Ann Clin Neurophysiol.
2021 Apr;23(1):17-28. 10.14253/acn.2021.23.1.17.
Targeting the culprit: vessel wall magnetic resonance imaging for evaluating stroke
- Affiliations
-
- 1Department of Neurology, Veterans Health Service Medical Center, Seoul, Korea
- 2Department of Neurology, Asan Medical Center, Seoul, Korea
- 3Department of Neurology, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2515604
- DOI: http://doi.org/10.14253/acn.2021.23.1.17
Abstract
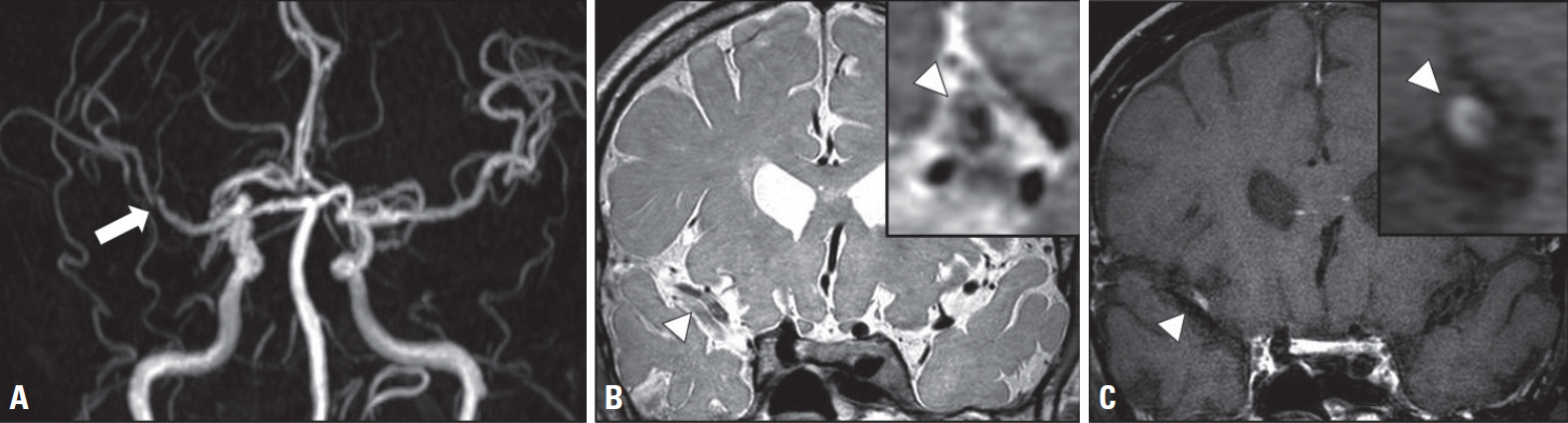
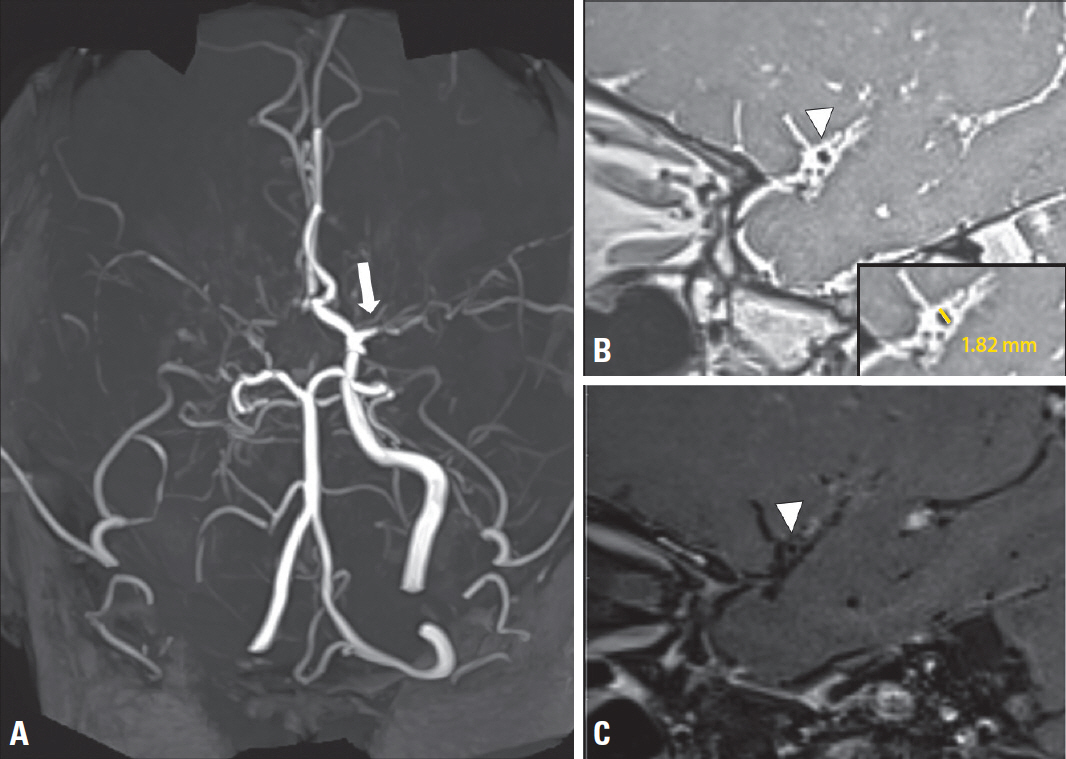
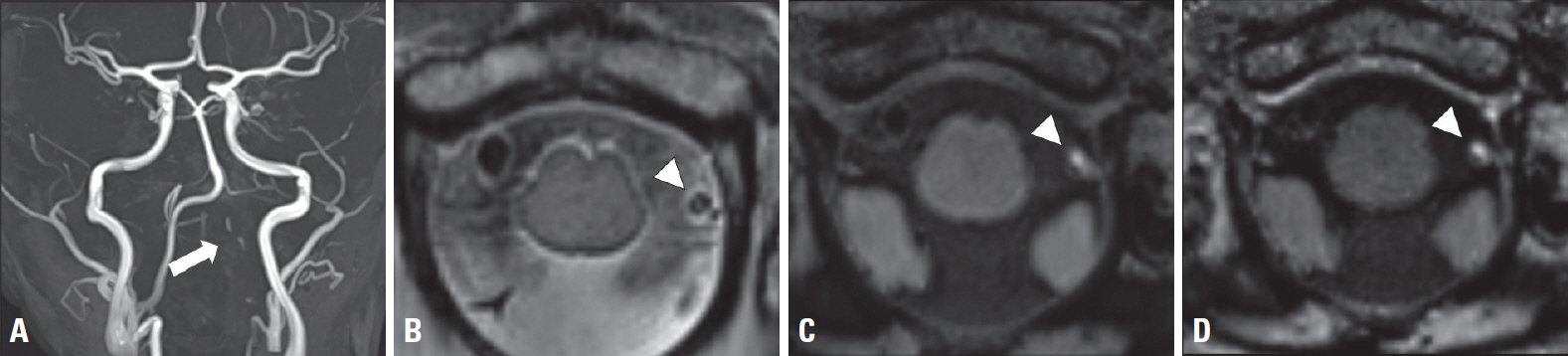
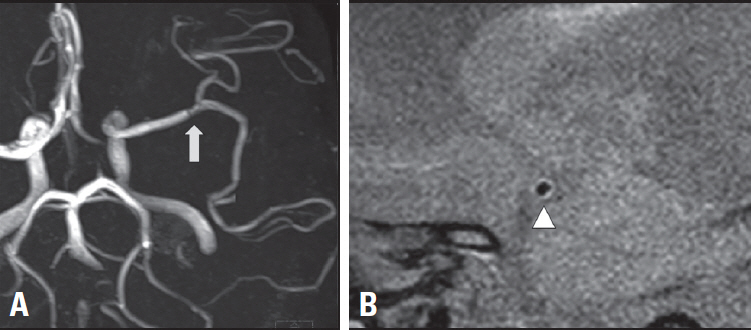
- The pathogenesis of many strokes originates in the vessel wall. Despite this, most traditional imaging focuses on the vascular lumen. Vessel-wall magnetic resonance imaging (VWMRI) is useful for establishing the etiology of intracranial stenosis. It also provides information regarding atherosclerotic plaque composition and thus plaque vulnerability, which is an indication of its potential to cause a stroke. In this review we focus on the characteristics of VWMRI findings in various arteriopathies related to intracranial artery stenosis, and discuss the clinical implications of these findings.
Keyword
Figure
Reference
-
1. Kim BJ, Kim JS. Ischemic stroke subtype classification: an asian viewpoint. J Stroke. 2014; 16:8–17.
Article2. Kim BJ, Kang HG, Kim HJ, Ahn SH, Kim NY, Warach S, et al. Magnetic resonance imaging in acute ischemic stroke treatment. J Stroke. 2014; 16:131–145.
Article3. Kim SM, Kim YJ, Kim K, Kim BJ. Usefulness of carotid ultrasonography and treatment of carotid disease. J Korean Med Assoc. 2020; 63:342–353.
Article4. Kim JS, Nah HW, Park SM, Kim SK, Cho KH, Lee J, et al. Risk factors and stroke mechanisms in atherosclerotic stroke: intracranial compared with extracranial and anterior compared with posterior circulation disease. Stroke. 2012; 43:3313–3318.5. Kim JS, Bonovich D. Research on intracranial atherosclerosis from the East and west: why are the results different? J Stroke. 2014; 16:105–113.
Article6. Kim BJ, Lee KM, Lee SH, Kim HG, Kim EJ, Heo SH, et al. Ethnic differences in intracranial artery tortuosity: a possible reason for different locations of cerebral atherosclerosis. J Stroke. 2018; 20:140–141.
Article7. Kim YS, Kim BJ, Noh KC, Lee KM, Heo SH, Choi HY, et al. Distal versus proximal middle cerebral artery occlusion: different mechanisms. Cerebrovasc Dis. 2019; 47:238–244.
Article8. Ha SH, Chang JY, Lee SH, Lee KM, Heo SH, Chang DI, et al. Mechanism of stroke according to the severity and location of atherosclerotic middle cerebral artery disease. J Stroke Cerebrovasc Dis. 2021; 30:105503.
Article9. Mandell DM, Mossa-Basha M, Qiao Y, Hess CP, Hui F, Matouk C, et al. Intracranial vessel wall MRI: Principles and Expert Consensus Recommendations of the American Society of Neuroradiology. AJNR Am J Neuroradiol. 2017; 38:218–229.
Article10. Kim BJ, Yoon Y, Lee DH, Kang DW, Kwon SU, Kim JS. The shape of middle cerebral artery and plaque location: high-resolution MRI finding. Int J Stroke. 2015; 10:856–860.
Article11. Fuster V, Moreno PR, Fayad ZA, Corti R, Badimon JJ. Atherothrombosis and high-risk plaque: part I: evolving concepts. J Am Coll Cardiol. 2005; 46:937–954.12. Dieleman N, Yang W, Abrigo JM, Chu WC, van der Kolk AG, Siero JC, et al. Magnetic resonance imaging of plaque morphology, burden, and distribution in patients with symptomatic middle cerebral artery stenosis. Stroke. 2016; 47:1797–1802.
Article13. Xu WH, Li ML, Gao S, Ni J, Zhou LX, Yao M, et al. In vivo high-resolution MR imaging of symptomatic and asymptomatic middle cerebral artery atherosclerotic stenosis. Atherosclerosis. 2010; 212:507–511.
Article14. Kim JM, Jung KH, Sohn CH, Moon J, Shin JH, Park J, et al. Intracranial plaque enhancement from high resolution vessel wall magnetic resonance imaging predicts stroke recurrence. Int J Stroke. 2016; 11:171–179.
Article15. Vakil P, Vranic J, Hurley MC, Bernstein RA, Korutz AW, Habib A, et al. T1 gadolinium enhancement of intracranial atherosclerotic plaques associated with symptomatic ischemic presentations. AJNR Am J Neuroradiol. 2013; 34:2252–2258.
Article16. Chen XY, Wong KS, Lam WW, Zhao HL, Ng HK. Middle cerebral artery atherosclerosis: histological comparison between plaques associated with and not associated with infarct in a postmortem study. Cerebrovasc Dis. 2008; 25:74–80.
Article17. Portanova A, Hakakian N, Mikulis DJ, Virmani R, Abdalla WM, Wasserman BA. Intracranial vasa vasorum: insights and implications for imaging. Radiology. 2013; 267:667–679.
Article18. Parma L, Baganha F, Quax PHA, de Vries MR. Plaque angiogenesis and intraplaque hemorrhage in atherosclerosis. Eur J Pharmacol. 2017; 816:107–115.
Article19. Chu B, Kampschulte A, Ferguson MS, Kerwin WS, Yarnykh VL, O’Brien KD, et al. Hemorrhage in the atherosclerotic carotid plaque: a high-resolution MRI study. Stroke. 2004; 35:1079–1084.
Article20. Kim BJ, Kim HY, Jho W, Kim YS, Koh SH, Heo SH, et al. Asymptomatic basilar artery plaque distribution and vascular geometry. J Atheroscler Thromb. 2019; 26:1007–1014.
Article21. Yang WJ, Fisher M, Zheng L, Niu CB, Paganini-Hill A, Zhao HL, et al. Histological characteristics of intracranial atherosclerosis in a Chinese population: a postmortem study. Front Neurol. 2017; 8:488.
Article22. Yang WJ, Chen XY, Zhao HL, Niu CB, Xu Y, Wong KS, et al. In vitro assessment of histology verified intracranial atherosclerotic disease by 1.5T magnetic resonance imaging: concentric or eccentric? Stroke. 2016; 47:527–530.
Article23. Chung GH, Kwak HS, Hwang SB, Jin GY. High resolution MR imaging in patients with symptomatic middle cerebral artery stenosis. Eur J Radiol. 2012; 81:4069–4074.
Article24. Qiao Y, Anwar Z, Intrapiromkul J, Liu L, Zeiler SR, Leigh R, et al. Patterns and implications of intracranial arterial remodeling in stroke patients. Stroke. 2016; 47:434–440.
Article25. Pasterkamp G, Schoneveld AH, van der Wal AC, Hijnen DJ, van Wolveren WJ, Plomp S, et al. Inflammation of the atherosclerotic cap and shoulder of the plaque is a common and locally observed feature in unruptured plaques of femoral and coronary arteries. Arterioscler Thromb Vasc Biol. 1999; 19:54–58.
Article26. Shi MC, Wang SC, Zhou HW, Xing YQ, Cheng YH, Feng JC, et al. Compensatory remodeling in symptomatic middle cerebral artery atherosclerotic stenosis: a high-resolution MRI and microemboli monitoring study. Neurol Res. 2012; 34:153–158.
Article27. Watanabe Y, Nagayama M. MR plaque imaging of the carotid artery. Neuroradiology. 2010; 52:253–274.
Article28. Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969; 20:288–299.29. Bang OY, Ryoo S, Kim SJ, Yoon CH, Cha J, Yeon JY, et al. Adult moyamoya disease: a burden of intracranial stenosis in East Asians? PLoS One. 2015; 10:e0130663.
Article30. Kim JS. Moyamoya disease: epidemiology, clinical features, and diagnosis. J Stroke. 2016; 18:2–11.
Article31. Kaku Y, Morioka M, Ohmori Y, Kawano T, Kai Y, Fukuoka H, et al. Outer-diameter narrowing of the internal carotid and middle cerebral arteries in moyamoya disease detected on 3D constructive interference in steady-state MR image: is arterial constrictive remodeling a major pathogenesis? Acta Neurochir (Wien). 2012; 154:2151–2157.
Article32. Takagi Y, Kikuta K, Nozaki K, Hashimoto N. Histological features of middle cerebral arteries from patients treated for Moyamoya disease. Neurol Med Chir (Tokyo). 2007; 47:1–4.
Article33. Kim YJ, Lee DH, Kwon JY, Kang DW, Suh DC, Kim JS, et al. High resolution MRI difference between moyamoya disease and intracranial atherosclerosis. Eur J Neurol. 2013; 20:1311–1318.
Article34. Burke GM, Burke AM, Sherma AK, Hurley MC, Batjer HH, Bendok BR. Moyamoya disease: a summary. Neurosurg Focus. 2009; 26:E11.
Article35. Choi YJ, Jung SC, Lee DH. Vessel wall imaging of the intracranial and cervical carotid arteries. J Stroke. 2015; 17:238–255.
Article36. Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015; 14:640–654.
Article37. Kwon JY, Kim NY, Suh DC, Kang DW, Kwon SU, Kim JS. Intracranial and extracranial arterial dissection presenting with ischemic stroke: lesion location and stroke mechanism. J Neurol Sci. 2015; 358:371–376.
Article38. Maruyama H, Nagoya H, Kato Y, Deguchi I, Fukuoka T, Ohe Y, et al. Spontaneous cervicocephalic arterial dissection with headache and neck pain as the only symptom. J Headache Pain. 2012; 13:247–253.
Article39. Lee SH, Kim KY, Jung JM. High-resolution magnetic resonance imaging for the follow-up of intracranial arterial dissections. Acta Neurol Belg. 2020; Jul. 10. [Epub]. DOI:10.1007/s13760-020-01432-0. Online ahead of print.
Article40. Lee SH, Jung JM, Kim KY, Kim BJ. Intramural hematoma shape and acute cerebral infarction in intracranial artery dissection: a high-resolution magnetic resonance imaging study. Cerebrovasc Dis. 2020; 49:269–276.
Article41. Patel RR, Adam R, Maldjian C, Lincoln CM, Yuen A, Arneja A. Cervical carotid artery dissection: current review of diagnosis and treatment. Cardiol Rev. 2012; 20:145–152.42. Wu Y, Wu F, Liu Y, Fan Z, Fisher M, Li D, et al. High-resolution magnetic resonance imaging of cervicocranial artery dissection: imaging features associated with stroke. Stroke. 2019; 50:3101–3107.43. Wang Y, Lou X, Li Y, Sui B, Sun S, Li C, et al. Imaging investigation of intracranial arterial dissecting aneurysms by using 3 T high-resolution MRI and DSA: from the interventional neuroradiologists’ view. Acta Neurochir (Wien). 2014; 156:515–525.44. Redekop GJ. Extracranial carotid and vertebral artery dissection: a review. Can J Neurol Sci. 2008; 35:146–152.
Article45. Calabrese LH, Dodick DW, Schwedt TJ, Singhal AB. Narrative review: reversible cerebral vasoconstriction syndromes. Ann Intern Med. 2007; 146:34–44.
Article46. Miller TR, Shivashankar R, Mossa-Basha M, Gandhi D. Reversible cerebral vasoconstriction syndrome, part 1: epidemiology, pathogenesis, and clinical course. AJNR Am J Neuroradiol. 2015; 36:1392–1399.
Article47. Miller TR, Shivashankar R, Mossa-Basha M, Gandhi D. Reversible cerebral vasoconstriction syndrome, part 2: diagnostic work-up, imaging evaluation, and differential diagnosis. AJNR Am J Neuroradiol. 2015; 36:1580–1588.
Article48. Swartz RH, Bhuta SS, Farb RI, Agid R, Willinsky RA, Terbrugge KG, et al. Intracranial arterial wall imaging using high-resolution 3-tesla contrast-enhanced MRI. Neurology. 2009; 72:627–634.
Article49. Hajj-Ali RA, Calabrese LH. Diagnosis and classification of central nervous system vasculitis. J Autoimmun. 2014; 48-49:149–152.
Article50. Jung SC, Kang DW, Turan TN. Vessel and vessel wall imaging. Front Neurol Neurosci. 2016; 40:109–123.
Article51. Lindenholz A, van der Kolk AG, Zwanenburg JJM, Hendrikse J. The use and pitfalls of intracranial vessel wall imaging: how we do it. Radiology. 2018; 286:12–28.
Article52. Power S, Matouk C, Casaubon LK, Silver FL, Krings T, Mikulis DJ, et al. Vessel wall magnetic resonance imaging in acute ischemic stroke: effects of embolism and mechanical thrombectomy on the arterial wall. Stroke. 2014; 45:2330–2334.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vessel Wall Imaging of the Intracranial and Cervical Carotid Arteries
- Intracranial Atherosclerosis: From Microscopy to High-Resolution Magnetic Resonance Imaging
- Advances in Fast Vessel-Wall Magnetic Resonance Imaging Using High-Density Coil Arrays
- Acute Stroke Caused by Large Vessel Vasculitis in a Patient with Systemic Lupus Erythematosus
- High-Resolution MRI of Intracranial Atherosclerotic Disease