J Korean Neurosurg Soc.
2021 May;64(3):437-446. 10.3340/jkns.2020.0236.
The Fate of Proximal Junctional Vertebral Fractures after Long-Segment Spinal Fixation : Are There Predictable Radiologic Characteristics for Revision surgery?
- Affiliations
-
- 1Department of Neurosurgery, Gangnam Severance Hospital, Spine and Spinal Cord Institute, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, the Leon Wiltse Memorial Hospital, Suwon, Korea
- KMID: 2515500
- DOI: http://doi.org/10.3340/jkns.2020.0236
Abstract
Objective
: To investigate the radiographic characteristics of the uppermost instrumented vertebrae (UIV) and UIV+1 compression fractures that are predictive of revision surgery following long-segment spinal fixation.
Methods
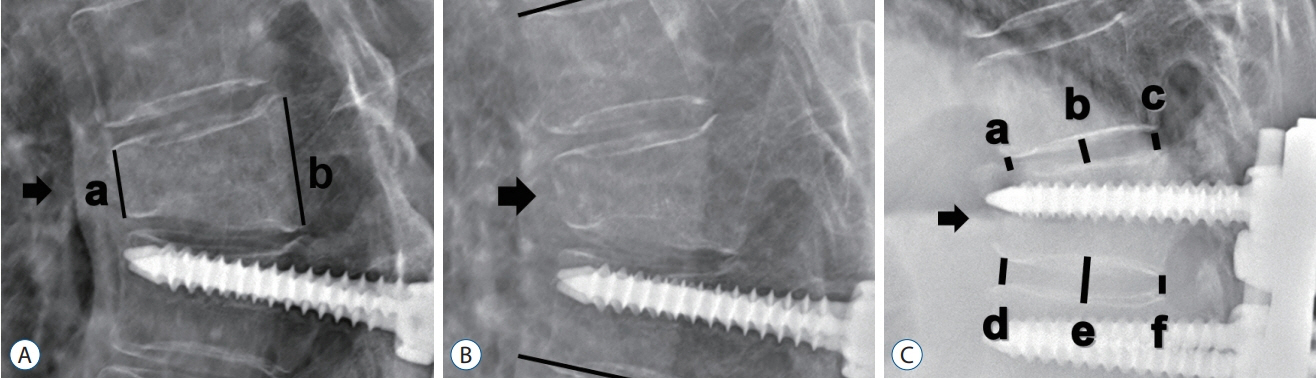
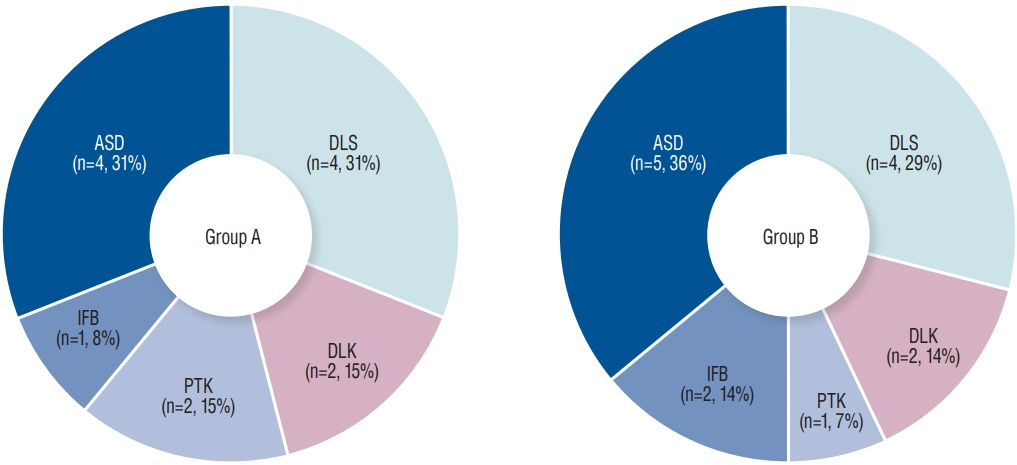
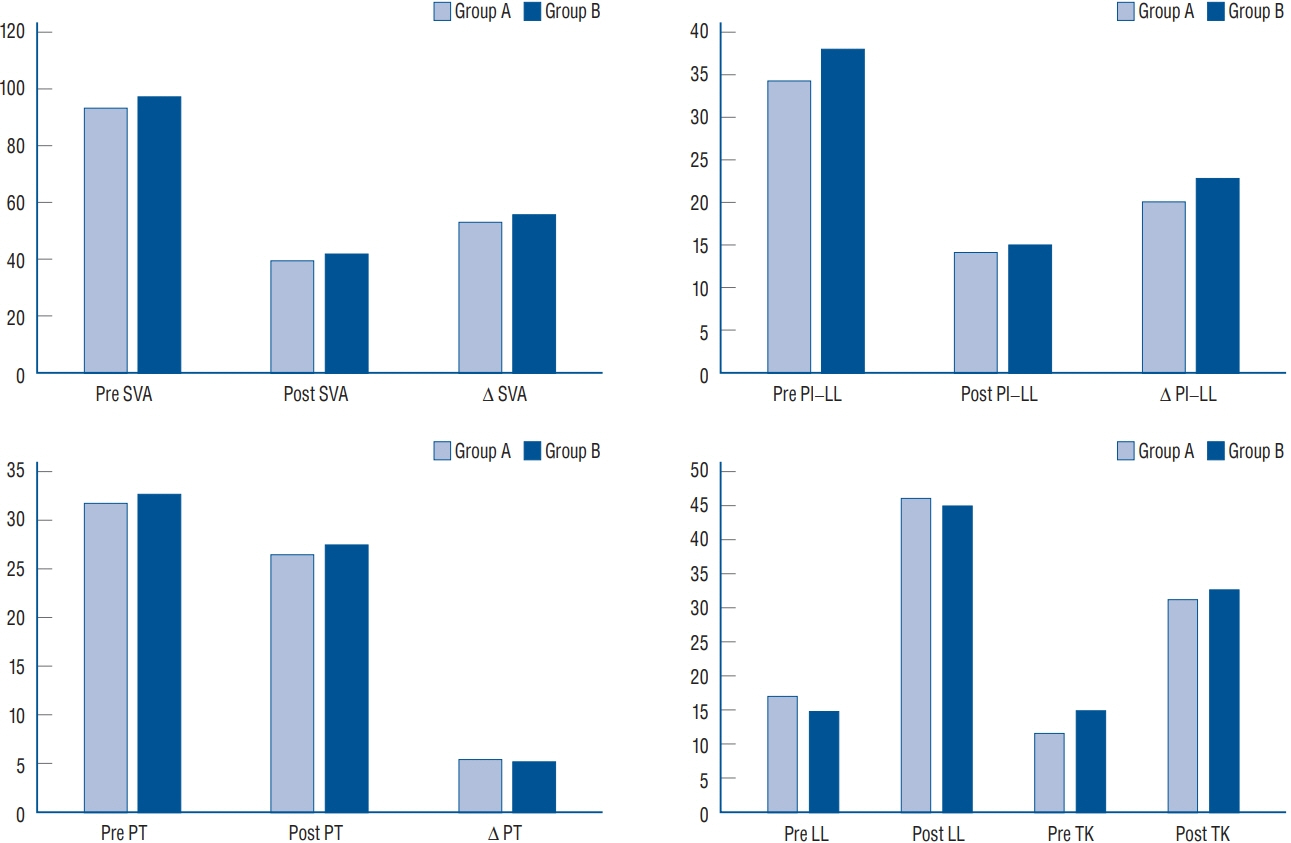
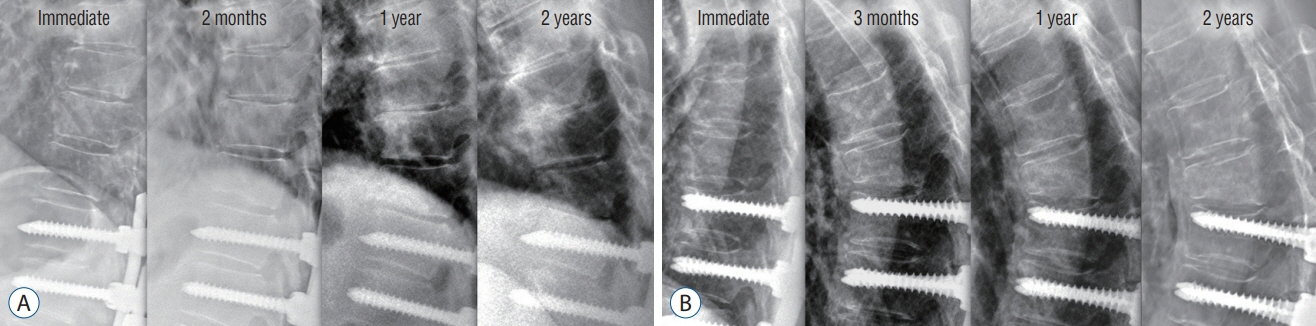
: A total 27 patients who presented newly developed compression fracture at UIV, UIV+1 after long segment spinal fixation (minimum 5 vertebral bodies, lowest instrumented vertebra of L5 or distal) were reviewed retrospectively. Patients were divided into two groups according to following management : revisional surgery (group A, n=13) and conservative care (group B, n=14). Pre- and postoperative images, and images taken shortly before and after the occurrence of fracture were evaluated for radiologic characteristics
Results
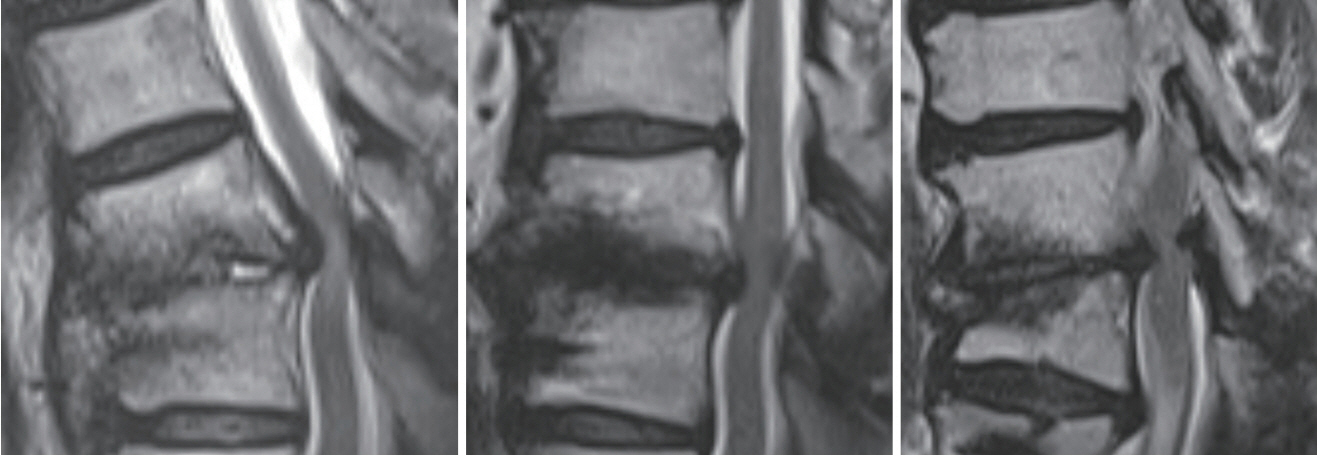
: Despite similar degrees of surgical correction of deformity, the fate of the two groups with proximal junctional compression fractures differed. Immediately after the fracture, the decrement of adjacent disc height in group A (32.3±7.6 mm to 23.7±8.4 mm, Δ=8.5±6.9 mm) was greater than group B (31.0±13.9 mm to 30.1±15.5 mm, Δ=0.9±2.9 mm, p=0.003). Pre-operative magnetic resonance imaging indicated that group A patients have a higher grade of disc degeneration adjacent to fractured vertebrae compared to group B (modified Pfirrmann grade, group A : 6.10±0.99, group B : 4.08±0.90, p=0.004). Binary logistic regression analysis indicated that decrement of disc height was the only associated risk factor for future revision surgery (odds ratio, 1.891; 95% confidence interval, 1.121–3.190; p=0.017).
Conclusion
: Proximal junctional vertebral compression fractures with greater early-stage decrement of adjacent disc height were associated with increased risk of future neurological deterioration and necessity of revision. The condition of adjacent disc degeneration should be considered regarding severity and revision rate of proximal junctional kyphosis/proximal junction failures.
Keyword
Figure
Reference
-
References
1. Bridwell KH, Lenke LG, Cho SK, Pahys JM, Zebala LP, Dorward IG, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery. 72:899–906. 2013.
Article2. Cammarata M, Aubin CÉ, Wang X, Mac-Thiong JM. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976). 39:E500–E507. 2014.3. Choi HY, Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Radiographic and clinical outcomes following pedicle subtraction osteotomy : minimum 2-year follow-up data. J Korean Neurosurg Soc. 63:99–107. 2020.
Article4. Daniels AH, Bess S, Line B, Eltorai AEM, Reid DBC, Lafage V, et al. Peak timing for complications after adult spinal deformity surgery. World neurosurg. 115:e509–e515. 2018.
Article5. Estublier C, Chapurlat R, Szulc P. Older men with severe disc degeneration have more incident vertebral fractures-the prospective MINOS cohort study. Rheumatology (Oxford). 56:37–45. 2017.
Article6. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 86:1497–1503. 2004.
Article7. Glassman SD, Coseo MP, Carreon LY. Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord. 11:1. 2016.
Article8. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 30:1643–1649. 2005.
Article9. Griffith JF, Wang YX, Antonio GE, Choi KC, Yu A, Ahuja AT, et al. Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 32:E708–E712. 2007.
Article10. Han S, Hyun SJ, Kim KJ, Jahng TA, Jeon SI, Wui SH, et al. Effect of vertebroplasty at the upper instrumented vertebra and upper instrumented vertebra +1 for prevention of proximal junctional failure in adult spinal deformity surgery: a comparative matched-cohort study. World Neurosurg. 124:e436–e444. 2019.11. Hart R, McCarthy I, O’brien M, Bess S, Line B, Adjei OB, et al. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine (Phila Pa 1976). 38:E1223–E1227. 2013.
Article12. Hart RA, Rastegar F, Contag A, Kane M, Daniels A, Klineberg E, et al. Inter- and intra-rater reliability of the hart-issg proximal junctional failure severity scale. Spine (Phila Pa 1976). 43:E461–E467. 2018.
Article13. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 4(6 Suppl):190S–194S. 2004.
Article14. Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 14:126–132. 2017.
Article15. Hyun SJ, Rhim SC, Kim YJ, Kim YB. A mid-term follow-up result of spinopelvic fixation using iliac screws for lumbosacral fusion. J Korean Neurosurg Soc. 48:347–353. 2010.
Article16. Kim HJ, Bridwell KH, Lenke LG, Park MS, Song KS, Piyaskulkaew C, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976). 39:E576–E580. 2014.
Article17. Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 33:2179–2184. 2008.
Article18. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976). 31:2359–2366. 2006.
Article19. Lau D, Funao H, Clark AJ, Nicholls F, Smith J, Bess S, et al. The clinical correlation of the Hart-ISSG Proximal Junctional Kyphosis Severity Scale with health-related quality-of-life outcomes and need for revision surgery. Spine (Phila Pa 1976). 41:213–223. 2016.
Article20. Lewis SJ, Abbas H, Chua S, Bacon S, Bronstein Y, Goldstein S, et al. Upper instrumented vertebral fractures in long lumbar fusions: what are the associated risk factors? Spine (Phila Pa 1976). 37:1407–1414. 2012.21. Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 38:E1469–E1476. 2013.
Article22. Nguyen NL, Kong CY, Hart RA. Proximal junctional kyphosis and failure-diagnosis, prevention, and treatment. Curr Rev Musculoskelet Med. 9:299–308. 2016.
Article23. O’Leary PT, Bridwell KH, Lenke LG, Good CR, Pichelmann MA, Buchowski JM, et al. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976). 34:2134–2139. 2009.24. Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. 80:279–286. 2017.
Article25. Phan K, Nazareth A, Hussain AK, Dmytriw AA, Nambiar M, Nguyen D, et al. Relationship between sagittal balance and adjacent segment disease in surgical treatment of degenerative lumbar spine disease: metaanalysis and implications for choice of fusion technique. Eur Spine J. 27:1981–1991. 2018.
Article26. Pollintine P, Dolan P, Tobias JH, Adams MA. Intervertebral disc degeneration can lead to “stress-shielding” of the anterior vertebral body: a cause of osteoporotic vertebral fracture? Spine (Phila Pa 1976). 29:774–782. 2004.
Article27. Shirado O, Kaneda K, Tadano S, Ishikawa H, McAfee PC, Warden KE. Influence of disc degeneration on mechanism of thoracolumbar burst fractures. Spine (Phila Pa 1976). 17:286–292. 1992.
Article28. Smith MW, Annis P, Lawrence BD, Daubs MD, Brodke DS. Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J. 15:2142–2148. 2015.
Article29. Soh J, Lee JC, Shin BJ. Analysis of risk factors for adjacent segment degeneration occurring more than 5 years after fusion with pedicle screw fixation for degenerative lumbar spine. Asian Spine J. 7:273–281. 2013.
Article30. Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Koester L, Hensley M. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine (Phila Pa 1976). 35:138–145. 2010.
Article31. Wui SH, Hyun SJ, Kang B, Kim KJ, Jahng TA, Kim HJ. Bicortical screw purchase at upper instrumented vertebra (UIV) can cause UIV fracture after adult spinal deformity surgery: a finite element analysis study. Neurospine. 17:377–383. 2020.
Article32. Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 37:1479–1489. 2012.
Article33. Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ, et al. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976). 39:E607–E614. 2014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proximal Junctional Kyphosis and Proximal Junctional Failure Following Adult Spinal Deformity Surgery
- A Comparison of Adjacent Segment Diseases Above One Versus Above Two Vertebral Segment after Spinal Fusion of the Degenerative Lumbar Disease
- Impact of Spinal Correction Surgeries with Osteotomy and Pelvic Fixation in Patients with Kyphosis Due to Osteoporotic Vertebral Fractures
- Ligament Augmentation With Mersilene Tape Reduces the Rates of Proximal Junctional Kyphosis and Failure in Adult Spinal Deformity
- Comparison of Short Segment and Long Segment Posterior Instrumentation of Thoracolumbar and Lumbar Bursting Fractures at Load Sharing Score 7 or Above