Korean J Gastroenterol.
2021 Apr;77(4):164-170. 10.4166/kjg.2021.039.
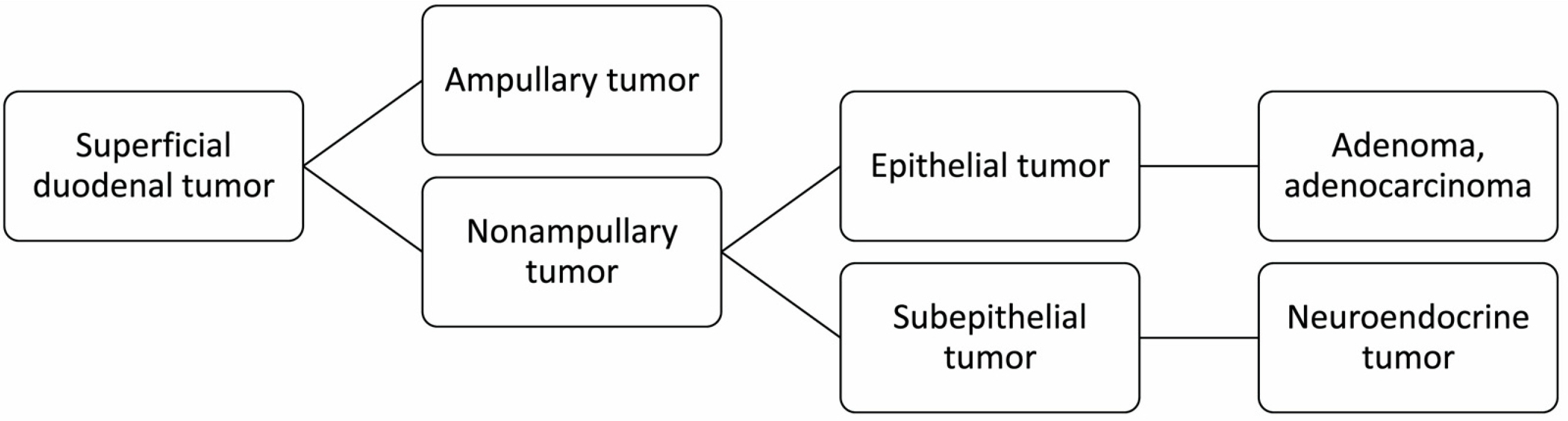
Endoscopic Treatment for Superficial Nonampullary Duodenal Tumors
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2515137
- DOI: http://doi.org/10.4166/kjg.2021.039
Abstract
- Superficial nonampullary duodenal epithelial tumors are considered rare but have been increasingly recognized in recent years. Accordingly, the importance of endoscopic treatment for the lesions are also increasing. An endoscopic resection can be considered for duodenal adenoma and mucosal cancer. The choice of resection method should be made based on the size of the lesion, endoscopic findings, pathologic diagnosis, and risk of procedure-related complication. For small adenomas <10 mm in size, endoscopic mucosal resection (EMR), cold snare polypectomy, and underwater EMR can be considered. An en bloc or piecemeal resection using EMR or underwater EMR can be selected for 10-20 mm sized adenomas. For lesions ≥20 mm in size or suspicious for mucosal cancer, an endoscopic submucosal dissection followed by closure of the mucosal defect conducted by an experienced endoscopist is appropriate.
Figure
Reference
-
1. Kakushima N, Yoshida M, Yabuuchi Y, et al. 2020; Present status of endoscopic submucosal dissection for non-ampullary duodenal epithelial tumors. Clin Endosc. 53:652–658. DOI: 10.5946/ce.2019.184. PMID: 31937098. PMCID: PMC7719431.
Article2. Kim GH, Kim JI, Jeon SW, et al. 2014; Endoscopic resection for duodenal carcinoid tumors: a multicenter, retrospective study. J Gastroenterol Hepatol. 29:318–324. DOI: 10.1111/jgh.12390. PMID: 24117946.
Article3. Goda K, Kikuchi D, Yamamoto Y, et al. 2014; Endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors in Japan: multicenter case series. Dig Endosc. 26 Suppl 2:23–29. DOI: 10.1111/den.12277. PMID: 24750144.
Article4. Okada K, Fujisaki J, Kasuga A, et al. 2011; Sporadic nonampullary duodenal adenoma in the natural history of duodenal cancer: a study of follow-up surveillance. Am J Gastroenterol. 106:357–364. DOI: 10.1038/ajg.2010.422. PMID: 21139577.
Article5. Kakushima N, Ono H, Takao T, Kanemoto H, Sasaki K. 2014; Method and timing of resection of superficial non-ampullary duodenal epithelial tumors. Dig Endosc. 26 Suppl 2:35–40. DOI: 10.1111/den.12259. PMID: 24750146.
Article6. Yoshimizu S, Kawachi H, Yamamoto Y, et al. 2020; Clinicopathological features and risk factors for lymph node metastasis in early-stage non-ampullary duodenal adenocarcinoma. J Gastroenterol. 55:754–762. DOI: 10.1007/s00535-020-01696-6. PMID: 32533301.
Article7. Nonaka S, Oda I, Tada K, et al. 2015; Clinical outcome of endoscopic resection for nonampullary duodenal tumors. Endoscopy. 47:129–135. DOI: 10.1055/s-0034-1390774. PMID: 25314330.
Article8. Kinoshita S, Nishizawa T, Ochiai Y, et al. 2017; Accuracy of biopsy for the preoperative diagnosis of superficial nonampullary duodenal adenocarcinoma. Gastrointest Endosc. 86:329–332. DOI: 10.1016/j.gie.2016.12.007. PMID: 28003118.
Article9. Kakushima N, Yoshida M, Iwai T, et al. 2017; A simple endoscopic scoring system to differentiate between duodenal adenoma and carcinoma. Endosc Int Open. 5:E763–E768. DOI: 10.1055/s-0043-113567. PMID: 28791326. PMCID: PMC5546900.
Article10. Navaneethan U, Hasan MK, Lourdusamy V, Zhu X, Hawes RH, Varadarajulu S. 2016; Efficacy and safety of endoscopic mucosal resection of non-ampullary duodenal polyps: a systematic review. Endosc Int Open. 4:E699–E708. DOI: 10.1055/s-0042-107069. PMID: 27556081. PMCID: PMC4993908.
Article11. Pérez-Cuadrado-Robles E, Quénéhervé L, Margos W, et al. 2018; Comparative analysis of ESD versus EMR in a large european series of non-ampullary superficial duodenal tumors. Endosc Int Open. 6:E1008–E1014. DOI: 10.1055/a-0577-7546. PMID: 30083592. PMCID: PMC6075950.
Article12. Singh A, Siddiqui UD, Konda VJ, et al. 2016; Safety and efficacy of EMR for sporadic, nonampullary duodenal adenomas: a single U.S. center experience (with video). Gastrointest Endosc. 84:700–708. DOI: 10.1016/j.gie.2016.03.1467. PMID: 27063918.13. Tomizawa Y, Ginsberg GG. 2018; Clinical outcome of EMR of sporadic, nonampullary, duodenal adenomas: a 10-year retrospective. Gastrointest Endosc. 87:1270–1278. DOI: 10.1016/j.gie.2017.12.026. PMID: 29317270.
Article14. Klein A, Nayyar D, Bahin FF, et al. 2016; Endoscopic mucosal resection of large and giant lateral spreading lesions of the duodenum: success, adverse events, and long-term outcomes. Gastrointest Endosc. 84:688–696. DOI: 10.1016/j.gie.2016.02.049. PMID: 26975231.
Article15. Inoue T, Uedo N, Yamashina T, et al. 2014; Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc. 26:220–227. DOI: 10.1111/den.12104. PMID: 23621427.
Article16. Kim HK, Chung WC, Lee BI, Cho YS. 2010; Efficacy and long-term outcome of endoscopic treatment of sporadic nonampullary duodenal adenoma. Gut Liver. 4:373–377. DOI: 10.5009/gnl.2010.4.3.373. PMID: 20981216. PMCID: PMC2956351.
Article17. Min YW, Min BH, Kim ER, et al. 2013; Efficacy and safety of endoscopic treatment for nonampullary sporadic duodenal adenomas. Dig Dis Sci. 58:2926–2932. DOI: 10.1007/s10620-013-2708-8. PMID: 23695872.
Article18. Park SM, Ham JH, Kim BW, et al. 2015; Feasibility of endoscopic resection for sessile nonampullary duodenal tumors: a multicenter retrospective study. Gastroenterol Res Pract. 2015:692492. DOI: 10.1155/2015/692492. PMID: 25810715. PMCID: PMC4355118.
Article19. Seo JY, Hong SJ, Han JP, et al. 2014; Usefulness and safety of endoscopic treatment for nonampullary duodenal adenoma and adenocarcinoma. J Gastroenterol Hepatol. 29:1692–1698. DOI: 10.1111/jgh.12601. PMID: 24720570.
Article20. Sohn JW, Jeon SW, Cho CM, et al. 2010; Endoscopic resection of duodenal neoplasms: a single-center study. Surg Endosc. 24:3195–3200. DOI: 10.1007/s00464-010-1114-y. PMID: 20490557.
Article21. Maruoka D, Matsumura T, Kasamatsu S, et al. 2017; Cold polypectomy for duodenal adenomas: a prospective clinical trial. Endoscopy. 49:776–783. DOI: 10.1055/s-0043-107028. PMID: 28493238.
Article22. Hamada K, Takeuchi Y, Ishikawa H, et al. 2016; Feasibility of cold snare polypectomy for multiple duodenal adenomas in patients with familial adenomatous polyposis: a pilot study. Dig Dis Sci. 61:2755–2759. DOI: 10.1007/s10620-016-4165-7. PMID: 27126203.
Article23. Binmoeller KF, Shah JN, Bhat YM, Kane SD. 2013; "Underwater" EMR of sporadic laterally spreading nonampullary duodenal adenomas (with video). Gastrointest Endosc. 78:496–502. DOI: 10.1016/j.gie.2013.03.1330. PMID: 23642790.
Article24. Iwagami H, Takeuchi Y, Yamasaki Y, et al. 2020; Feasibility of underwater endoscopic mucosal resection and management of residues for superficial non-ampullary duodenal epithelial neoplasms. Dig Endosc. 32:565–573. DOI: 10.1111/den.13541. PMID: 31550394.
Article25. Kiguchi Y, Kato M, Nakayama A, et al. 2020; Feasibility study comparing underwater endoscopic mucosal resection and conventional endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumor < 20 mm. Dig Endosc. 32:753–760. DOI: 10.1111/den.13524. PMID: 31498932.26. Shibukawa G, Irisawa A, Sato A, et al. 2018; Endoscopic mucosal resection performed underwater for nonampullary duodenal epithelial tumor: evaluation of feasibility and safety. Gastroenterol Res Pract. 2018:7490961. DOI: 10.1155/2018/7490961. PMID: 30158967. PMCID: PMC6109562.
Article27. Yamasaki Y, Uedo N, Takeuchi Y, et al. 2018; Underwater endoscopic mucosal resection for superficial nonampullary duodenal adenomas. Endoscopy. 50:154–158. DOI: 10.1055/s-0043-119214.
Article28. Bhogal N, Mohan B, Chandan S, et al. 2020; Efficacy and safety of underwater endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumors: a systematic review and meta-analysis. Ann Gastroenterol. 33:379–384. DOI: 10.20524/aog.2020.0504. PMCID: PMC7315707.29. Hoteya S, Furuhata T, Takahito T, et al. 2017; Endoscopic submucosal dissection and endoscopic mucosal resection for non-ampullary superficial duodenal tumor. Digestion. 95:36–42. DOI: 10.1159/000452363. PMID: 28052275.
Article30. Jung JH, Choi KD, Ahn JY, et al. 2013; Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy. 45:133–135. DOI: 10.1055/s-0032-1326178. PMID: 23364841.
Article31. Matsumoto S, Miyatani H, Yoshida Y. 2013; Endoscopic submucosal dissection for duodenal tumors: a single-center experience. Endoscopy. 45:136–137. DOI: 10.1055/s-0032-1310123. PMID: 22930172.
Article32. Yahagi N, Kato M, Ochiai Y, et al. 2018; Outcomes of endoscopic resection for superficial duodenal epithelial neoplasia. Gastrointest Endosc. 88:676–682. DOI: 10.1016/j.gie.2018.05.002. PMID: 29753040.
Article33. Miura Y, Shinozaki S, Hayashi Y, Sakamoto H, Lefor AK, Yamamoto H. 2017; Duodenal endoscopic submucosal dissection is feasible using the pocket-creation method. Endoscopy. 49:8–14. DOI: 10.1055/s-0042-116315. PMID: 27875854.
Article34. Hoteya S, Kaise M, Iizuka T, et al. 2015; Delayed bleeding after endoscopic submucosal dissection for non-ampullary superficial duodenal neoplasias might be prevented by prophylactic endoscopic closure: analysis of risk factors. Dig Endosc. 27:323–330. DOI: 10.1111/den.12377. PMID: 25186455.
Article35. Takimoto K, Imai Y, Matsuyama K. 2014; Endoscopic tissue shielding method with polyglycolic acid sheets and fibrin glue to prevent delayed perforation after duodenal endoscopic submucosal dissection. Dig Endosc. 26 Suppl 2:46–49. DOI: 10.1111/den.12280. PMID: 24750148.
Article36. Akimoto T, Goto O, Nishizawa T, Yahagi N. 2017; Endoscopic closure after intraluminal surgery. Dig Endosc. 29:547–558. DOI: 10.1111/den.12839. PMID: 28181699.
Article37. Nishizawa T, Akimoto T, Uraoka T, et al. 2018; Endoscopic string clip suturing method: a prospective pilot study (with video). Gastrointest Endosc. 87:1074–1078. DOI: 10.1016/j.gie.2017.11.007. PMID: 29154910.38. Yahagi N, Nishizawa T, Akimoto T, Ochiai Y, Goto O. 2016; New endoscopic suturing method: string clip suturing method. Gastrointest Endosc. 84:1064–1065. DOI: 10.1016/j.gie.2016.05.054. PMID: 27327846.
Article39. Kato M, Ochiai Y, Fukuhara S, et al. 2019; Clinical impact of closure of the mucosal defect after duodenal endoscopic submucosal dissection. Gastrointest Endosc. 89:87–93. DOI: 10.1016/j.gie.2018.07.026. PMID: 30055156.
Article40. Tashima T, Ohata K, Sakai E, et al. 2018; Efficacy of an over-the-scope clip for preventing adverse events after duodenal endoscopic submucosal dissection: a prospective interventional study. Endoscopy. 50:487–496. DOI: 10.1055/s-0044-102255. PMID: 29499578.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
- SOX9 Is Highly Expressed in Nonampullary Duodenal Adenoma and Adenocarcinoma in Humans
- A Case of Primary Duodenal Adenocarcinoma Treated by Endoscopic Mucosal Resection
- Clinicopathological features and management strategy for superficial nonampullary duodenal tumors: a multi-center retrospective study
- Efficacy and Long-Term Outcome of Endoscopic Treatment of Sporadic Nonampullary Duodenal Adenoma