Endocrinol Metab.
2021 Apr;36(2):296-311. 10.3803/EnM.2021.958.
An Update on Contraception in Polycystic Ovary Syndrome
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Hacettepe University School of Medicine, Ankara, Turkey
- KMID: 2515456
- DOI: http://doi.org/10.3803/EnM.2021.958
Abstract
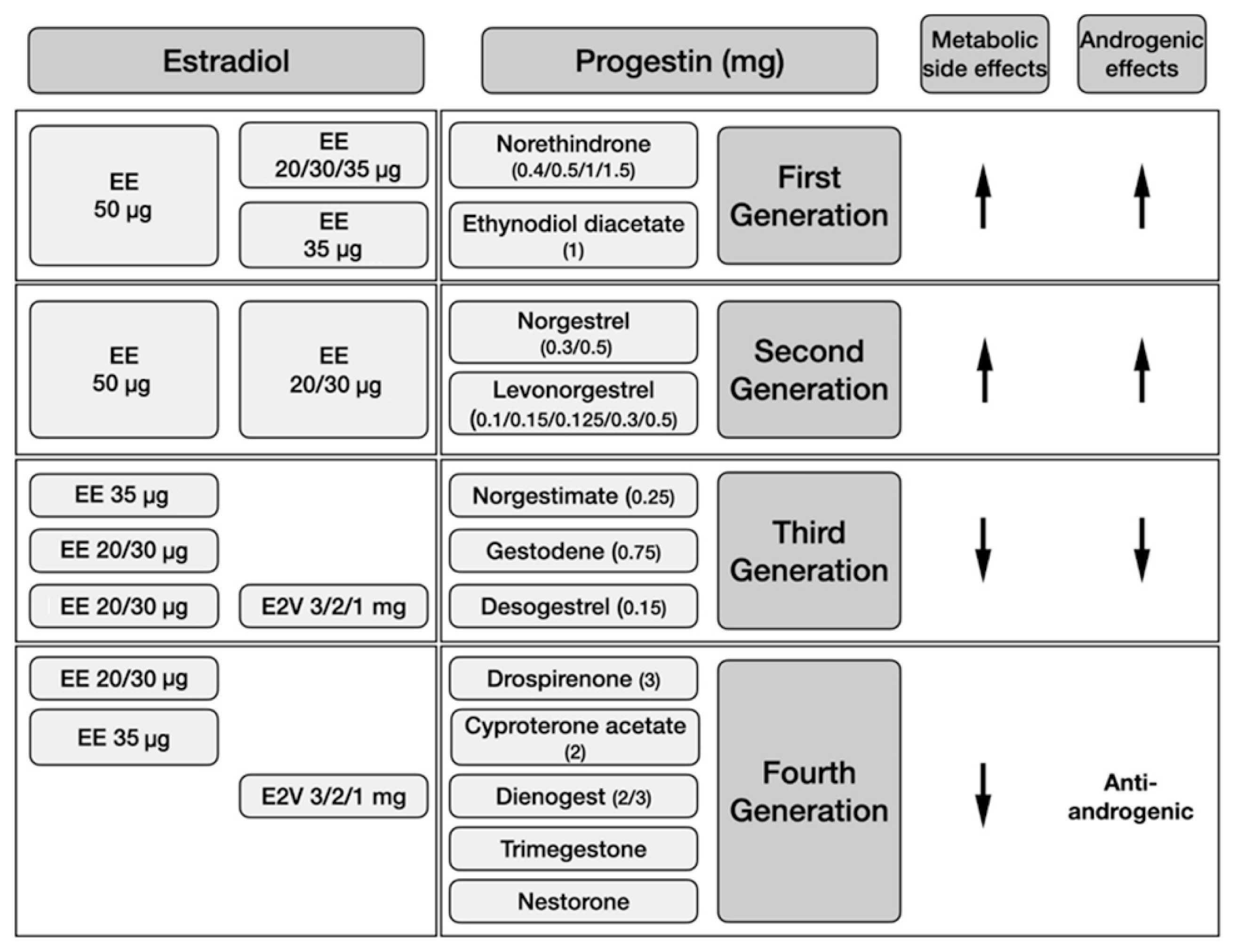
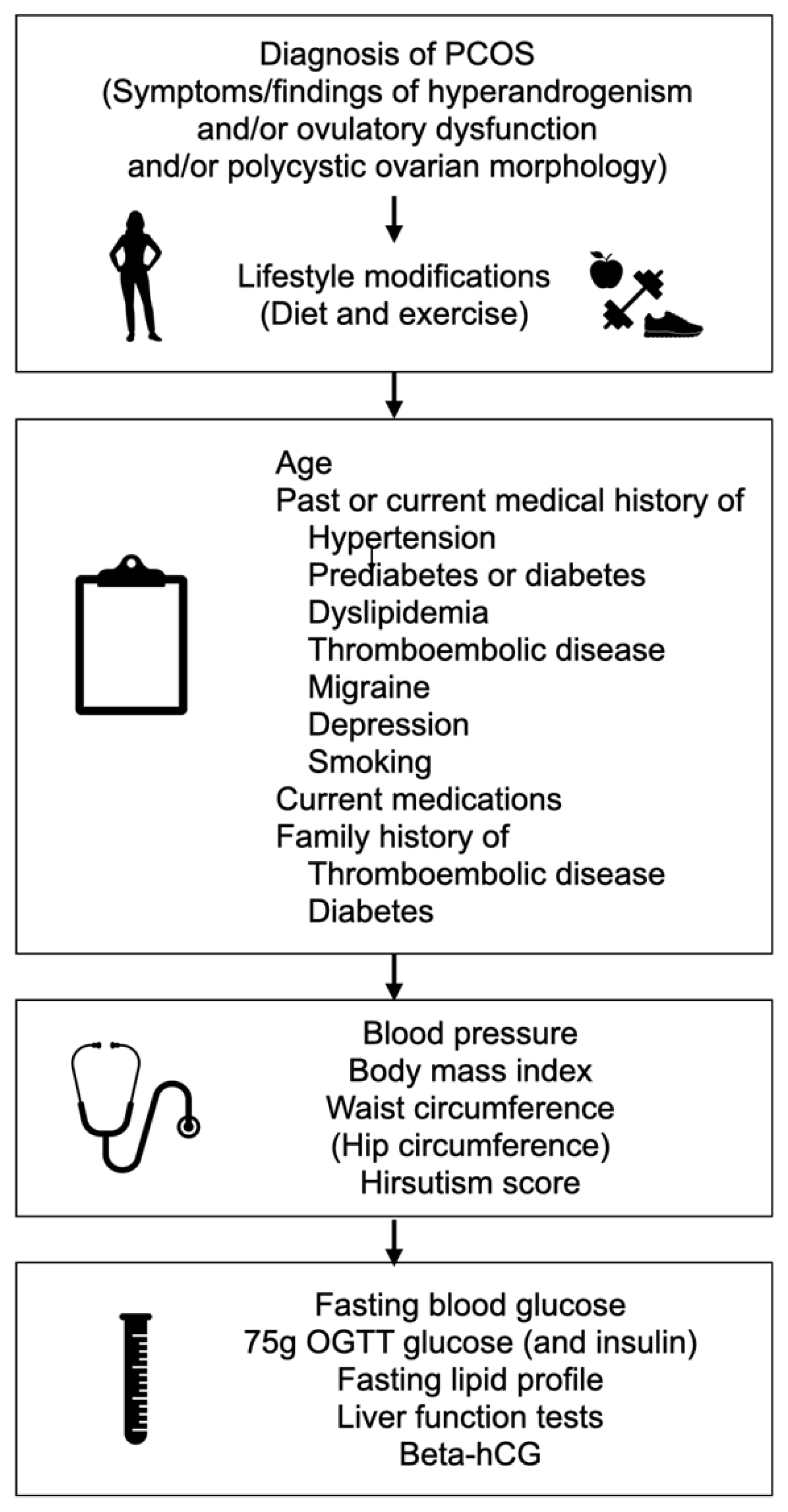
- Polycystic ovary syndrome (PCOS) is a common endocrine disorder in reproductive-aged women, characterized by hyperandrogenism, oligo/anovulation, and polycystic ovarian morphology. Combined oral contraceptives (COCs), along with lifestyle modifications, represent the first-line medical treatment for the long-term management of PCOS. Containing low doses of estrogen and different types of progestin, COCs restore menstrual cyclicity, improve hyperandrogenism, and provide additional benefits such as reducing the risk of endometrial cancer. However, potential cardiometabolic risk associated with these agents has been a concern. COCs increase the risk of venous thromboembolism (VTE), related both to the dose of estrogen and the type of progestin involved. Arterial thrombotic events related to COC use occur much less frequently, and usually not a concern for young patients. All patients diagnosed with PCOS should be carefully evaluated for cardiometabolic risk factors at baseline, before initiating a COC. Age, smoking, obesity, glucose intolerance or diabetes, hypertension, dyslipidemia, thrombophilia, and family history of VTE should be recorded. Patients should be re-assessed at consecutive visits, more closely if any baseline cardiometabolic risk factor is present. Individual risk assessment is the key in order to avoid unfavorable outcomes related to COC use in women with PCOS.
Keyword
Figure
Reference
-
1. Bozdag G, Mumusoglu S, Zengin D, Karabulut E, Yildiz BO. The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2016; 31:2841–55.
Article2. Pincus G, Garcia CR, Rock J, Paniagua M, Pendleton A, Laraque F, et al. Effectiveness of an oral contraceptive; effects of a progestin-estrogen combination upon fertility, menstrual phenomena, and health. Science. 1959; 130:81–3.3. Golobof A, Kiley J. The current status of oral contraceptives: progress and recent innovations. Semin Reprod Med. 2016; 34:145–51.
Article4. Gerstman BB, Piper JM, Tomita DK, Ferguson WJ, Stadel BV, Lundin FE. Oral contraceptive estrogen dose and the risk of deep venous thromboembolic disease. Am J Epidemiol. 1991; 133:32–7.
Article5. De Leo V, Musacchio MC, Cappelli V, Piomboni P, Morgante G. Hormonal contraceptives: pharmacology tailored to women’s health. Hum Reprod Update. 2016; 22:634–46.
Article6. Yildiz BO. Approach to the patient: contraception in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2015; 100:794–802.
Article7. Christin-Maitre S. History of oral contraceptive drugs and their use worldwide. Best Pract Res Clin Endocrinol Metab. 2013; 27:3–12.
Article8. Goebelsmann U, Mashchak CA, Mishell DR Jr. Comparison of hepatic impact of oral and vaginal administration of ethinyl estradiol. Am J Obstet Gynecol. 1985; 151:868–77.
Article9. Sitruk-Ware R, Nath A. Characteristics and metabolic effects of estrogen and progestins contained in oral contraceptive pills. Best Pract Res Clin Endocrinol Metab. 2013; 27:13–24.
Article10. Timmer CJ, Geurts TB. Bioequivalence assessment of three different estradiol formulations in postmenopausal women in an open, randomized, single-dose, 3-way cross-over study. Eur J Drug Metab Pharmacokinet. 1999; 24:47–53.
Article11. Sitruk-Ware R, Nath A. The use of newer progestins for contraception. Contraception. 2010; 82:410–7.
Article12. Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, et al. Classification and pharmacology of progestins. Maturitas. 2008; 61:171–80.
Article13. Oelkers W, Foidart JM, Dombrovicz N, Welter A, Heithecker R. Effects of a new oral contraceptive containing an antimineralocorticoid progestogen, drospirenone, on the renin-aldosterone system, body weight, blood pressure, glucose tolerance, and lipid metabolism. J Clin Endocrinol Metab. 1995; 80:1816–21.
Article14. Hemrika DJ, Slaats EH, Kennedy JC, de Vries Robles-Korsen TJ, Schoemaker J. Pulsatile luteinizing hormone patterns in long term oral contraceptive users. J Clin Endocrinol Metab. 1993; 77:420–6.
Article15. Rivera R, Yacobson I, Grimes D. The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices. Am J Obstet Gynecol. 1999; 181(5 Pt 1):1263–9.
Article16. Fraser IS, Romer T, Parke S, Zeun S, Mellinger U, Machlitt A, et al. Effective treatment of heavy and/or prolonged menstrual bleeding with an oral contraceptive containing estradiol valerate and dienogest: a randomized, double-blind Phase III trial. Hum Reprod. 2011; 26:2698–708.
Article17. Klipping C, Duijkers I, Trummer D, Marr J. Suppression of ovarian activity with a drospirenone-containing oral contraceptive in a 24/4 regimen. Contraception. 2008; 78:16–25.
Article18. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018; 110:364–79.
Article19. Rojanasakul A, Sirimongkolkasem R, Piromsawasdi S, Sumavong V, Chailurkit L, Chaturachinda K. Effects of combined ethinylestradiol and desogestrel on hormone profiles and sex hormone binding globulin in women with polycystic ovarian disease. Contraception. 1987; 36:633–40.
Article20. Stegeman BH, Raps M, Helmerhorst FM, Vos HL, van Vliet HA, Rosendaal FR, et al. Effect of ethinylestradiol dose and progestagen in combined oral contraceptives on plasma sex hormone-binding globulin levels in premenopausal women. J Thromb Haemost. 2013; 11:203–5.
Article21. Martin KA, Anderson RR, Chang RJ, Ehrmann DA, Lobo RA, Murad MH, et al. Evaluation and treatment of hirsutism in premenopausal women: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018; 103:1233–57.
Article22. Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012; 97:28–38.
Article23. Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013; 98:4565–92.
Article24. Conway G, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, Franks S, Gambineri A, et al. The polycystic ovary syndrome: a position statement from the European Society of Endocrinology. Eur J Endocrinol. 2014; 171:P1–29.
Article25. Barrionuevo P, Nabhan M, Altayar O, Wang Z, Erwin PJ, Asi N, et al. Treatment options for hirsutism: a systematic review and network meta-analysis. J Clin Endocrinol Metab. 2018; 103:1258–64.
Article26. Bahamondes L, Valeria Bahamondes M, Shulman LP. Non-contraceptive benefits of hormonal and intrauterine reversible contraceptive methods. Hum Reprod Update. 2015; 21:640–51.
Article27. ESHRE Capri Workshop Group. Noncontraceptive health benefits of combined oral contraception. Hum Reprod Update. 2005; 11:513–25.28. Jensen JT, Parke S, Mellinger U, Machlitt A, Fraser IS. Effective treatment of heavy menstrual bleeding with estradiol valerate and dienogest: a randomized controlled trial. Obstet Gynecol. 2011; 117:777–87.29. Vlahos N, Vlachos A, Triantafyllidou O, Vitoratos N, Creatsas G. Continuous versus cyclic use of oral contraceptives after surgery for symptomatic endometriosis: a prospective cohort study. Fertil Steril. 2013; 100:1337–42.
Article30. Zorbas KA, Economopoulos KP, Vlahos NF. Continuous versus cyclic oral contraceptives for the treatment of endometriosis: a systematic review. Arch Gynecol Obstet. 2015; 292:37–43.
Article31. Schultheis P, Montoya MN, Zhao Q, Archer J, Madden T, Peipert JF. Contraception and ectopic pregnancy risk: a prospective observational analysis. Am J Obstet Gynecol. 2021; 224:228–9.
Article32. Burkman R, Schlesselman JJ, Zieman M. Safety concerns and health benefits associated with oral contraception. Am J Obstet Gynecol. 2004; 190(4 Suppl):S5–22.
Article33. Li C, Zhao WH, Meng CX, Ping H, Qin GJ, Cao SJ, et al. Contraceptive use and the risk of ectopic pregnancy: a multi-center case-control study. PLoS One. 2014; 9:e115031.
Article34. Lanza di Scalea T, Pearlstein T. Premenstrual dysphoric disorder. Med Clin North Am. 2019; 103:613–28.
Article35. Pearlstein TB, Bachmann GA, Zacur HA, Yonkers KA. Treatment of premenstrual dysphoric disorder with a new drospirenone-containing oral contraceptive formulation. Contraception. 2005; 72:414–21.
Article36. Michels KA, Pfeiffer RM, Brinton LA, Trabert B. Modification of the associations between duration of oral contraceptive use and ovarian, endometrial, breast, and colorectal cancers. JAMA Oncol. 2018; 4:516–21.
Article37. Karlsson T, Johansson T, Hoglund J, Ek WE, Johansson A. Time-dependent effects of oral contraceptive use on breast, ovarian and endometrial cancers. Cancer Res. 2021; 81:1153–62.
Article38. Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017; 216:580.39. World Health Organization. Medical eligibility criteria for contraceptive use [Internet]. Geneva: WHO;2015. [cited 2021 Mar 26]. Available from: https://www.who.int/publications/i/item/9789241549158 .40. Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, et al. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016; 65:1–103.
Article41. Heinemann LA, Dinger JC. Range of published estimates of venous thromboembolism incidence in young women. Contraception. 2007; 75:328–36.
Article42. Dragoman MV, Tepper NK, Fu R, Curtis KM, Chou R, Gaffield ME. A systematic review and meta-analysis of venous thrombosis risk among users of combined oral contraception. Int J Gynaecol Obstet. 2018; 141:287–94.
Article43. Kourlaba G, Relakis J, Kontodimas S, Holm MV, Maniadakis N. A systematic review and meta-analysis of the epidemiology and burden of venous thromboembolism among pregnant women. Int J Gynaecol Obstet. 2016; 132:4–10.
Article44. Barsoum MK, Heit JA, Ashrani AA, Leibson CL, Petterson TM, Bailey KR. Is progestin an independent risk factor for incident venous thromboembolism?: a population-based case-control study. Thromb Res. 2010; 126:373–8.
Article45. de Bastos M, Stegeman BH, Rosendaal FR, Van Hylckama Vlieg A, Helmerhorst FM, Stijnen T, et al. Combined oral contraceptives: venous thrombosis. Cochrane Database Syst Rev. 2014; 3:CD010813.
Article46. Practice Committee of the American Society for Reproductive Medicine; Practice Committee of the American Society for Reproductive Medicine. Combined hormonal contraception and the risk of venous thromboembolism: a guideline. Fertil Steril. 2017; 107:43–51.47. van Hylckama Vlieg A, Helmerhorst FM, Vandenbroucke JP, Doggen CJ, Rosendaal FR. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ. 2009; 339:b2921.
Article48. Oedingen C, Scholz S, Razum O. Systematic review and meta-analysis of the association of combined oral contraceptives on the risk of venous thromboembolism: the role of the progestogen type and estrogen dose. Thromb Res. 2018; 165:68–78.
Article49. Dinger J, Do Minh T, Heinemann K. Impact of estrogen type on cardiovascular safety of combined oral contraceptives. Contraception. 2016; 94:328–39.
Article50. Manneras-Holm L, Baghaei F, Holm G, Janson PO, Ohlsson C, Lonn M, et al. Coagulation and fibrinolytic disturbances in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011; 96:1068–76.
Article51. Yildiz BO, Haznedaroglu IC, Kirazli S, Bayraktar M. Global fibrinolytic capacity is decreased in polycystic ovary syndrome, suggesting a prothrombotic state. J Clin Endocrinol Metab. 2002; 87:3871–5.
Article52. Okoroh EM, Hooper WC, Atrash HK, Yusuf HR, Boulet SL. Is polycystic ovary syndrome another risk factor for venous thromboembolism? United States, 2003–2008. Am J Obstet Gynecol. 2012; 207:377.
Article53. Gariani K, Hugon-Rodin J, Philippe J, Righini M, Blondon M. Association between polycystic ovary syndrome and venous thromboembolism: a systematic review and meta-analysis. Thromb Res. 2020; 185:102–8.
Article54. Luque-Ramirez M, Ortiz-Flores AE, Nattero-Chavez L, Escobar-Morreale HF. A safety evaluation of current medications for adult women with the polycystic ovarian syndrome not pursuing pregnancy. Expert Opin Drug Saf. 2020; 19:1559–76.
Article55. Kasapoglu T. Do oral contraceptive pills really protect against venous thromboembolism, especially in polycystic ovary syndrome patients?: prescription bias or not? Am J Obstet Gynecol. 2013; 209:73–4.
Article56. Roach RE, Helmerhorst FM, Lijfering WM, Stijnen T, Algra A, Dekkers OM. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015; 8:CD011054.
Article57. Lidegaard O, Lokkegaard E, Jensen A, Skovlund CW, Keiding N. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med. 2012; 366:2257–66.
Article58. Helvaci N, Yildiz BO. Polycystic ovary syndrome and aging: health implications after menopause. Maturitas. 2020; 139:12–9.
Article59. Wekker V, van Dammen L, Koning A, Heida KY, Painter RC, Limpens J, et al. Long-term cardiometabolic disease risk in women with PCOS: a systematic review and meta-analysis. Hum Reprod Update. 2020; 26:942–60.
Article60. Gunning MN, Fauser BC. Are women with polycystic ovary syndrome at increased cardiovascular disease risk later in life? Climacteric. 2017; 20:222–7.
Article61. Schmidt J, Landin-Wilhelmsen K, Brannstrom M, Dahlgren E. Cardiovascular disease and risk factors in PCOS women of postmenopausal age: a 21-year controlled follow-up study. J Clin Endocrinol Metab. 2011; 96:3794–803.
Article62. Merz CN, Shaw LJ, Azziz R, Stanczyk FZ, Sopko G, Braunstein GD, et al. Cardiovascular disease and 10-year mortality in postmenopausal women with clinical features of polycystic ovary syndrome. J Womens Health (Larchmt). 2016; 25:875–81.
Article63. Meun C, Franco OH, Dhana K, Jaspers L, Muka T, Louwers Y, et al. High androgens in postmenopausal women and the risk for atherosclerosis and cardiovascular disease: the Rotterdam study. J Clin Endocrinol Metab. 2018; 103:1622–30.
Article64. Zhou Y, Wang X, Jiang Y, Ma H, Chen L, Lai C, et al. Association between polycystic ovary syndrome and the risk of stroke and all-cause mortality: insights from a meta-analysis. Gynecol Endocrinol. 2017; 33:904–10.
Article65. Glintborg D, Rubin KH, Nybo M, Abrahamsen B, Andersen M. Cardiovascular disease in a nationwide population of Danish women with polycystic ovary syndrome. Cardiovasc Diabetol. 2018; 17:37.
Article66. Merz CN, Johnson BD, Berga S, Braunstein G, Reis SE, Bittner V, et al. Past oral contraceptive use and angiographic coronary artery disease in postmenopausal women: data from the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation. Fertil Steril. 2006; 85:1425–31.
Article67. Forslund M, Landin-Wilhelmsen K, Trimpou P, Schmidt J, Brannstrom M, Dahlgren E. Type 2 diabetes mellitus in women with polycystic ovary syndrome during a 24-year period: importance of obesity and abdominal fat distribution. Hum Reprod Open. 2020; 2020:hoz042.
Article68. Rubin KH, Glintborg D, Nybo M, Abrahamsen B, Andersen M. Development and risk factors of type 2 diabetes in a nationwide population of women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2017; 102:3848–57.
Article69. Troisi RJ, Cowie CC, Harris MI. Oral contraceptive use and glucose metabolism in a national sample of women in the United States. Am J Obstet Gynecol. 2000; 183:389–95.
Article70. Lopez LM, Grimes DA, Schulz KF. Steroidal contraceptives: effect on carbohydrate metabolism in women without diabetes mellitus. Cochrane Database Syst Rev. 2019; 11:CD006133.
Article71. Halperin IJ, Kumar SS, Stroup DF, Laredo SE. The association between the combined oral contraceptive pill and insulin resistance, dysglycemia and dyslipidemia in women with polycystic ovary syndrome: a systematic review and meta-analysis of observational studies. Hum Reprod. 2011; 26:191–201.
Article72. Luque-Ramirez M, Nattero-Chavez L, Ortiz Flores AE, Escobar-Morreale HF. Combined oral contraceptives and/or antiandrogens versus insulin sensitizers for polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2018; 24:225–41.
Article73. Behboudi-Gandevani S, Ramezani Tehrani F, Hosseinpanah F, Khalili D, Cheraghi L, Kazemijaliseh H, et al. Cardiometabolic risks in polycystic ovary syndrome: long-term population-based follow-up study. Fertil Steril. 2018; 110:1377–86.
Article74. Yildiz BO, Bozdag G, Yapici Z, Esinler I, Yarali H. Prevalence, phenotype and cardiometabolic risk of polycystic ovary syndrome under different diagnostic criteria. Hum Reprod. 2012; 27:3067–73.
Article75. Moran LJ, Misso ML, Wild RA, Norman RJ. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2010; 16:347–63.
Article76. Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020; 35:100937.
Article77. Cagnacci A, Paoletti AM, Renzi A, Orru M, Pilloni M, Melis GB, et al. Glucose metabolism and insulin resistance in women with polycystic ovary syndrome during therapy with oral contraceptives containing cyproterone acetate or desogestrel. J Clin Endocrinol Metab. 2003; 88:3621–5.
Article78. Wang A, Mo T, Li Q, Shen C, Liu M. The effectiveness of metformin, oral contraceptives, and lifestyle modification in improving the metabolism of overweight women with polycystic ovary syndrome: a network meta-analysis. Endocrine. 2019; 64:220–32.
Article79. Amiri M, Ramezani Tehrani F, Nahidi F, Kabir A, Azizi F, Carmina E. Effects of oral contraceptives on metabolic profile in women with polycystic ovary syndrome: a meta-analysis comparing products containing cyproterone acetate with third generation progestins. Metabolism. 2017; 73:22–35.
Article80. Amiri M, Nahidi F, Bidhendi-Yarandi R, Khalili D, Tohidi M, Ramezani Tehrani F. A comparison of the effects of oral contraceptives on the clinical and biochemical manifestations of polycystic ovary syndrome: a crossover randomized controlled trial. Hum Reprod. 2020; 35:175–86.
Article81. Li L, Zhang R, Zeng J, Ke H, Peng X, Huang L, et al. Effectiveness and safety assessment of drospirenone/ethinyl estradiol tablet in treatment of PCOS patients: a single center, prospective, observational study. BMC Womens Health. 2020; 20:39.
Article82. Fields EL, Trent ME. Treatment considerations for the cardiometabolic signs of polycystic ovary syndrome: a review of the literature since the 2013 Endocrine Society clinical practice guidelines. JAMA Pediatr. 2016; 170:502–7.
Article83. Hirschberg AL, Bystrom B, Carlstrom K, von Schoultz B. Reduced serum cholecystokinin and increase in body fat during oral contraception. Contraception. 1996; 53:109–13.
Article84. Arusoglu G, Koksal G, Cinar N, Tapan S, Aksoy DY, Yildiz BO. Basal and meal-stimulated ghrelin, PYY, CCK levels and satiety in lean women with polycystic ovary syndrome: effect of low-dose oral contraceptive. J Clin Endocrinol Metab. 2013; 98:4475–82.
Article85. Naessen S, Carlstrom K, Bystrom B, Pierre Y, Hirschberg AL. Effects of an antiandrogenic oral contraceptive on appetite and eating behavior in bulimic women. Psychoneuroendocrinology. 2007; 32:548–54.
Article86. Gallo MF, Lopez LM, Grimes DA, Carayon F, Schulz KF, Helmerhorst FM. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014; 1:CD003987.
Article87. Lindh I, Ellstrom AA, Milsom I. The long-term influence of combined oral contraceptives on body weight. Hum Reprod. 2011; 26:1917–24.
Article88. Aydin K, Cinar N, Aksoy DY, Bozdag G, Yildiz BO. Body composition in lean women with polycystic ovary syndrome: effect of ethinyl estradiol and drospirenone combination. Contraception. 2013; 87:358–62.
Article89. Pasquali R, Gambineri A, Anconetani B, Vicennati V, Colitta D, Caramelli E, et al. The natural history of the metabolic syndrome in young women with the polycystic ovary syndrome and the effect of long-term oestrogen-progestagen treatment. Clin Endocrinol (Oxf). 1999; 50:517–27.
Article90. Mes-Krowinkel MG, Louwers YV, Mulders AG, de Jong FH, Fauser BC, Laven JS. Influence of oral contraceptives on anthropomorphometric, endocrine, and metabolic profiles of anovulatory polycystic ovary syndrome patients. Fertil Steril. 2014; 101:1757–65.
Article91. Ibanez L, Diaz M, Sebastiani G, Marcos MV, Lopez-Bermejo A, de Zegher F. Oral contraception vs insulin sensitization for 18 months in nonobese adolescents with androgen excess: posttreatment differences in C-reactive protein, intima-media thickness, visceral adiposity, insulin sensitivity, and menstrual regularity. J Clin Endocrinol Metab. 2013; 98:E902–7.92. Harmanci A, Cinar N, Bayraktar M, Yildiz BO. Oral contraceptive plus antiandrogen therapy and cardiometabolic risk in polycystic ovary syndrome. Clin Endocrinol (Oxf). 2013; 78:120–5.
Article93. Shufelt C, LeVee A. Hormonal contraception in women with hypertension. JAMA. 2020; 324:1451–2.
Article94. Skovlund CW, Morch LS, Kessing LV, Lidegaard O. Association of hormonal contraception with depression. JAMA Psychiatry. 2016; 73:1154–62.
Article95. Schaffir J, Worly BL, Gur TL. Combined hormonal contraception and its effects on mood: a critical review. Eur J Contracept Reprod Health Care. 2016; 21:347–55.
Article96. Fruzzetti F, Fidecicchi T. Hormonal contraception and depression: updated evidence and implications in clinical practice. Clin Drug Investig. 2020; 40:1097–106.
Article97. Lundin C, Wikman A, Bixo M, Gemzell-Danielsson K, Sundstrom Poromaa I. Towards individualised contraceptive counselling: clinical and reproductive factors associated with self-reported hormonal contraceptive-induced adverse mood symptoms. BMJ Sex Reprod Health. 2021; Jan. 15. [Epub]. https://doi.org/10.1136/bmjsrh-2020-200658 .
Article98. Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate andcsevere depressive and anxiety symptoms in polycystic ovary syndrome: acsystematic review and meta-analysis. Hum Reprod. 2017; 32:1075–91.99. Cinar N, Harmanci A, Demir B, Yildiz BO. Effect of an oral contraceptive on emotional distress, anxiety and depression of women with polycystic ovary syndrome: a prospective study. Hum Reprod. 2012; 27:1840–5.
Article100. Edwards AC, Lonn SL, Crump C, Moscicki EK, Sundquist J, Kendler KS, et al. Oral contraceptive use and risk of suicidal behavior among young women. Psychol Med. 2020; Oct. 21. [Epub]. https://doi.org/10.1017/S0033291720003475 .
Article101. Dokras A, Sarwer DB, Allison KC, Milman L, Kris-Etherton PM, Kunselman AR, et al. Weight loss and lowering androgens predict improvements in health-related quality of life in women with PCOS. J Clin Endocrinol Metab. 2016; 101:2966–74.
Article102. Yilmaz B, Yildiz BO. Endocrinology of hirsutism: from androgens to androgen excess disorders. Front Horm Res. 2019; 53:108–19.
Article103. Curtis KM, Jatlaoui TC, Tepper NK, Zapata LB, Horton LG, Jamieson DJ, et al. U.S. selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep. 2016; 65:1–66.
Article104. ACOG Practice Bulletin No. 206: use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2019; 133:e128–50.105. Coquoz A, Gruetter C, Stute P. Impact of micronized progesterone on body weight, body mass index, and glucose metabolism: a systematic review. Climacteric. 2019; 22:148–61.
Article106. Kayikcioglu F, Gunes M, Ozdegirmenci O, Haberal A. Effects of levonorgestrel-releasing intrauterine system on glucose and lipid metabolism: a 1-year follow-up study. Contraception. 2006; 73:528–31.
Article107. Morin-Papunen L, Martikainen H, McCarthy MI, Franks S, Sovio U, Hartikainen AL, et al. Comparison of metabolic and inflammatory outcomes in women who used oral contraceptives and the levonorgestrel-releasing intrauterine device in a general population. Am J Obstet Gynecol. 2008; 199:529.
Article108. Kivela A, Ruuskanen M, Agren U, Dieben T. The effects of two progrestogen-only pills containing either desogestrel (75 microgram/day) or levonorgestrel (30 microgram/day) on carbohydrate metabolism and adrenal and thyroid function. Eur J Contracept Reprod Health Care. 2001; 6:71–7.109. Oderich CL, Wender MC, Lubianca JN, Santos LM, de Mello GC. Impact of etonogestrel-releasing implant and copper intrauterine device on carbohydrate metabolism: a comparative study. Contraception. 2012; 85:173–6.
Article110. Villas-Boas J, Vilodre LC, Malerba H, Pontremoli Salcedo M, Foresti Jimenez M, El Beitune P. Metabolic safety of the etonogestrel contraceptive implant in healthy women over a 3-year period. Eur J Obstet Gynecol Reprod Biol. 2016; 202:51–4.
Article111. Biswas A, Viegas OA, Coeling Bennink HJ, Korver T, Ratnam SS. Implanon contraceptive implants: effects on carbohydrate metabolism. Contraception. 2001; 63:137–41.
Article112. Centers for Disease Control and Prevention. Table C1. Classifications for progestin-only contraceptives [Internet]. Atlanta: CDC;2020. [cited 2021 Mar 26]. Available from: https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/appendixc_tablec1.html .113. Grimes DA, Lopez LM, O’Brien PA, Raymond EG. Progestin-only pills for contraception. Cochrane Database Syst Rev. 2013; 11:CD007541.
Article114. Palacios S, Colli E, Regidor PA. Efficacy and cardiovascular safety of the new estrogen-free contraceptive pill containing 4 mg drospirenone alone in a 24/4 regime. BMC Womens Health. 2020; 20:218.115. Zigler RE, McNicholas C. Unscheduled vaginal bleeding with progestin-only contraceptive use. Am J Obstet Gynecol. 2017; 216:443–50.
Article116. Hickey M, Higham JM, Fraser I. Progestogens with or without oestrogen for irregular uterine bleeding associated with anovulation. Cochrane Database Syst Rev. 2012; 9:CD001895.
Article117. Bagis T, Gokcel A, Zeyneloglu HB, Tarim E, Kilicdag EB, Haydardedeoglu B. The effects of short-term medroxyprogesterone acetate and micronized progesterone on glucose metabolism and lipid profiles in patients with polycystic ovary syndrome: a prospective randomized study. J Clin Endocrinol Metab. 2002; 87:4536–40.
Article118. Livadas S, Boutzios G, Economou F, Alexandraki K, Xyrafis X, Christou M, et al. The effect of oral micronized progesterone on hormonal and metabolic parameters in anovulatory patients with polycystic ovary syndrome. Fertil Steril. 2010; 94:242–6.
Article119. Barkfeldt J, Virkkunen A, Dieben T. The effects of two progestogen-only pills containing either desogestrel (75 microg/day) or levonorgestrel (30 microg/day) on lipid metabolism. Contraception. 2001; 64:295–9.
Article120. Clark MK, Dillon JS, Sowers M, Nichols S. Weight, fat mass, and central distribution of fat increase when women use depot-medroxyprogesterone acetate for contraception. Int J Obes (Lond). 2005; 29:1252–8.121. Clark MK, Sowers MR, Nichols S, Levy B. Bone mineral density changes over two years in first-time users of depot medroxyprogesterone acetate. Fertil Steril. 2004; 82:1580–6.
Article122. Meyer C, Talbot M, Teede H. Effect of implanon on insulin resistance in women with polycystic ovary syndrome. Aust N Z J Obstet Gynaecol. 2005; 45:155–8.
Article123. Luukkainen T, Lahteenmaki P, Toivonen J. Levonorgestrel-releasing intrauterine device. Ann Med. 1990; 22:85–90.
Article124. Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost effectiveness of contraceptives in the United States. Contraception. 2009; 79:5–14.
Article125. Mittermeier T, Farrant C, Wise MR. Levonorgestrel-releasing intrauterine system for endometrial hyperplasia. Cochrane Database Syst Rev. 2020; 9:CD012658.
Article126. Seeber B, Ziehr SC, Gschlieber A, Moser C, Mattle V, Seger C, et al. Quantitative levonorgestrel plasma level measurements in patients with regular and prolonged use of the levonorgestrel-releasing intrauterine system. Contraception. 2012; 86:345–9.
Article127. Mandelbaum RS, Ciccone MA, Nusbaum DJ, Khoshchehreh M, Purswani H, Morocco EB, et al. Progestin therapy for obese women with complex atypical hyperplasia: levonorgestrel-releasing intrauterine device vs systemic therapy. Am J Obstet Gynecol. 2020; 223:103.
Article128. Lin M, Xu X, Wang Y, Hu Y, Zhao Y. Evaluation of a levonorgestrel-releasing intrauterine system for treating endometrial hyperplasia in patients with polycystic ovary syndrome. Gynecol Obstet Invest. 2014; 78:41–4.
Article129. Fambrini M, Bargelli G, Peruzzi E, Buccoliero AM, Pieralli A, Andersson KL, et al. Levonorgestrel-releasing intrauterine system alone as primary treatment in young women with early endometrial cancer: case report. J Minim Invasive Gynecol. 2009; 16:630–3.
Article130. Tanmahasamut P, Wongwananuruk T. Challenging regimen for long-term conservative treatment of endometrial adenocarcinoma in young women: a case report and review of the literature. Case Rep Oncol. 2010; 3:380–5.
Article131. Bofill Rodriguez M, Lethaby A, Jordan V. Progestogen-releasing intrauterine systems for heavy menstrual bleeding. Cochrane Database Syst Rev. 2020; 6:CD002126.
Article132. Lethaby A, Wise MR, Weterings MA, Bofill Rodriguez M, Brown J. Combined hormonal contraceptives for heavy menstrual bleeding. Cochrane Database Syst Rev. 2019; 2:CD000154.
Article133. Petta CA, Ferriani RA, Abrao MS, Hassan D, Rosa E, Silva JC, Podgaec S, et al. Randomized clinical trial of a levonorgestrel-releasing intrauterine system and a depot GnRH analogue for the treatment of chronic pelvic pain in women with endometriosis. Hum Reprod. 2005; 20:1993–8.
Article134. Barnett C, Moehner S, Do Minh T, Heinemann K. Perforation risk and intra-uterine devices: results of the EURAS-IUD 5-year extension study. Eur J Contracept Reprod Health Care. 2017; 22:424–8.
Article135. da Silva AV, de Melo AS, Barboza RP, de Paula Martins W, Ferriani RA, Vieira CS. Levonorgestrel-releasing intrauterine system for women with polycystic ovary syndrome: metabolic and clinical effects. Reprod Sci. 2016; 23:877–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical diagnosis and treatment of polycystic ovary syndrome
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome
- Idiopathic Intracranial Hypertension in Patient with Polycystic Ovary Syndromes
- Inter-ovarian differences in ultrasound markers of ovarian size in women with polycystic ovary syndrome
- Diagnosis and Treatment of Polycystic Ovary Syndrome