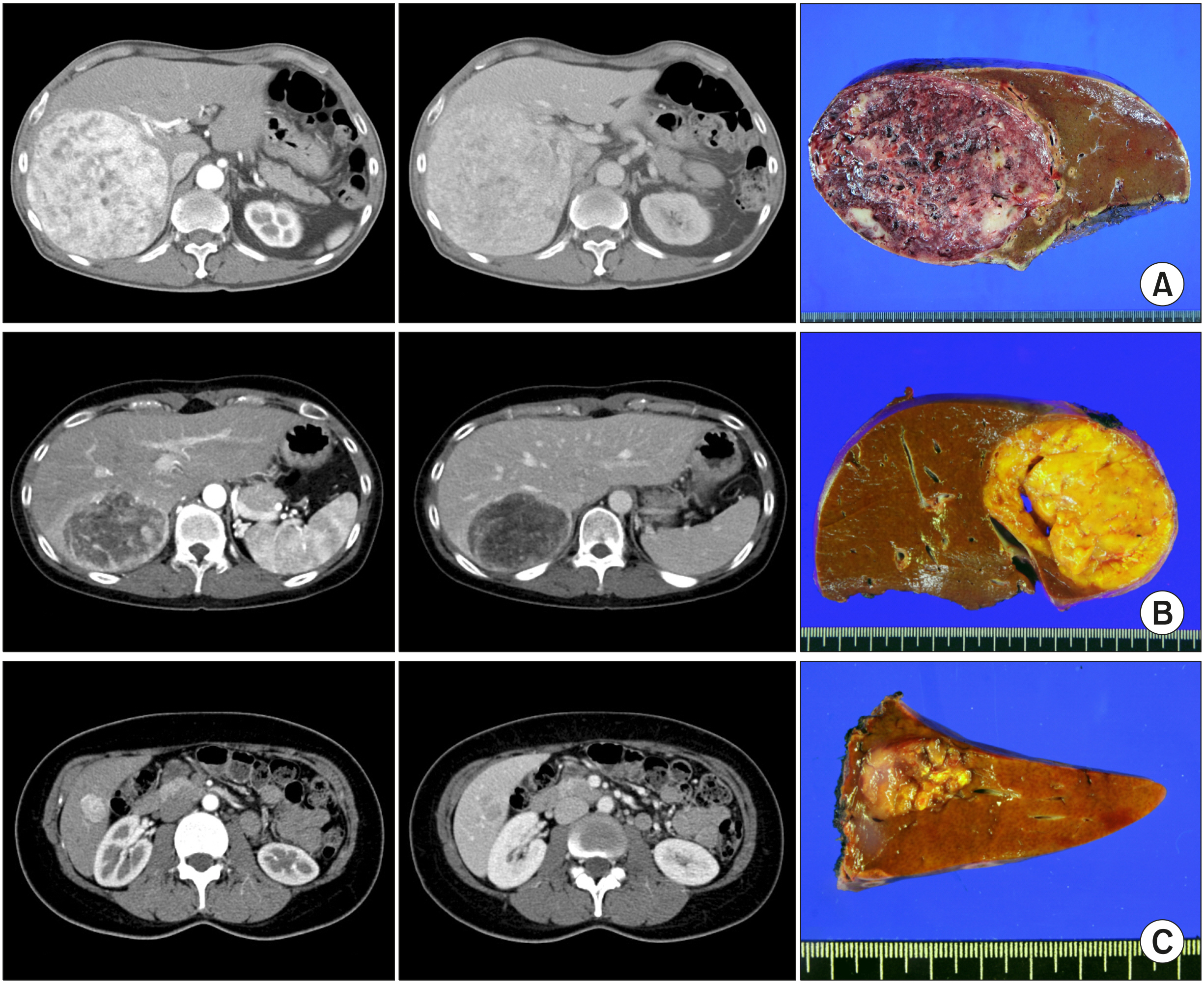
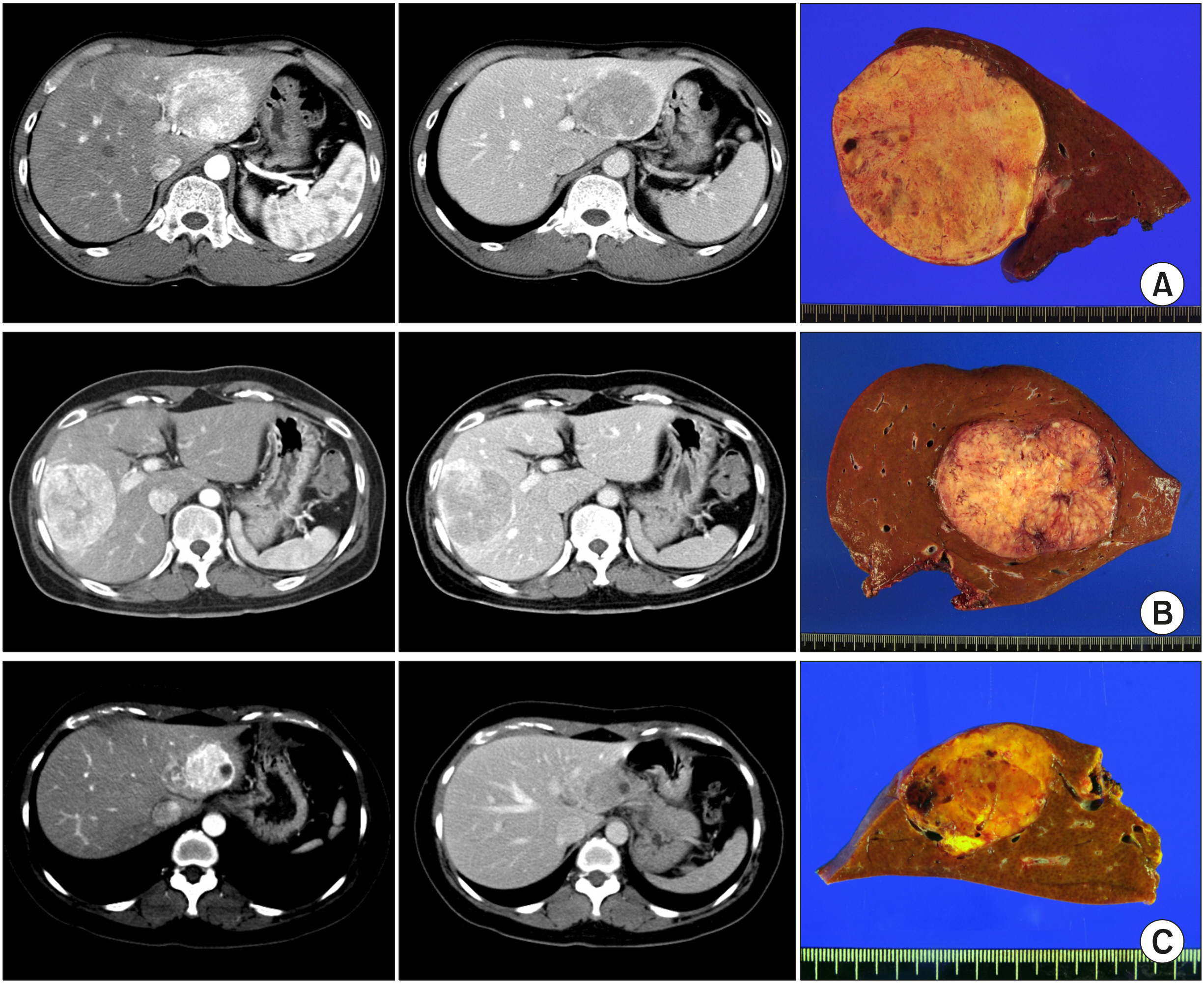
Figure
Reference
-
1. Martignoni G, Pea M, Reghellin D, Zamboni G, Bonetti F. 2008; PEComas: the past, the present and the future. Virchows Arch. 452:119–132. DOI: 10.1007/s00428-007-0509-1. PMID: 18080139. PMCID: PMC2234444.
Article2. Ameurtesse H, Chbani L, Bennani A, Toughrai I, Beggui N, Kamaoui I, et al. 2014; Primary perivascular epithelioid cell tumor of the liver: new case report and literature review. Diagn Pathol. 9:149. DOI: 10.1186/1746-1596-9-149. PMID: 25034830. PMCID: PMC4223599.
Article3. Ortiz S, Tortosa F. 2016; Epithelioid angiomyolipoma of the liver: clinicopathological correlation in a series of 4 cases. Rev Esp Enferm Dig. 108:27–30. DOI: 10.17235/reed.2015.3947/2015. PMID: 26765232.
Article4. Chang Z, Zhang JM, Ying JQ, Ge YP. 2011; Characteristics and treatment strategy of hepatic angiomyolipoma: a series of 94 patients collected from four institutions. J Gastrointestin Liver Dis. 20:65–69.5. Shi H, Cao D, Wei L, Sun L, Guo A. 2010; Inflammatory angiomyolipomas of the liver: a clinicopathologic and immunohistochemical analysis of 5 cases. Ann Diagn Pathol. 14:240–246. DOI: 10.1016/j.anndiagpath.2010.03.002. PMID: 20637427.
Article6. Jung DH, Hwang S, Hong SM, Kim KH, Ahn CS, Moon DB, et al. 2018; Clinico-pathological correlation of hepatic angiomyolipoma: a series of 23 resection cases. ANZ J Surg. 88:E60–E65. DOI: 10.1111/ans.13880. PMID: 28122404.
Article7. Lencioni R. 2010; Surveillance and early diagnosis of hepatocellular carcinoma. Dig Liver Dis. 42 Suppl 3:S223–S227. DOI: 10.1016/S1590-8658(10)60509-9.
Article8. Cho HD, Hwang S, Lee YJ, Park KM, Kim KH, Kim JC, et al. 2016; Changes in the types of liver diseases requiring hepatic resection: a single-institution experience of 9016 cases over a 10-year period. Korean J Hepatobiliary Pancreat Surg. 20:49–52. DOI: 10.14701/kjhbps.2016.20.2.49. PMID: 27212990. PMCID: PMC4874044.
Article9. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. 2015; Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 19:1305–1314. DOI: 10.1007/s11605-015-2846-8. PMID: 25947549.
Article10. Lee SG, Hwang S. 2005; How I do it: assessment of hepatic functional reserve for indication of hepatic resection. J Hepatobiliary Pancreat Surg. 12:38–43. DOI: 10.1007/s00534-004-0949-9. PMID: 15754098.
Article11. Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, Ha TY, et al. 2015; The impact of tumor size on long-term survival outcomes after resection of solitary hepatocellular carcinoma: single-institution experience with 2558 patients. J Gastrointest Surg. 19:1281–1290. DOI: 10.1007/s11605-015-2849-5. PMID: 25956724.
Article12. Hwang S, Lee YJ, Song GW, Park KM, Kim KH, Ahn CS, et al. 2015; Prognostic impact of tumor growth type on 7th AJCC staging system for intrahepatic cholangiocarcinoma: a single-center experience of 659 cases. J Gastrointest Surg. 19:1291–1304. DOI: 10.1007/s11605-015-2803-6. PMID: 25820487.
Article13. Yoon YI, Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, et al. 2016; Postresection outcomes of combined hepatocellular carcinoma-cholangiocarcinoma, hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Gastrointest Surg. 20:411–420. DOI: 10.1007/s11605-015-3045-3. PMID: 26628072.
Article14. Miettinen M, Fletcher CD, Kindblom LG, Zimmermann A, Tsui WMS. Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. 2010. Mesenchymal tumours of the liver. WHO classification of tumours of the digestive system. 4th ed. International Agency for Research on Cancer;Lyon: p. 241–250.15. Ji JS, Lu CY, Wang ZF, Xu M, Song JJ. 2013; Epithelioid angiomyolipoma of the liver: CT and MRI features. Abdom Imaging. 38:309–314. DOI: 10.1007/s00261-012-9911-5. PMID: 22610058. PMCID: PMC3594823.
Article16. Tryggvason G, Blöndal S, Goldin RD, Albrechtsen J, Björnsson J, Jónasson JG. 2004; Epithelioid angiomyolipoma of the liver: case report and review of the literature. APMIS. 112:612–616. DOI: 10.1111/j.1600-0463.2004.apm1120909.x. PMID: 15601311.
Article17. Xu PJ, Shan Y, Yan FH, Ji Y, Ding Y, Zhou ML. 2009; Epithelioid angiomyolipoma of the liver: cross-sectional imaging findings of 10 immunohistochemically-verified cases. World J Gastroenterol. 15:4576–4581. DOI: 10.3748/wjg.15.4576. PMID: 19777618. PMCID: PMC2752004.
Article18. Xiao W, Zhou M, Lou H, Wang Z, Zhang M. 2010; Hemodynamic characterization of hepatic angiomyolipoma with least amount of fat evaluated by contrast-enhanced magnetic resonance angiography. Abdom Imaging. 35:203–207. DOI: 10.1007/s00261-009-9508-9. PMID: 19319591.
Article19. Agaimy A, Vassos N, Croner RS, Strobel D, Lell M. 2012; Hepatic angiomyolipoma: a series of six cases with emphasis on pathological-radiological correlations and unusual variants diagnosed by core needle biopsy. Int J Clin Exp Pathol. 5:512–521.20. Bleeker JS, Quevedo JF, Folpe AL. 2012; "Malignant" perivascular epithelioid cell neoplasm: risk stratification and treatment strategies. Sarcoma. 2012:541626. DOI: 10.1155/2012/541626. PMID: 22619565. PMCID: PMC3350998.
Article21. Mizuguchi T, Katsuramaki T, Nobuoka T, Nishikage A, Oshima H, Kawasaki H, et al. 2004; Growth of hepatic angiomyolipoma indicating malignant potential. J Gastroenterol Hepatol. 19:1328–1330. DOI: 10.1111/j.1440-1746.2004.03583.x. PMID: 15482547.
Article22. Deng YF, Lin Q, Zhang SH, Ling YM, He JK, Chen XF. 2008; Malignant angiomyolipoma in the liver: a case report with pathological and molecular analysis. Pathol Res Pract. 204:911–918. DOI: 10.1016/j.prp.2008.06.007. PMID: 18723294.
Article23. Wang WT, Li ZQ, Zhang GH, Guo Y, Teng MJ. 2015; Liver transplantation for recurrent posthepatectomy malignant hepatic angiomyolipoma: a case report. World J Gastroenterol. 21:3755–3758. DOI: 10.3748/wjg.v21.i12.3755. PMID: 25834347. PMCID: PMC4375604.
Article24. Fukuda Y, Omiya H, Takami K, Mori K, Kodama Y, Mano M, et al. 2016; Malignant hepatic epithelioid angiomyolipoma with recurrence in the lung 7 years after hepatectomy: a case report and literature review. Surg Case Rep. 2:31. DOI: 10.1186/s40792-016-0158-1. PMID: 27037804. PMCID: PMC4818648.
Article25. Occhionorelli S, Dellachiesa L, Stano R, Cappellari L, Tartarini D, Severi S, et al. 2013; Spontaneous rupture of a hepatic epithelioid angiomyolipoma: damage control surgery. A case report. G Chir. 34:320–322.26. Brimo F, Robinson B, Guo C, Zhou M, Latour M, Epstein JI. 2010; Renal epithelioid angiomyolipoma with atypia: a series of 40 cases with emphasis on clinicopathologic prognostic indicators of malignancy. Am J Surg Pathol. 34:715–722. DOI: 10.1097/PAS.0b013e3181d90370. PMID: 20410812.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hepatic Angiomyolipoma Showing Different Uptake on F-18 FDG and C-11 Acetate PET
- Epithelioid Angiomyolipoma of the Kidney with Distant Metastasis
- Huge Hepatic Angiomyolipoma Mimicking Low Grade Hepatocellular Carcinoma
- Diagnosis and surgical treatment of a rare hepatic angiomyolipoma with internal hemorrhage
- A case of spontaneous rupture of hepatic angiomyolipoma