Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):192-197. 10.14701/ahbps.2021.25.2.192.
Comparison of skeletal muscle index-based formula and body surface area-based formula for calculating standard liver volume
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2516239
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.192
Abstract
- Backgrounds/Aims
Formula-derived standard liver volume (SLV) has been clinically used for living donor liver transplantation and hepatic resection. The majority of currently available SLV formulae are based on body surface are (BSA). However, they often show a wide range of error. Skeletal muscle index measured at the third lumbar vertebra level (L3SMI) appears to reflect lean body mass. The objective of this study was to compare the accuracy of L3SMI-based formula and BSA-based formula for calculating SLV.
Methods
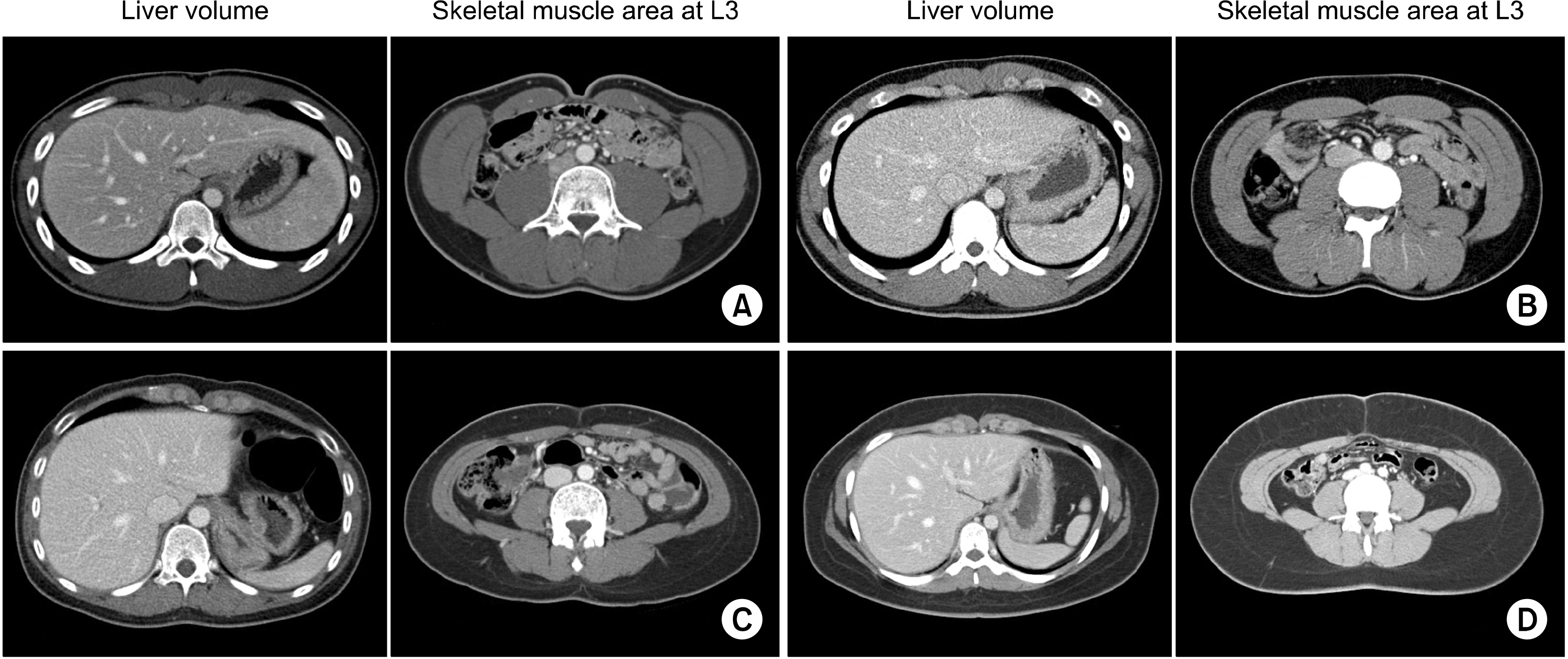
The study cohort was 500 hundred living liver donors who underwent surgery between January 2010 and December 2013. Computed tomography images were used for liver volumetry and skeletal muscle area measurement.
Results
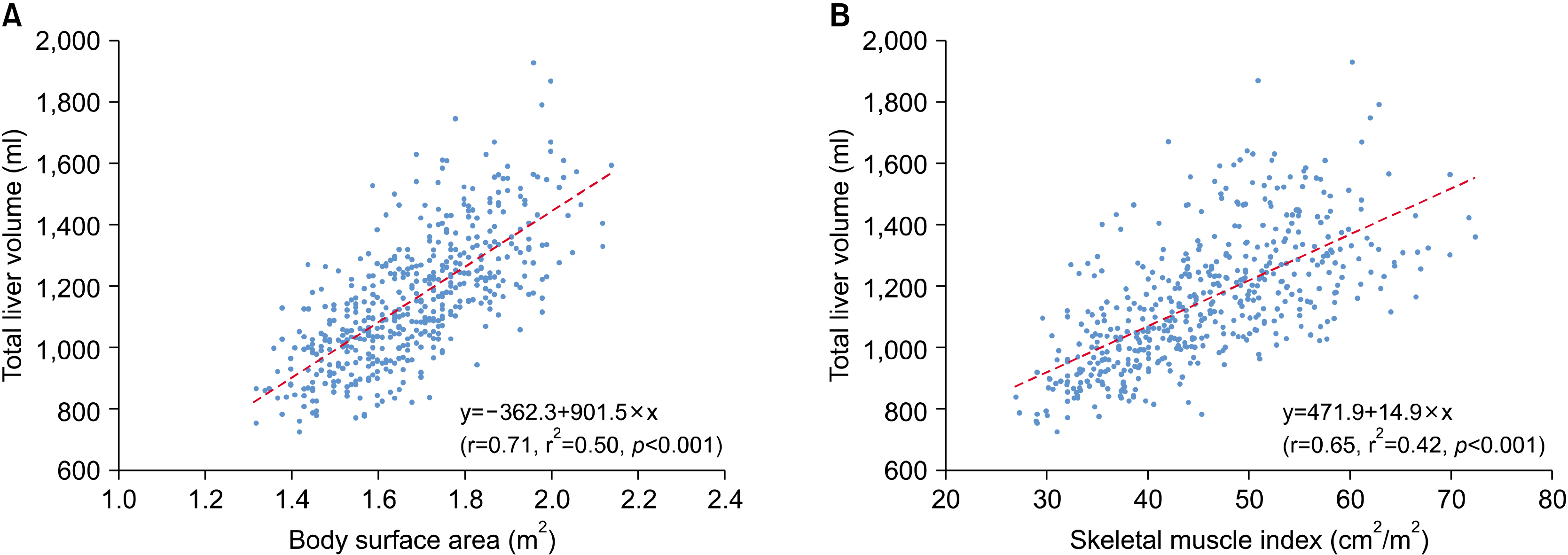
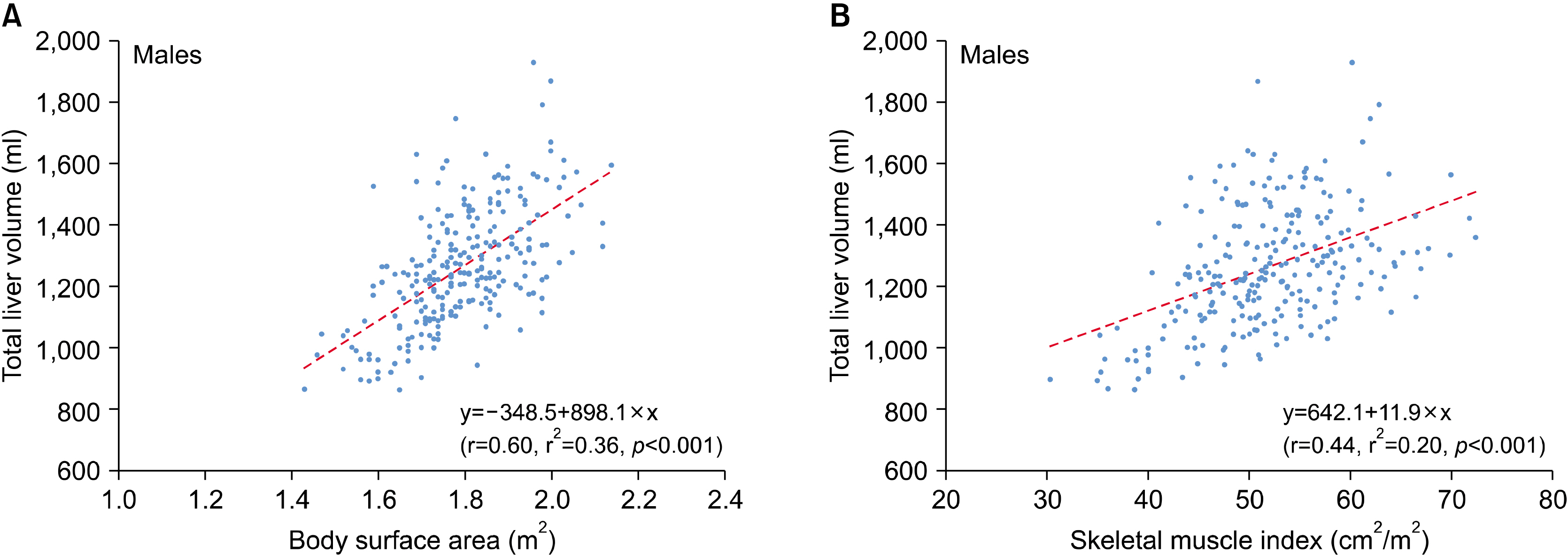
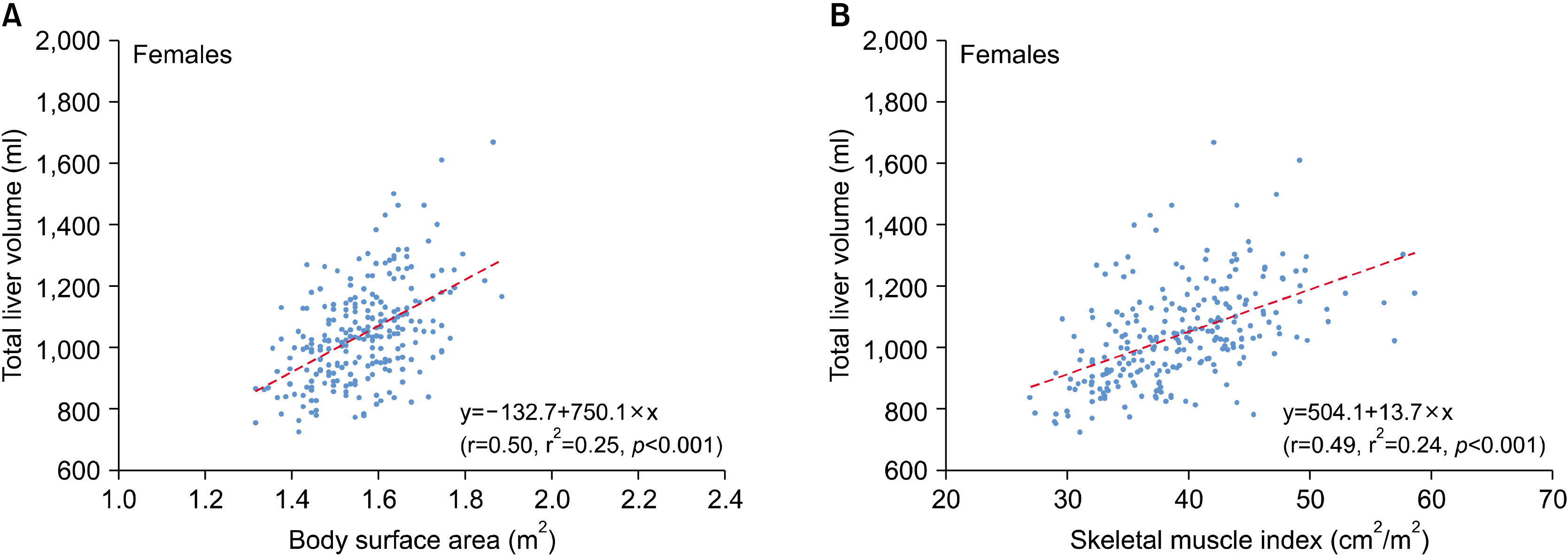
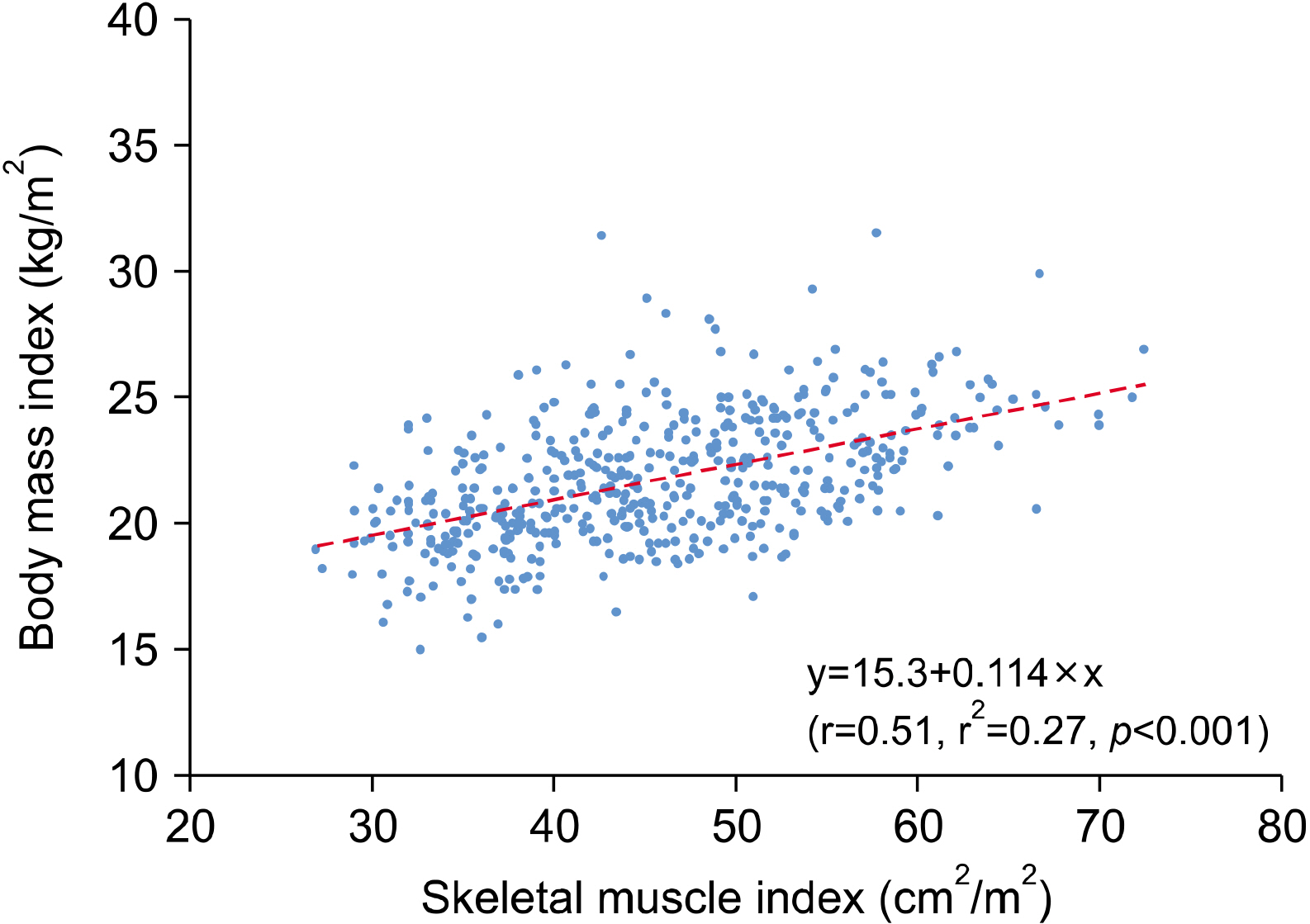
The study cohort included 250 male and 250 female donors. Their age, BSA, L3SMI, and body mass index were 26.8±8.7 years, 1.68±0.16 m2 , 45.6±9.0 cm2 /m2 , and 21.7±2.5 kg/m2 , respectively. The BSA-based SLV formula was “SLV (ml)=−362.3+901.5×BSA (m2 ) (r=0.71, r2 =0.50, p<0.001)”. The L3SMI-based SLV formula was “SLV (ml)=471.9+14.9×L3SMI (cm2 /m2 ) (r=0.65, r2 =0.42, p<0.001)”. Correlation coefficients were similar in subgroup analyses with 250 male donors and 250 female donors. There was a crude correlation between L3SMI and body mass index (r=0.51, r2 =0.27, p<0.001).
Conclusions
The results of this study suggest that SLV calculation with L3SMI-based formula does not appear to be superior to the currently available BSA-based formulae.
Keyword
Figure
Reference
-
1. Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, et al. 1995; Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 21:1317–1321. DOI: 10.1002/hep.1840210515. PMID: 7737637.
Article2. Pomposelli JJ, Tongyoo A, Wald C, Pomfret EA. 2012; Variability of standard liver volume estimation versus software-assisted total liver volume measurement. Liver Transpl. 18:1083–1092. DOI: 10.1002/lt.23461. PMID: 22532341.
Article3. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. 2015; Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 19:1305–1314. DOI: 10.1007/s11605-015-2846-8. PMID: 25947549.
Article4. Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. 2011; Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 12:489–495. DOI: 10.1016/S1470-2045(10)70218-7.
Article5. Montano-Loza AJ, Meza-Junco J, Baracos VE, Prado CM, Ma M, Meeberg G, et al. 2014; Severe muscle depletion predicts postoperative length of stay but is not associated with survival after liver transplantation. Liver Transpl. 20:640–648. DOI: 10.1002/lt.23863. PMID: 24678005.
Article6. Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. 2004; Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol (1985). 97:2333–2338. DOI: 10.1152/japplphysiol.00744.2004. PMID: 15310748.
Article7. Golse N, Bucur PO, Ciacio O, Pittau G, Sa Cunha A, Adam R, et al. 2017; A new definition of sarcopenia in patients with cirrhosis undergoing liver transplantation. Liver Transpl. 23:143–154. DOI: 10.1002/lt.24671. PMID: 28061014.
Article8. Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. 2008; Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 9:629–635. DOI: 10.1016/S1470-2045(08)70153-0.
Article9. Mosteller RD. 1987; Simplified calculation of body-surface area. N Engl J Med. 317:1098. DOI: 10.1056/NEJM198710223171717. PMID: 3657876.
Article10. Hwang S, Lee SG, Lee YJ, Park KM, Jeon HB, Kim PN, et al. 1997; Calculation of standard liver volume of Korean adults. Korean J Hepatobiliary Pancreat Surg. 1:59–65.11. Hashimoto T, Sugawara Y, Tamura S, Hasegawa K, Kishi Y, Kokudo N, et al. 2006; Estimation of standard liver volume in Japanese living liver donors. J Gastroenterol Hepatol. 21:1710–1713. DOI: 10.1111/j.1440-1746.2006.04433.x. PMID: 16984594.
Article12. Yuan D, Lu T, Wei YG, Li B, Yan LN, Zeng Y, et al. 2008; Estimation of standard liver volume for liver transplantation in the Chinese population. Transplant Proc. 40:3536–3540. DOI: 10.1016/j.transproceed.2008.07.135. PMID: 19100432.
Article13. Poovathumkadavil A, Leung KF, Al Ghamdi HM, Othman Iel H, Meshikhes AW. 2010; Standard formula for liver volume in Middle Eastern Arabic adults. Transplant Proc. 42:3600–3605. DOI: 10.1016/j.transproceed.2010.07.098. PMID: 21094823.
Article14. Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. 2013; Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 31:1539–1547. DOI: 10.1200/JCO.2012.45.2722. PMID: 23530101.
Article15. Kim EY, Kim YS, Park I, Ahn HK, Cho EK, Jeong YM. 2015; Prognostic significance of CT-determined sarcopenia in patients with small-cell lung cancer. J Thorac Oncol. 10:1795–1799. DOI: 10.1097/JTO.0000000000000690. PMID: 26484630.
Article16. Kim EY, Lee HY, Kim YS, Park I, Ahn HK, Cho EK, et al. 2018; Prognostic significance of cachexia score assessed by CT in male patients with small cell lung cancer. Eur J Cancer Care (Engl). 27:e12695. DOI: 10.1111/ecc.12695. PMID: 28426181.
Article17. Zheng ZF, Lu J, Zheng CH, Li P, Xie JW, Wang JB, et al. 2017; A novel prognostic scoring system based on preoperative sarcopenia predicts the long-term outcome for patients after r0 resection for gastric cancer: experiences of a high-volume center. Ann Surg Oncol. 24:1795–1803. DOI: 10.1245/s10434-017-5813-7. PMID: 28213789.
Article18. Kim KM, Jang HC, Lim S. 2016; Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med. 31:643–650. DOI: 10.3904/kjim.2016.015. PMID: 27334763. PMCID: PMC4939509.
Article19. Merrill Z, Perera S, Chambers A, Cham R. 2019; Age and body mass index associations with body segment parameters. J Biomech. 88:38–47. DOI: 10.1016/j.jbiomech.2019.03.016. PMID: 30914188.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of skeletal muscle index-based formula and body surface area-based formula for calculating standard liver volume
- Calculation of Standard Liver Volume of Korean Adults
- Calculation of standard liver volume in Korean adults with analysis of confounding variables
- Types of Special Infant Formulas Marketed in Korea and Their Indications
- A new formula for estimation of standard liver volume using liver height and thoracic width