J Korean Med Sci.
2021 May;36(20):e136. 10.3346/jkms.2021.36.e136.
Procedural Sedation for Pediatric Upper Gastrointestinal Endoscopy in Korea
- Affiliations
-
- 1Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 2Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea
- 4Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- 5Department of Pediatrics, Hallym University College of Medicine, Chuncheon, Korea
- 6Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- 7Department of Pediatrics, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 8Department of Pediatrics, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 9Department of Pediatrics, Nowon Eulji Medical Center, Eulji University School of Medicine, Seoul, Korea
- 10Department of Pediatrics, Chung-Ang University Hospital, College of Medicine, Chung-Ang University, Seoul, Korea
- 11Department of Pediatrics, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 12Department of Pediatrics, Inje University Ilsan Paik Hospital, Goyang, Korea
- 13Department of Pediatrics, Daegu Catholic University School of Medicine, Daegu, Korea
- 14Department of Pediatrics, Daejeon Eulji Medical Center, Eulji University School of Medicine, Daejeon, Korea
- 15Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 16Department of Pediatrics, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea
- 17Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2516048
- DOI: http://doi.org/10.3346/jkms.2021.36.e136
Abstract
- Background
Sedative upper endoscopy is similar in pediatrics and adults, but it is characteristically more likely to lead to respiratory failure. Although recommended guidelines for pediatric procedural sedation are available within South Korea and internationally, Korean pediatric endoscopists use different drugs, either alone or in combination, in practice. Efforts are being made to minimize the risk of sedation while avoiding procedural challenges. The purpose of this study was to collect and analyze data on the sedation methods used by Korean pediatric endoscopists to help physicians perform pediatric sedative upper endoscopy (PSUE).
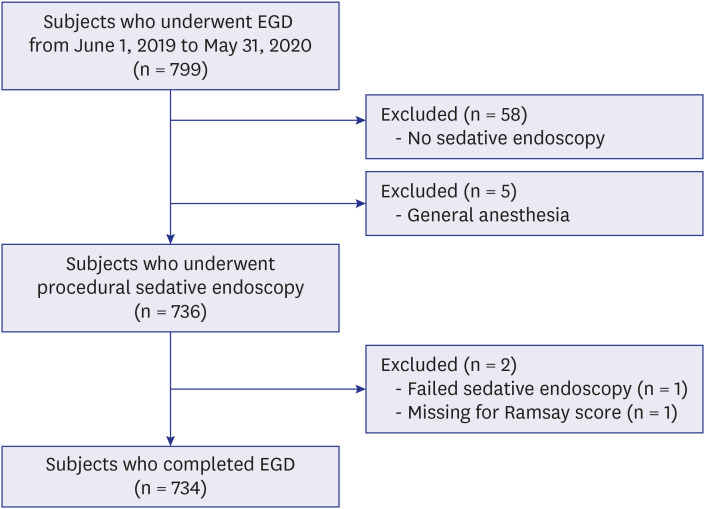
Methods
The PSUE procedures performed in 15 Korean pediatric gastrointestinal endoscopic units within a year were analyzed. Drugs used for sedation were grouped according to the method of use, and the depth of sedation was evaluated based on the Ramsay scores. The procedures and their complications were also assessed.
Results
In total, 734 patients who underwent PSUE were included. Sedation and monitoring were performed by an anesthesiologist at one of the institutions. The sedative procedures were performed by a pediatric endoscopist at the other 14 institutions. Regarding the number of assistants present during the procedures, 36.6% of procedures had one assistant, 38.8% had 2 assistants, and 24.5% had 3 assistants. The average age of the patients was 11.6 years old. Of the patients, 19.8% had underlying diseases, 10.0% were taking medications such as epilepsy drugs, and 1.0% had snoring or sleep apnea history. The average duration of the procedures was 5.2 minutes. The subjects were divided into 5 groups as follows: 1) midazolam + propofol + ketamine (M + P + K): n = 18, average dose of 0.03 + 2.4 + 0.5 mg/kg; 2) M + P: n = 206, average dose of 0.06 + 2.1 mg/kg; 3) M + K: n = 267, average dose of 0.09 + 0.69 mg/kg; 4) continuous P infusion for 20 minutes: n = 15, average dose of 6.6 mg/kg; 5) M: n = 228, average dose of 0.11 mg/kg. The average Ramsay score for the five groups was 3.7, with significant differences between the groups (P < 0.001). Regarding the adverse effects, desaturation and increased oxygen supply were most prevalent in the M + K group. Decreases and increases in blood pressure were most prevalent in the M + P + K group, and bag-mask ventilation was most used in the M + K group. There were no reported incidents of intubation or cardiopulmonary resuscitation. A decrease in oxygen saturation was observed in 37 of 734 patients, and it significantly increased in young patients (P = 0.001) and when ketamine was used (P = 0.014). Oxygen saturation was also correlated with dosage (P = 0.037). The use of ketamine (P < 0.001) and propofol (P < 0.001) were identified as factors affecting the Ramsay score in the logistic regression analysis.
Conclusion
Although the drug use by Korean pediatric endoscopists followed the recommended guidelines to an extent, it was apparent that they combined the drugs or reduced the doses depending on the patient characteristics to reduce the likelihood of respiratory failure. Inducing deep sedation facilitates comfort during the procedure, but it also leads to a higher risk of complications.
Figure
Cited by 1 articles
-
Letter to the Editor: Optimal Method for Sedation of Pediatric Upper Gastrointestinal Endoscopy
Soon Chul Kim
J Korean Med Sci. 2021;36(35):e254. doi: 10.3346/jkms.2021.36.e254.
Reference
-
1. Krauss B, Green SM. Procedural sedation and analgesia in children. Lancet. 2006; 367(9512):766–780. PMID: 16517277.
Article2. van Beek EJ, Leroy PL. Safe and effective procedural sedation for gastrointestinal endoscopy in children. J Pediatr Gastroenterol Nutr. 2012; 54(2):171–185. PMID: 21975965.
Article3. Orel R, Brecelj J, Dias JA, Romano C, Barros F, Thomson M, et al. Review on sedation for gastrointestinal tract endoscopy in children by non-anesthesiologists. World J Gastrointest Endosc. 2015; 7(9):895–911. PMID: 26240691.
Article4. Lightdale JR, Mahoney LB, Schwarz SM, Liacouras CA. Methods of sedation in pediatric endoscopy: a survey of NASPGHAN members. J Pediatr Gastroenterol Nutr. 2007; 45(4):500–502. PMID: 18030225.
Article5. Tringali A, Thomson M, Dumonceau JM, Tavares M, Tabbers MM, Furlano R, et al. Pediatric gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) guideline executive summary. Endoscopy. 2017; 49(1):83–91. PMID: 27617420.
Article6. Sessler CN, Grap MJ, Ramsay MA. Evaluating and monitoring analgesia and sedation in the intensive care unit. Crit Care. 2008; 12 Suppl 3(Suppl 3):S2.
Article7. Yang SM, Yi DY, Choi GJ, Lim IS, Chae SA, Yun SW, et al. Effects of sedation performed by an anesthesiologist on pediatric endoscopy: a single-center retrospective study in Korea. J Korean Med Sci. 2020; 35(21):e183. PMID: 32476304.
Article8. Boudewyns A, Saldien V, Van de Heyning P, Verhulst S. Drug-induced sedation endoscopy in surgically naïve infants and children with obstructive sleep apnea: impact on treatment decision and outcome. Sleep Breath. 2018; 22(2):503–510. PMID: 29081031.
Article9. Gazzaz MJ, Isaac A, Anderson S, Alsufyani N, Alrajhi Y, El-Hakim H. Does drug-induced sleep endoscopy change the surgical decision in surgically naïve non-syndromic children with snoring/sleep disordered breathing from the standard adenotonsillectomy? A retrospective cohort study. J Otolaryngol Head Neck Surg. 2017; 46(1):12. PMID: 28193298.
Article10. Kandil A, Subramanyam R, Hossain MM, Ishman S, Shott S, Tewari A, et al. Comparison of the combination of dexmedetomidine and ketamine to propofol or propofol/sevoflurane for drug-induced sleep endoscopy in children. Paediatr Anaesth. 2016; 26(7):742–751. PMID: 27212000.
Article11. Boudewyns A, Verhulst S, Maris M, Saldien V, Van de Heyning P. Drug-induced sedation endoscopy in pediatric obstructive sleep apnea syndrome. Sleep Med. 2014; 15(12):1526–1531. PMID: 25311832.
Article12. Liu KA, Liu CC, Alex G, Szmuk P, Mitchell RB. Anesthetic management of children undergoing drug-induced sleep endoscopy: a retrospective review. Int J Pediatr Otorhinolaryngol. 2020; 139:110440. PMID: 33080472.
Article13. Riesco-López JM, Rizo-Pascual J, Díaz-Sánchez A, Manzano-Fernández R, Martín-Saborido C, Varillas-Delgado D, et al. Endoscopist-directed propofol is more efficient than anesthesiologist-administered propofol in patients at low-intermediate anesthetic risk. Eur J Gastroenterol Hepatol. 2020; 32(11):1440–1446. PMID: 32925498.
Article14. Coté CJ, Wilson S. American Academy of Pediatrics. American Academy of Pediatric Dentistry. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures. Pediatrics. 2019; 143(6):e20191000. PMID: 31138666.
Article15. Klotz D, Seifert V, Baumgartner J, Teufel U, Fuchs H. High-flow nasal cannula vs standard respiratory care in pediatric procedural sedation: a randomized controlled pilot trial. Pediatr Pulmonol. 2020; 55(10):2706–2712. PMID: 32696598.
Article16. Biber JL, Allareddy V, Allareddy V, Gallagher SM, Couloures KG, Speicher DG, et al. Prevalence and predictors of adverse events during procedural sedation anesthesia-outside the operating room for esophagogastroduodenoscopy and colonoscopy in children: age is an independent predictor of outcomes. Pediatr Crit Care Med. 2015; 16(8):e251–e259. PMID: 26218257.17. Oh JE, Lee HJ, Lee YH. Propofol versus midazolam for sedation during esophagogastroduodenoscopy in children. Clin Endosc. 2013; 46(4):368–372. PMID: 23964333.
Article18. Cravero JP, Blike GT, Beach M, Gallagher SM, Hertzog JH, Havidich JE, et al. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the Pediatric Sedation Research Consortium. Pediatrics. 2006; 118(3):1087–1096. PMID: 16951002.
Article19. Rafeey M, Ghojazadeh M, Feizo Allah Zadeh H, Majidi H. Use of oral midazolam in pediatric upper gastrointestinal endoscopy. Pediatr Int. 2010; 52(2):191–195. PMID: 19664010.
Article20. Motamed F, Aminpour Y, Hashemian H, Soltani AE, Najafi M, Farahmand F. Midazolam-ketamine combination for moderate sedation in upper GI endoscopy. J Pediatr Gastroenterol Nutr. 2012; 54(3):422–426. PMID: 21857244.
Article21. Tosun Z, Esmaoglu A, Coruh A. Propofol-ketamine vs propofol-fentanyl combinations for deep sedation and analgesia in pediatric patients undergoing burn dressing changes. Paediatr Anaesth. 2008; 18(1):43–47. PMID: 18095965.
Article22. Hong H, Hahn S, Choi Y, Jang MJ, Kim S, Lee JH, et al. Evaluation of propofol in comparison with other general anesthetics for surgery in children younger than 3 years: a systematic review and meta-analysis. J Korean Med Sci. 2019; 34(15):e124. PMID: 31001938.
Article23. Rajasekaran S, Hackbarth RM, Davis AT, Kopec JS, Cloney DL, Fitzgerald RK, et al. The safety of propofol sedation for elective nonintubated esophagogastroduodenoscopy in pediatric patients. Pediatr Crit Care Med. 2014; 15(6):e261–9. PMID: 24849145.
Article24. Paspatis GA, Charoniti I, Manolaraki M, Vardas E, Papanikolaou N, Anastasiadou A, et al. Synergistic sedation with oral midazolam as a premedication and intravenous propofol versus intravenous propofol alone in upper gastrointestinal endoscopies in children: a prospective, randomized study. J Pediatr Gastroenterol Nutr. 2006; 43(2):195–199. PMID: 16877984.25. Uludağ Ö, Doğukan M, Kaya R, Tutak A, Dumlupinar E. Comparison of the effects of midazolam ketamine or midazolam-propofol combinations on hemodynamic stability, patient comfort, and post-anesthesia recovery in children undergoing sedation for magnetic resonance imaging procedures. Ain-Shams J Anesthesiology. 2020; 12(1):1–7.
Article26. Chayapathi V, Kalra M, Bakshi AS, Mahajan A. A comparison of ketamine + midazolam to propofol for procedural sedation for lumbar puncture in pediatric oncology by nonanesthesiologists-a randomized comparative trial. Pediatr Blood Cancer. 2018; 65(8):e27108. PMID: 29727056.27. Khoshoo V, Thoppil D, Landry L, Brown S, Ross G. Propofol versus midazolam plus meperidine for sedation during ambulatory esophagogastroduodenoscopy. J Pediatr Gastroenterol Nutr. 2003; 37(2):146–149. PMID: 12883300.
Article28. Jang HY, Jung JH, Kyong YY, Kim KH, Kim DK, Kim MR, et al. Korean guidelines for pediatric procedural sedation and analgesia. J Korean Soc Emerg Med. 2012; 23(3):303–314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sedation for Pediatric Endoscopy
- The Evalution of Patient Anxiety Associated with Upper Gastrointestinal Endoscopy
- Procedural sedation and analgesia in pediatric emergency department
- Sedation in Pediatric Esophagogastroduodenoscopy
- Upper gastrointestinal diseases diagnosed by upper gastrointestinal fiberoptic endoscopy in children