Korean Circ J.
2021 Jun;51(6):533-544. 10.4070/kcj.2020.0499.
Benefit of Extracorporeal Membrane Oxygenation before Revascularization in Patients with Acute Myocardial Infarction Complicated by Profound Cardiogenic Shock after Resuscitated Cardiac Arrest
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 3Department of Emergency Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2516215
- DOI: http://doi.org/10.4070/kcj.2020.0499
Abstract
- Background and Objectives
The study sought to investigate the impact of early extracorporeal membrane oxygenation (ECMO) support before revascularization in patients with acute myocardial infarction (AMI) complicated by profound cardiogenic shock after resuscitated cardiac arrest. It is difficult to determine optimal timing of ECMO in patients with AMI complicated by profound cardiogenic shock after resuscitated cardiac arrest.
Methods
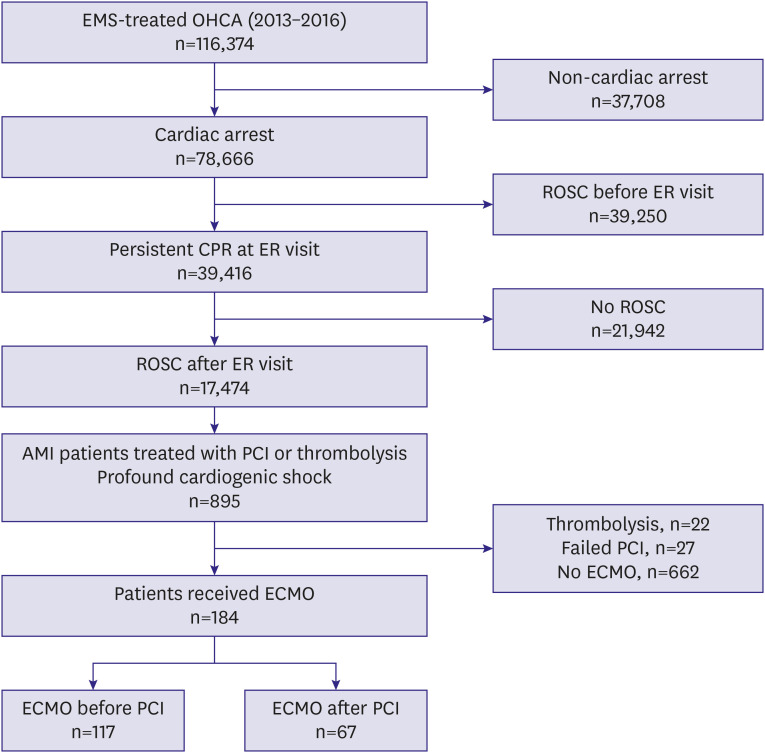
Among 116,374 patients experiencing out-of-hospital cardiac arrest in South Korea, a total of 184 resuscitated patients with AMI complicated by profound cardiogenic shock, and who were treated successfully with percutaneous coronary intervention (PCI) and ECMO, were enrolled. Patients were divided into 2 groups according to the timing of ECMO: pre-PCI ECMO (n=117) and post-PCI ECMO (n=67). We compared 30-day mortality between the 2 groups.
Results
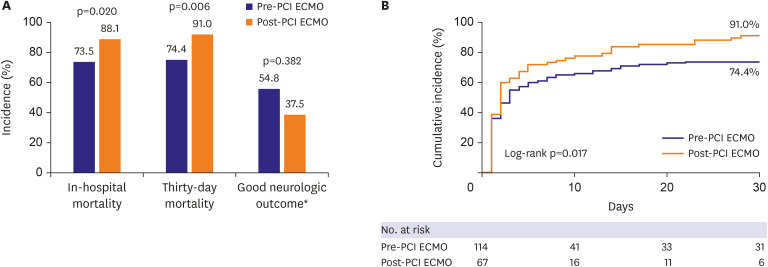
In-hospital mortality was 78.8% in the entire study population and significantly lower in the pre-PCI ECMO group (73.5% vs. 88.1%, p=0.020). Thirty-day mortality was also lower in the pre-PCI ECMO group compared to the post-PCI ECMO group (74.4% vs. 91.0%; adjusted hazard ratio [HR], 0.66; 95% confidence interval [CI], 0.47–0.93; p=0.017). Shockable rhythm at the emergency room (HR, 0.57; 95% CI, 0.36–0.91; p=0.019) and successful therapeutic hypothermia (HR, 0.40; 95% CI, 0.23–0.69; p=0.001) were also associated with improved 30-day survival.
Conclusions
ECMO support before revascularization was associated with an improved short-term survival rate compared to ECMO after revascularization in patients with AMI complicated by profound cardiogenic shock after resuscitated cardiac arrest.
Keyword
Figure
Cited by 2 articles
-
Do ECMO First Even in the Desperate Situation
Jung Ho Heo
Korean Circ J. 2021;51(6):545-546. doi: 10.4070/kcj.2021.0152.Editorial on Paper Titled Comparison of Veno-Arterial Extracorporeal Membrane Oxygenation Type in Patients Listed for Heart Transplantation
Jeong Hoon Yang
Korean Circ J. 2023;53(8):548-549. doi: 10.4070/kcj.2023.0168.
Reference
-
1. Menees DS, Peterson ED, Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013; 369:901–909. PMID: 24004117.
Article2. Eapen ZJ, Tang WH, Felker GM, et al. Defining heart failure end points in ST-segment elevation myocardial infarction trials: integrating past experiences to chart a path forward. Circ Cardiovasc Qual Outcomes. 2012; 5:594–600. PMID: 22811505.3. Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009; 119:1211–1219. PMID: 19237658.4. Goldberg RJ, Makam RC, Yarzebski J, McManus DD, Lessard D, Gore JM. Decade-long trends (2001–2011) in the incidence and hospital death rates associated with the in-hospital development of cardiogenic shock after acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2016; 9:117–125. PMID: 26884615.
Article5. Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med. 1999; 341:625–634. PMID: 10460813.6. Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006; 295:2511–2515. PMID: 16757723.
Article7. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–177. PMID: 28886621.8. Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37:267–315. PMID: 26320110.9. Kontos MC, Scirica BM, Chen AY, et al. Cardiac arrest and clinical characteristics, treatments and outcomes among patients hospitalized with ST-elevation myocardial infarction in contemporary practice: a report from the National Cardiovascular Data Registry. Am Heart J. 2015; 169:515–522.e1. PMID: 25819858.
Article10. Kvakkestad KM, Sandvik L, Andersen GØ, Sunde K, Halvorsen S. Long-term survival in patients with acute myocardial infarction and out-of-hospital cardiac arrest: a prospective cohort study. Resuscitation. 2018; 122:41–47. PMID: 29155294.
Article11. Ostenfeld S, Lindholm MG, Kjaergaard J, et al. Prognostic implication of out-of-hospital cardiac arrest in patients with cardiogenic shock and acute myocardial infarction. Resuscitation. 2015; 87:57–62. PMID: 25475249.
Article12. Thiele H, Ohman EM, Desch S, Eitel I, de Waha S. Management of cardiogenic shock. Eur Heart J. 2015; 36:1223–1230. PMID: 25732762.
Article13. Abrams D, Combes A, Brodie D. Extracorporeal membrane oxygenation in cardiopulmonary disease in adults. J Am Coll Cardiol. 2014; 63:2769–2778. PMID: 24814488.
Article14. Cove ME, MacLaren G. Clinical review: mechanical circulatory support for cardiogenic shock complicating acute myocardial infarction. Crit Care. 2010; 14:235. PMID: 21067535.
Article15. Kim H, Lim SH, Hong J, et al. Efficacy of veno-arterial extracorporeal membrane oxygenation in acute myocardial infarction with cardiogenic shock. Resuscitation. 2012; 83:971–975. PMID: 22322287.
Article16. Sheu JJ, Tsai TH, Lee FY, et al. Early extracorporeal membrane oxygenator-assisted primary percutaneous coronary intervention improved 30-day clinical outcomes in patients with ST-segment elevation myocardial infarction complicated with profound cardiogenic shock. Crit Care Med. 2010; 38:1810–1817. PMID: 20543669.
Article17. Kagawa E, Dote K, Kato M, et al. Should we emergently revascularize occluded coronaries for cardiac arrest?: rapid-response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation. 2012; 126:1605–1613. PMID: 22899771.18. Ouweneel DM, Schotborgh JV, Limpens J, et al. Extracorporeal life support during cardiac arrest and cardiogenic shock: a systematic review and meta-analysis. Intensive Care Med. 2016; 42:1922–1934. PMID: 27647331.
Article19. Jung E, Park JH, Kong SY, et al. Cardiac arrest while exercising on mountains in national or provincial parks: a national observational study from 2012 to 2015. Am J Emerg Med. 2018; 36:1350–1355. PMID: 29287617.
Article20. Ro YS, Shin SD, Song KJ, et al. Effects of dispatcher-assisted cardiopulmonary resuscitation on survival outcomes in infants, children, and adolescents with out-of-hospital cardiac arrests. Resuscitation. 2016; 108:20–26. PMID: 27592157.
Article21. Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015; 132:1286–1300. PMID: 25391522.22. Choi SW, Shin SD, Ro YS, Song KJ, Lee EJ, Ahn KO. Effect of therapeutic hypothermia on the outcomes after out-of-hospital cardiac arrest according to initial ECG rhythm and witnessed status: a nationwide observational interaction analysis. Resuscitation. 2016; 100:51–59. PMID: 26774175.
Article23. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012; 33:2551–2567. PMID: 22922414.24. Huang CC, Hsu JC, Wu YW, et al. Implementation of extracorporeal membrane oxygenation before primary percutaneous coronary intervention may improve the survival of patients with ST-segment elevation myocardial infarction and refractory cardiogenic shock. Int J Cardiol. 2018; 269:45–50. PMID: 30077527.
Article25. Demondion P, Fournel L, Golmard JL, Niculescu M, Pavie A, Leprince P. Predictors of 30-day mortality and outcome in cases of myocardial infarction with cardiogenic shock treated by extracorporeal life support. Eur J Cardiothorac Surg. 2014; 45:47–54. PMID: 23616484.
Article26. Choi KH, Yang JH, Hong D, et al. Optimal timing of venoarterial-extracorporeal membrane oxygenation in acute myocardial infarction patients suffering from refractory cardiogenic shock. Circ J. 2020; 84:1502–1510. PMID: 32684541.
Article27. Chung SY, Tong MS, Sheu JJ, et al. Short-term and long-term prognostic outcomes of patients with ST-segment elevation myocardial infarction complicated by profound cardiogenic shock undergoing early extracorporeal membrane oxygenator-assisted primary percutaneous coronary intervention. Int J Cardiol. 2016; 223:412–417. PMID: 27544596.
Article28. Anderson ML, Peterson ED, Peng SA, et al. Differences in the profile, treatment, and prognosis of patients with cardiogenic shock by myocardial infarction classification: a report from NCDR. Circ Cardiovasc Qual Outcomes. 2013; 6:708–715. PMID: 24221834.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Circulatory Support in the Cardiac Catheterization Laboratory for Cardiogenic Shock
- A case of rescuing a patient with acute cardiovascular instability from sudden and massive intraoperative pulmonary thromboembolism by extracorporeal membrane oxygenation
- Use of amplitude-integrated electroencephalography in decision-making for extracorporeal membrane oxygenation in comatose cardiac arrest patients whose eventual neurologic recovery is uncertain
- Successful Left-Heart Decompression during Extracorporeal Membrane Oxygenation in an Adult Patient by Percutaneous Transaortic Catheter Venting
- Acute fulminant myocarditis following influenza vaccination requiring extracorporeal membrane oxygenation