Anesth Pain Med.
2021 Apr;16(2):196-200. 10.17085/apm.20073.
A comparative study of glottis visualization according to the method of lifting the epiglottis in video laryngoscopy: indirect and direct lifting methods
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Presbyterian Medical Center, Jeonju, Korea
- KMID: 2515547
- DOI: http://doi.org/10.17085/apm.20073
Abstract
- Background
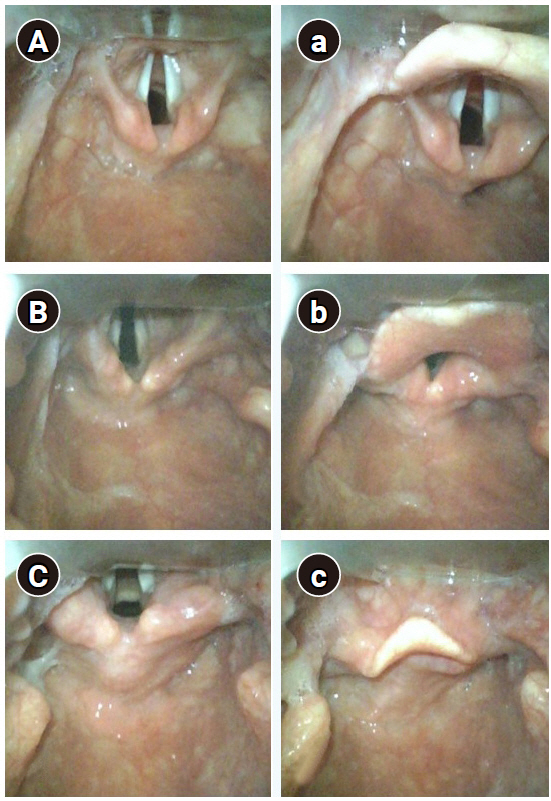
The direct entry of the camera under the epiglottis may provide a better view of the glottis than the indirect lifting of the epiglottis by placing the Macintosh blade tip on the vallecula when using the video laryngoscope. This study aimed to compare the efficiency of two different methods of lifting the epiglottis during the visualization of glottis using video laryngoscopy in the same patient.
Methods
This prospective study enrolled 60 patients who underwent general anesthesia with tracheal intubation. In each patient, glottic views were obtained by directly (group DE) and indirectly lifting the epiglottis (group IE). These two methods were compared using the modified Cormack and Lehane grade and the percentage of glottis opening (POGO) score as assessment parameters.
Results
Modified Cormack and Lehane grade showed a significant difference between the groups DE and IE (P = 0.004). The difference in the POGO score between the groups DE and IE was also statistically significant (87.5% and 64.4%, respectively; P < 0.001).
Conclusions
Our results, therefore, revealed that the method of directly lifting epiglottis was better at exposing glottis than the method of indirectly lifting epiglottis using a video laryngoscope.
Figure
Cited by 1 articles
-
A novel technique of handling the blade for videolaryngoscopy intubation in patients with a semi-rigid neck collar: a prospective randomized controlled trial
Myoung Hwa Kim, Ji Young Kim, Jong Seok Lee, Arim Jo, Do-Hyeong Kim
Korean J Anesthesiol. 2023;76(5):451-460. doi: 10.4097/kja.22733.
Reference
-
1. Macintosh RR. A new laryngoscope. Lancet. 1943; 241:205.2. Cooper RM. Use of a new videolaryngoscope (GlideScope) in the management of a difficult airway. Can J Anaesth. 2003; 50:611–3.3. Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope video laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005; 94:381–4.4. Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005; 52:191–8.5. Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth. 2012; 59:41–52.6. Sakles JC, Mosier J, Chiu S, Cosentino M, Kalin L. A comparison of the C-MAC video laryngoscope to the Macintosh direct laryngoscope for intubation in the emergency department. Ann Emerg Med. 2012; 60:739–48.7. Woo CH, Kim SH, Park JY, Bae JY, Kwak IS, Mun SH, et al. Macintosh laryngoscope vs. Pentax-AWS video laryngoscope: comparison of efficacy and cardiovascular responses to tracheal intubation in major burn patients. Korean J Anesthesiol. 2012; 62:119–24.8. Arulkumaran N, Lowe J, Ions R, Mendoza M, Bennett V, Dunser MW. Videolaryngoscopy versus direct laryngoscopy for emergency orotracheal intubation outside the operating room: a systematic review and meta-analysis. Br J Anaesth. 2018; 120:712–24.9. Liu DX, Ye Y, Zhu YH, Li J, He HY, Dong L, et al. Intubation of non-difficult airways using video laryngoscope versus direct laryngoscope: a randomized, parallel-group study. BMC Anesthesiol. 2019; 19:75.10. Avidan A, Shapira Y, Cohen A, Weissman C, Levin PD. Difficult airway management practice changes after introduction of the GlideScope videolaryngoscope: a retrospective cohort study. Eur J Anaesthesiol. 2020; 37:443–50.11. Yentis SM, Lee DJ. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia. 1998; 53:1041–4.12. Levitan RM, Ochroch EA, Kush S, Shofer FS, Hollander JE. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med. 1998; 5:919–23.13. Nakao H. The Macintosh laryngoscope: the mechanism of laryngeal exposure and the optimal maneuver. J Curr Surg. 2018; 8:1–6.14. Mihai R, Blair E, Kay H, Cook TM. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids. Anaesthesia. 2008; 63:745–60.15. Scott J, Baker PA. How did the Macintosh laryngoscope become so popular? Paediatr Anaesth. 2009; 19 Suppl 1:24–9.16. Gordon JK, Bertram VE, Cavallin F, Parotto M, Cooper RM. Direct versus indirect laryngoscopy using a Macintosh video laryngoscope: a mannequin study comparing applied forces. Can J Anaesth. 2020; 67:515–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The utilization of video laryngoscopy in nasotracheal intubation for oral and maxillofacial surgical procedures: a narrative review
- The use of Pentax-AWS for a difficult airway due to post-thyroidectomy hematoma : A case report
- Severe bradycardia during suspension laryngoscopy performed after tracheal intubation using a direct laryngoscope with a curved blade: A case report
- The Effect of Lifting Speed on Cumulative and Peak Biomechanical Loading for Symmetric Lifting Tasks
- Minimally invasive facial rejuvenation combining thread lifting with liposuction: A clinical comparison with thread lifting alone