J Korean Assoc Oral Maxillofac Surg.
2021 Apr;47(2):91-98. 10.5125/jkaoms.2021.47.2.91.
Efficacy of local hyaluronidase administration in guided bone regeneration surgery: a randomized controlled trial
- Affiliations
-
- 1Department of Oral and Periodontology, Section of Dentistry, Seoul National University Bundang Hospital, Seoul, Korea.
- 2Department of Conservative Dentistry, Section of Dentistry, Seoul National University Bundang Hospital, Seoul, Korea.
- 3Biomedical Research Institute, Seoul National University Bundang Hospital, Seoul, Korea.
- 4Department of Oral and Maxillofacial Surgery, Section of Dentistry, Seoul National University Bundang Hospital, Seoul, Korea.
- 5Department of Dentistry and Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea.
- KMID: 2515307
- DOI: http://doi.org/10.5125/jkaoms.2021.47.2.91
Abstract
Objectives
Hyaluronoglucosaminidase (hyaluronidase) increases the local intercellular permeability of the peripheral lymphatic channel and capillaries, which may help reduce edema. In the present study, the effects of hyaluronidase on postoperative edema and pain reduction were evaluated.
Materials and Methods
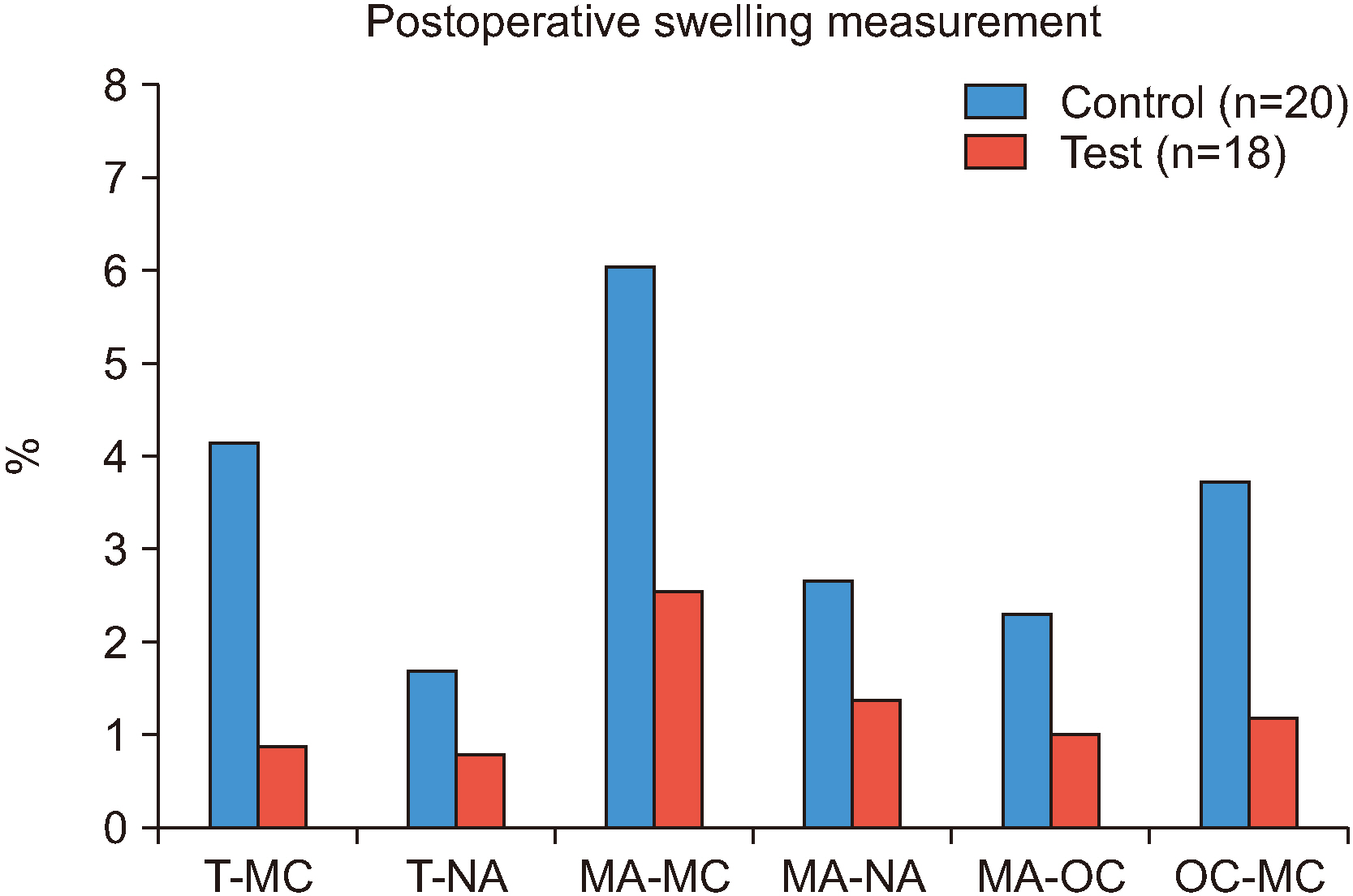
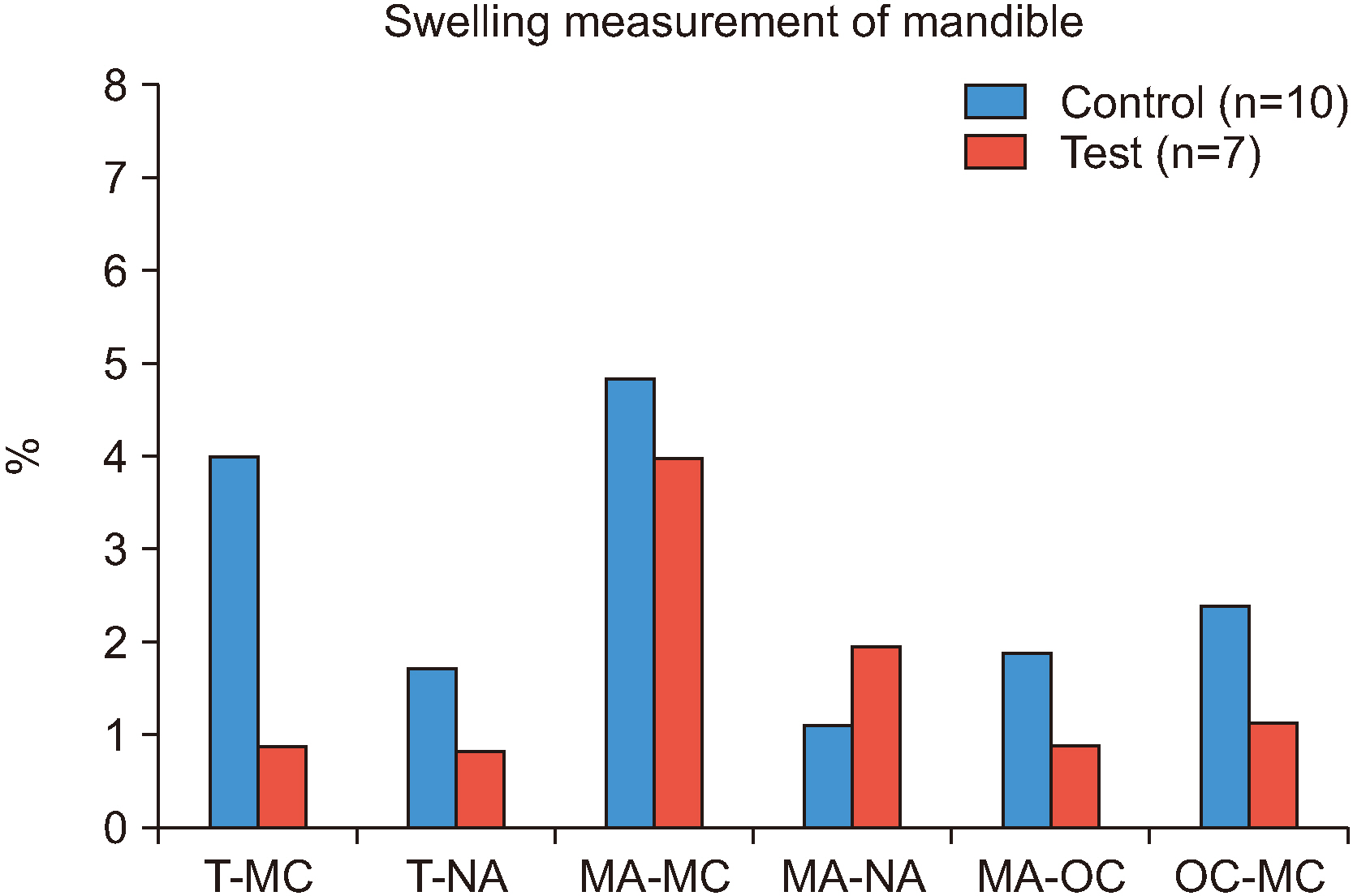
The study included 38 patients who underwent guided bone regeneration (GBR) surgery before implantation. Patients were randomly assigned to either the control group (n=20) or the test group (n=18). Hyaluronidase was injected into the GBR site of subjects in the test group. Postoperative edema was evaluated by measuring the distance between specific facial landmarks immediately after surgery (T1) and 2-4 days after surgery (T2). The degree of pain at T2 and at 10-14 days after surgery (T3) was assessed.
Results
In the test group, the degree of swelling was lower than in the control group, however, only two measurements, from the tragus to the mouth corner and from the outer canthus to the mouth corner, showed statistically significant differences (P=0.012 and P=0.001, respectively). The antiedema effect of hyaluronidase was more effective in the maxilla than in the mandible. In the maxilla, the percentage of facial swelling was significant for three measurements. However, in the mandible, the percentage of facial swelling was significant for only one measurement. Low levels of pain that were similar at T2 and T3 were reported in both groups.
Conclusion
The results indicate the degree of swelling was lower in the test group and hyaluronidase appeared to be more effective in the maxilla. The degree of pain reduction was similar between groups. Further in vivo and randomized controlled trials with larger sample sizes are warranted.
Keyword
Figure
Reference
-
References
1. Cardaropoli G, Araújo M, Lindhe J. 2003; Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol. 30:809–18. https://doi.org/10.1034/j.1600-051x.2003.00366.x . DOI: 10.1034/j.1600-051x.2003.00366.x. PMID: 12956657.
Article2. Araújo MG, Lindhe J. 2005; Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 32:212–8. https://doi.org/10.1111/j.1600-051X.2005.00642.x . DOI: 10.1111/j.1600-051X.2005.00642.x. PMID: 15691354.
Article3. Reich KM, Huber CD, Lippnig WR, Ulm C, Watzek G, Tangl S. 2011; Atrophy of the residual alveolar ridge following tooth loss in an historical population. Oral Dis. 17:33–44. https://doi.org/10.1111/j.1601-0825.2010.01699.x . DOI: 10.1111/j.1601-0825.2010.01699.x. PMID: 20604872.
Article4. Lim G, Lin GH, Monje A, Chan HL, Wang HL. 2018; Wound healing complications following guided bone regeneration for ridge augmentation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 33:41–50. https://doi.org/10.11607/jomi.5581 . DOI: 10.11607/jomi.5581. PMID: 28938030.
Article5. Romanos GE. 2010; Periosteal releasing incision for successful coverage of augmented sites. A technical note. J Oral Implantol. 36:25–30. https://doi.org/10.1563/AAID-JOI-D-09-00068 . DOI: 10.1563/AAID-JOI-D-09-00068. PMID: 20218867.
Article6. Moslemi N, Khorsand A, Torabi S, Shahnaz A, Soleimani Shayesteh Y, Fekrazad R. 2016; Periosteal releasing incision with diode laser in guided bone regeneration procedure: a case series. J Lasers Med Sci. 7:259–64. https://doi.org/10.15171/jlms.2016.46 . DOI: 10.15171/jlms.2016.46. PMID: 28491263. PMCID: PMC5415505.
Article7. Stern S, Lindenhayn K, Schultz O, Perka C. 2000; Cultivation of porcine cells from the nucleus pulposus in a fibrin/hyaluronic acid matrix. Acta Orthop Scand. 71:496–502. https://doi.org/10.1080/000164700317381207 . DOI: 10.1080/000164700317381207. PMID: 11186408.
Article8. Khan N, Niazi ZR, Rehman FU, Akhtar A, Khan MM, Khan S, et al. 2018; Hyaluronidases: a therapeutic enzyme. Protein Pept Lett. 25:663–76. https://doi.org/10.2174/0929866525666180629121823 . DOI: 10.2174/0929866525666180629121823. PMID: 29956608.
Article9. Nekoroski T, Paladini RD, Sauder DN, Frost GI, Keller GA. 2014; A recombinant human hyaluronidase sustained release gel for the treatment of post-surgical edema. Int J Dermatol. 53:777–85. https://doi.org/10.1111/ijd.12304 . DOI: 10.1111/ijd.12304. PMID: 24168080.
Article10. Buhren BA, Schrumpf H, Hoff NP, Bölke E, Hilton S, Gerber PA. 2016; Hyaluronidase: from clinical applications to molecular and cellular mechanisms. Eur J Med Res. 21:5. https://doi.org/10.1186/s40001-016-0201-5 . DOI: 10.1186/s40001-016-0201-5. PMID: 26873038. PMCID: PMC4752759.
Article11. Cerqueira PR, Vasconcelos BC, Bessa-Nogueira RV. 2004; Comparative study of the effect of a tube drain in impacted lower third molar surgery. J Oral Maxillofac Surg. 62:57–61. https://doi.org/10.1016/s0278-2391(03)00675-x . DOI: 10.1016/s0278-2391(03)00675-x. PMID: 14699550.
Article12. Duran-Reynals F. 1933; Studies on a certain spreading factor existing in bacteria and its significance for bacterial invasiveness. J Exp Med. 58:161–81. https://doi.org/10.1084/jem.58.2.161 . DOI: 10.1084/jem.58.2.161. PMID: 19870187. PMCID: PMC2132283.
Article13. Hobby GL, Dawson MH, Meyer K, Chaffee E. 1941; The relationship between spreading factor and hyaluronidase. J Exp Med. 73:109–23. https://doi.org/10.1084/jem.73.1.109 . DOI: 10.1084/jem.73.1.109. PMID: 19871061. PMCID: PMC2135114.
Article14. Fronza M, Muhr C, da Silveira DS, Sorgi CA, Rodrigues SF, Farsky SH, et al. 2016; Hyaluronidase decreases neutrophils infiltration to the inflammatory site. Inflamm Res. 65:533–42. https://doi.org/10.1007/s00011-016-0935-0 . DOI: 10.1007/s00011-016-0935-0. PMID: 26943648.
Article15. Frost GI. 2007; Recombinant human hyaluronidase (rHuPH20): an enabling platform for subcutaneous drug and fluid administration. Expert Opin Drug Deliv. 4:427–40. https://doi.org/10.1517/17425247.4.4.427 . DOI: 10.1517/17425247.4.4.427. PMID: 17683255.
Article16. van Wijk A, Kieffer JM, Lindeboom JH. 2009; Effect of third molar surgery on oral health-related quality of life in the first postoperative week using Dutch version of Oral Health Impact Profile-14. J Oral Maxillofac Surg. 67:1026–31. https://doi.org/10.1016/j.joms.2008.12.041 . DOI: 10.1016/j.joms.2008.12.041. PMID: 19375013.
Article17. Han JH, Kim J, Yoon KC, Shin HW. 2018; Treatment of post-traumatic hematoma and fibrosis using hyaluronidase injection. Arch Craniofac Surg. 19:218–21. https://doi.org/10.7181/acfs.2017.01396 . DOI: 10.7181/acfs.2017.01396. PMID: 30282434. PMCID: PMC6177682.
Article18. Kim JH, Yang H, Oh SH, Song SH, Kyung H. 2019; The efficacy of hyaluronidase in early surgery of nasal bone fracture. J Craniofac Surg. 30:e617–9. https://doi.org/10.1097/SCS.0000000000005646 . DOI: 10.1097/SCS.0000000000005646. PMID: 31261329.
Article19. Koç O, Er N. 2018; Can hyaluronidase be an alternative postoperative anti-edema agent to dexamethasone? Preliminary results of an animal study. J Oral Maxillofac Surg. 76:1653–9. https://doi.org/10.1016/j.joms.2018.03.010 . DOI: 10.1016/j.joms.2018.03.010. PMID: 29654778.
Article20. Amin MM, Laskin DM. 1983; Prophylactic use of indomethacin for prevention of postsurgical complications after removal of impacted third molars. Oral Surg Oral Med Oral Pathol. 55:448–51. https://doi.org/10.1016/0030-4220(83)90227-x . DOI: 10.1016/0030-4220(83)90227-x. PMID: 6575332.
Article21. Chukwuneke FN, Oji C, Saheeb DB. 2008; A comparative study of the effect of using a rubber drain on postoperative discomfort following lower third molar surgery. Int J Oral Maxillofac Surg. 37:341–4. https://doi.org/10.1016/j.ijom.2007.11.016 . DOI: 10.1016/j.ijom.2007.11.016. PMID: 18272338.
Article22. Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. 2011; Validity of four pain intensity rating scales. Pain. 152:2399–404. https://doi.org/10.1016/j.pain.2011.07.005 . DOI: 10.1016/j.pain.2011.07.005. PMID: 21856077.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of submucosal injection of hyaluronidase after mandibular third molar surgery: a randomized controlled trial
- Biologigic membrane for guided bone regeneration
- The Effect On Guided Bone Regeneration Of The Chitosan Membrane
- Hyaluronidase: An overview of its properties, applications, and side effects
- Assessment of clinical and radiographic outcomes of guided bone regeneration with dehydrothermally cross-linked collagen membrane around peri-implant dehiscence defects: Results from a 3-year randomized clinical trial