J Korean Med Sci.
2021 May;36(18):e116. 10.3346/jkms.2021.36.e116.
Analysis of Pediatric Surgery Using the National Healthcare Insurance Service Database in Korea: How Many Pediatric Surgeons Do We Need in Korea?
- Affiliations
-
- 1Department of Pediatric Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Seoul, Korea
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Pediatric Surgery, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea
- 4Department of Pediatric Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 5Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2515853
- DOI: http://doi.org/10.3346/jkms.2021.36.e116
Abstract
- Background
In the past, general surgeons (GSs) without a pediatric surgical subspecialty often performed surgery on children and, even now, GSs are performing many pediatric surgeries. We aimed to investigate the involvement of pediatric surgeons (PSs) and GSs in pediatric surgery, compare the outcomes of surgery in the neonatal intensive care unit (NICU), and estimate the appropriate PS workforce in Korea.
Methods
We used surgical data from the National Health Insurance Service database that was collected from patients under the age of 19 years in hospitals nationwide from January 2002 to December 2017. In this database, we found 37 hospitals where PSs worked by using the index operation (congenital diaphragmatic hernia, esophageal atresia, hypertrophic pyloric stenosis, Hirschsprung's disease, abdominal wall defect, jejunoileal atresia, malrotation, anorectal malformation, and biliary atresia). It was assumed that the surgery in the 37 hospitals was performed by PS and that the surgery in other hospitals was performed by GS. Mortality was analyzed to compare the outcomes of acute abdominal surgery in the NICU. We estimated the number of PS currently needed in Korea for each situation under the assumption that PS would perform all operations for the index operation, main pediatric diseases (index operation + gastroesophageal reflux disease, choledochal cyst, inguinal hernia, and appendicitis), acute abdominal surgery in the NICU, and all pediatric surgeries. Additionally, we estimated the appropriate number of PS required for more advanced pediatric surgery in the future.
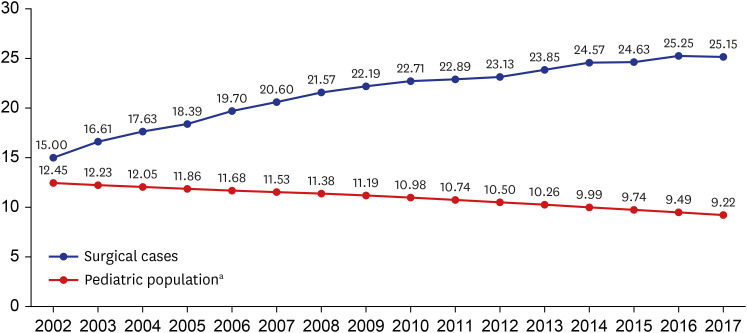
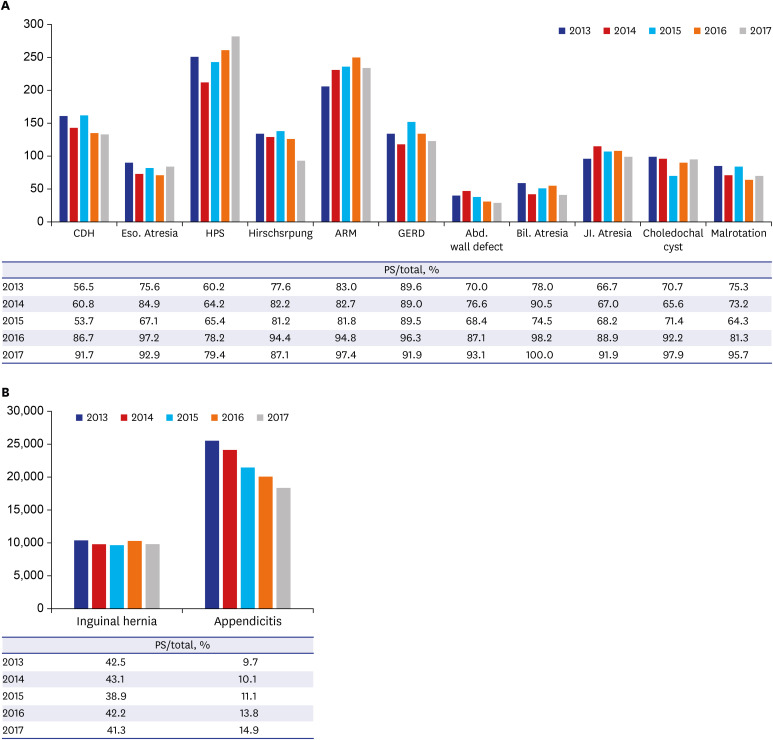
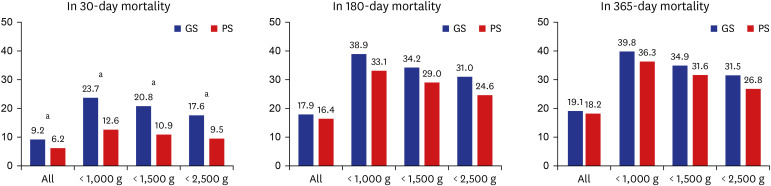
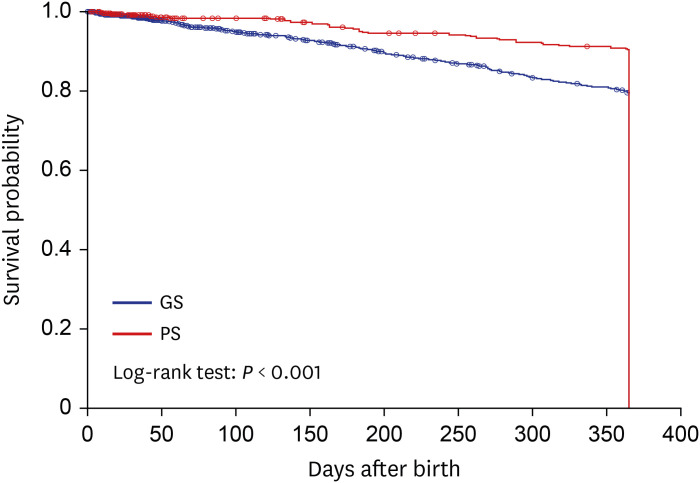
Results
The number of pediatric surgeries from 2002 to 2017 increased by 124%. Approximately 10.25% of the total pediatric surgeries were performed by PSs, and the percentage of the surgery performed by PSs increased from 8.32% in 2002 to 15.92% in 2017. The percentage of index operations performed by PSs annually was 62.44% in average. It was only 47.81% in 2002, and increased to 88.79% in 2017. During the last 5 years of the study period, the average annual number of surgeries for main pediatric diseases was approximately 33,228. The ratio of the number of surgeries performed by PS vs. GS steadily increased in main pediatric diseases, however, the ratio of the number of surgery performed by PS for inguinal hernia and appendicitis remained low in the most recent years. The percentage of the number of acute abdominal surgery performed by PS in the NICU was 44% in 2002, but it had recently risen to 89.7%. After 30 days of birth, mortality was significantly lower in all groups that were operated on by PS, rather than GS, during the last 5 years. In 2019, 49 PSs who were under the age of 65 years were actively working in Korea. Assuming that all pediatric surgeries of the patients under the age of 19 years should be performed by PS, the minimum number of PS currently required was about 63 if they perform all of the index operations, the main pediatric surgery was about 209, the NICU operation was about 63, and the all pediatric surgeries was about 366. Additionally, it was determined that approximately 165 to 206 PS will be appropriate for Korea to implement more advanced pediatric surgery in the future.
Conclusion
The proportion of the pediatric surgery performed by PS rather than GS is increasing in Korea, but it is still widely performed by GS. PSs have better operative outcomes for acute abdominal surgery in the NICU than GSs. We believe that at least the index operation or the NICU operation should be performed by PS for better outcome, and that a minimum of 63 PSs are needed in Korea to do so. In addition, approximately 200 PSs will be required in Korea in order to manage main pediatric diseases and to achieve more advanced pediatric surgery in the future.
Keyword
Figure
Reference
-
1. Hong J, Sim J. A single pediatric surgeon working in a single center: Was there a change in the pediatric surgeon's role following 25 years of service in Suwon City? Adv Pediatr Surg. 2020; 26(1):1–10.
Article2. Oh JT, Chang HK, Cho MJ, Cho YH, Choi SJ, Choi YM, et al. Sacrococcygeal teratoma: a survey by the Korean Association of Pediatric Surgeons in 2018. Adv Pediatr Surg. 2019; 25(2):35–43.
Article3. Langer JC, To T. Does pediatric surgical specialty training affect outcome after Ramstedt pyloromyotomy? A population-based study. Pediatrics. 2004; 113(5):1342–1347. PMID: 15121951.
Article4. Baird R, Eeson G, Safavi A, Puligandla P, Laberge JM, Skarsgard ED, et al. Institutional practice and outcome variation in the management of congenital diaphragmatic hernia and gastroschisis in Canada: a report from the Canadian Pediatric Surgery Network. J Pediatr Surg. 2011; 46(5):801–807. PMID: 21616230.
Article5. McKiernan PJ, Baker AJ, Kelly DA. The frequency and outcome of biliary atresia in the UK and Ireland. Lancet. 2000; 355(9197):25–29. PMID: 10615887.
Article6. da Silva PS, de Aguiar VE, Waisberg J. Pediatric surgeon vs general surgeon: Does subspecialty training affect the outcome of appendicitis? Pediatr Int. 2014; 56(2):248–253. PMID: 24004383.
Article7. McAteer JP, Kwon S, LaRiviere CA, Oldham KT, Goldin AB. Pediatric specialist care is associated with a lower risk of bowel resection in children with intussusception: a population-based analysis. J Am Coll Surg. 2013; 217(2):226–232.e1-3. PMID: 23664141.
Article8. Borenstein SH, To T, Wajja A, Langer JC. Effect of subspecialty training and volume on outcome after pediatric inguinal hernia repair. J Pediatr Surg. 2005; 40(1):75–80. PMID: 15868562.
Article9. Boo YJ, Lee EH, Lee JS. Comparison of surgical outcomes among infants in neonatal intensive care units treated by pediatric surgeons versus general surgeons: the need for pediatric surgery specialists. J Pediatr Surg. 2017; 52(11):1715–1717. PMID: 28189454.
Article10. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.
Article11. Hamad D, Yousef Y, Caminsky NG, Guadagno E, Tran VA, Laberge JM, et al. Defining the critical pediatric surgical workforce density for improving surgical outcomes: a global study. J Pediatr Surg. 2020; 55(3):493–512. PMID: 31839371.
Article12. The Statistics Korea. Korean Statistical Information Service. Updated 2020. Accessed December 31, 2020. https://kosis.kr/search/search.do.13. Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004; 198(4):626–632. PMID: 15051016.14. Archampong D, Borowski D, Wille-Jørgensen P, Iversen LH. Workload and surgeon's specialty for outcome after colorectal cancer surgery. Cochrane Database Syst Rev. 2012; (3):CD005391. PMID: 22419309.
Article15. Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg. 2007; 94(2):145–161. PMID: 17256810.
Article16. Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol. 2000; 18(11):2327–2340. PMID: 10829054.
Article17. O'Neill JA Jr, Gautam S, Geiger JD, Ein SH, Holder TM, Bloss RS, et al. A longitudinal analysis of the pediatric surgeon workforce. Ann Surg. 2000; 232(3):442–453. PMID: 10973394.18. Emil S, Blair G, Langer JC, Miller G, Aspirot A, Brisseau G, et al. A survey-based assessment of the Canadian pediatric surgery workforce. J Pediatr Surg. 2014; 49(5):678–681. PMID: 24851747.
Article19. Reich DA, Herbst KW, Campbell BT. The recent evolution of the breadth of practice for pediatric surgeons in the United States, 2005-2014. Pediatr Surg Int. 2019; 35(4):517–522. PMID: 30607543.
Article20. O'Neill JA Jr, Vander Zwagg R. Update on the analysis of the need for pediatric surgeons in the United States. J Pediatr Surg. 1980; 15(6):918–924. PMID: 7463295.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Cancer Research using Healthcare Big Data
- Clinical Study Using Healthcare Claims Database
- Trends in Ankyloglossia and Surgical Treatment among Pediatric Patients in South Korea
- Introducing big data analysis using data from National Health Insurance Service
- A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples