Intest Res.
2021 Apr;19(2):247-251. 10.5217/ir.2020.00016.
Non-cirrhotic portal hypertension related to azathioprine therapy in a patient with Crohn’s disease
- Affiliations
-
- 1Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Pathology, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2515484
- DOI: http://doi.org/10.5217/ir.2020.00016
Abstract
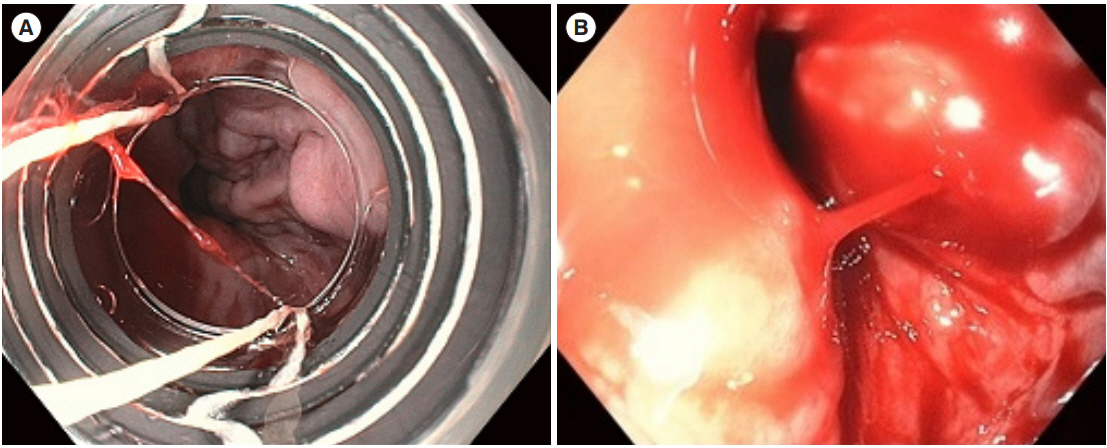
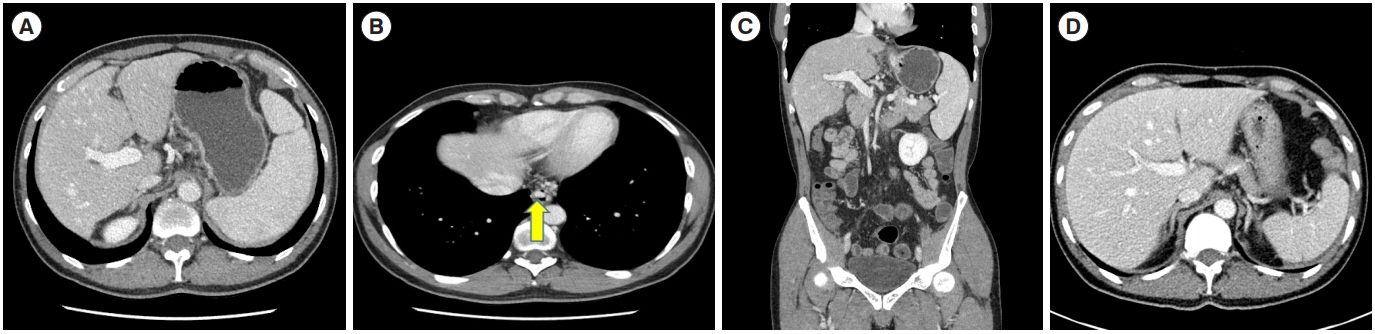
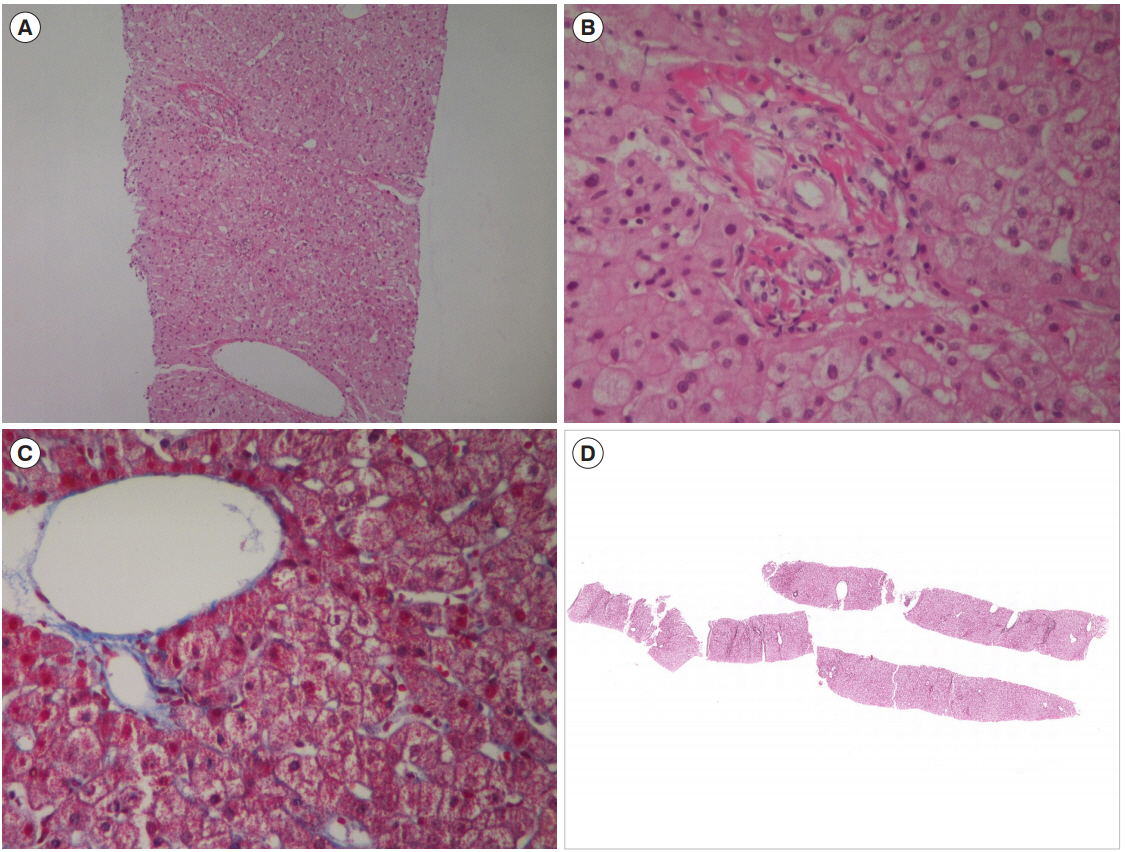
- Azathioprine is widely used for the treatment of Crohn’s disease (CD). Few cases from Western countries have reported idiopathic non-cirrhotic portal hypertension (NCPH) related to thiopurine therapy in patients with inflammatory bowel disease. Idiopathic NCPH is a rare hepatic condition with intrahepatic portal hypertension but no evidence of cirrhosis or chronic liver disease. Patients with idiopathic NCPH present with symptoms of portal hypertension such as thrombocytopenia, splenomegaly and esophageal varices. We report a case of idiopathic NCPH in a 51-year-old male patient with CD who had been taking azathioprine for 5 years. He was admitted due to esophageal variceal bleeding along with splenomegaly and thrombocytopenia. Evaluation of cirrhosis or chronic liver disease showed normal-range results as estimated by FibroScan evaluation, laboratory examination for autoimmune hepatitis or viral hepatitis, and liver biopsy. This case may suggest the need for careful monitoring for manifestations of portal hypertension in Asian patients with inflammatory bowel disease receiving thiopurine treatment.
Figure
Reference
-
1. Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s disease. Lancet. 2017; 389:1741–1755.
Article2. Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017; 152:313–321.
Article3. Pola S, Boland BS, Lin GY, Kuo A, Sandborn WJ. Non-cirrhotic portal hypertension due to 6-mercaptopurine use for Crohn’s disease. Dig Dis Sci. 2014; 59:1642–1644.
Article4. Riggio O, Gioia S, Pentassuglio I, Nicoletti V, Valente M, d’Amati G. Idiopathic noncirrhotic portal hypertension: current perspectives. Hepat Med. 2016; 8:81–88.5. Dooremont D, Decaestecker J, De Wulf D, et al. Azathioprine induced serious portal hypertension: a case series of three IBD patients and review of the literature. Acta Gastroenterol Belg. 2013; 76:342–346.6. Cohen-Ezra O, Avni Y, Morgenstern S, Ben-Ari Z. Nodular regenerative hyperplasia as a complication of thiopurine treatment in a patient with inflammatory bowel disease. Harefuah. 2012; 151:675–721.7. Simsek M, Meijer B, Ramsoekh D, et al. Clinical course of nodular regenerative hyperplasia in thiopurine treated inflammatory bowel disease patients. Clin Gastroenterol Hepatol. 2019; 17:568–570.
Article8. Reshamwala PA, Kleiner DE, Heller T. Nodular regenerative hyperplasia: not all nodules are created equal. Hepatology. 2006; 44:7–14.
Article9. Vernier-Massouille G, Cosnes J, Lemann M, et al. Nodular regenerative hyperplasia in patients with inflammatory bowel disease treated with azathioprine. Gut. 2007; 56:1404–1409.
Article10. Simsek M, Seinen ML, de Boer NKH. Nodular regenerative hyperplasia in inflammatory bowel disease patients with allopurinol-thiopurine cotherapy. Eur J Gastroenterol Hepatol. 2018; 30:1254–1255.
Article11. Musumba CO. Review article: the association between nodular regenerative hyperplasia, inflammatory bowel disease and thiopurine therapy. Aliment Pharmacol Ther. 2013; 38:1025–1037.
Article12. Suárez Ferrer C, Llop Herrera E, Calvo Moya M, et al. Idiopathic portal hypertension regarding thiopurine treatment in patients with inflammatory bowel disease. Rev Esp Enferm Dig. 2016; 108:79–83.
Article13. Fiel MI, Schiano TD. Idiopathic noncirrhotic portal hypertension. Semin Diagn Pathol. 2019; 36:395–403.
Article14. Schouten JN, Garcia-Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011; 54:1071–1081.
Article15. Hernández-Gea V, Baiges A, Turon F, Garcia-Pagán JC. Idiopathic portal hypertension. Hepatology. 2018; 68:2413–2423.
Article16. Sarin SK, Khanna R. Non-cirrhotic portal hypertension. Clin Liver Dis. 2014; 18:451–476.
Article17. Guido M, Sarcognato S, Sacchi D, Colloredo G. Pathology of idiopathic non-cirrhotic portal hypertension. Virchows Arch. 2018; 473:23–31.
Article18. Seiderer J, Zech CJ, Diebold J, et al. Nodular regenerative hyperplasia: a reversible entity associated with azathioprine therapy. Eur J Gastroenterol Hepatol. 2006; 18:553–555.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Azathioprine-Induced Non-Cirrhotic Portal Hypertension in a Patient with Crohn’s Disease
- Balloon Occlusion Retrograde Transvenous Obliteration of Gastric Varices in Two Non-Cirrhotic Patients with Portal Vein Thrombosis
- Unusual Complication of Crohn's Disease: Portal Hypertension Related with Rapid Progression of Portal Vein and Superior Mesenteric Vein Thrombosis
- Determining the Dose of Azathioprine Based on the Lower Limit of Leukocyte Count in Patients with Crohn's Disease
- Management of portal hypertensive gastropathy and other bleeding