Korean J Transplant.
2021 Mar;35(1):53-58. 10.4285/kjt.20.0047.
Acute antibody-mediated rejection limited to medullary lesions in following ABO-incompatible living donor kidney transplantation
- Affiliations
-
- 1Division of Nephrology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 2Department of Pathology, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2514409
- DOI: http://doi.org/10.4285/kjt.20.0047
Abstract
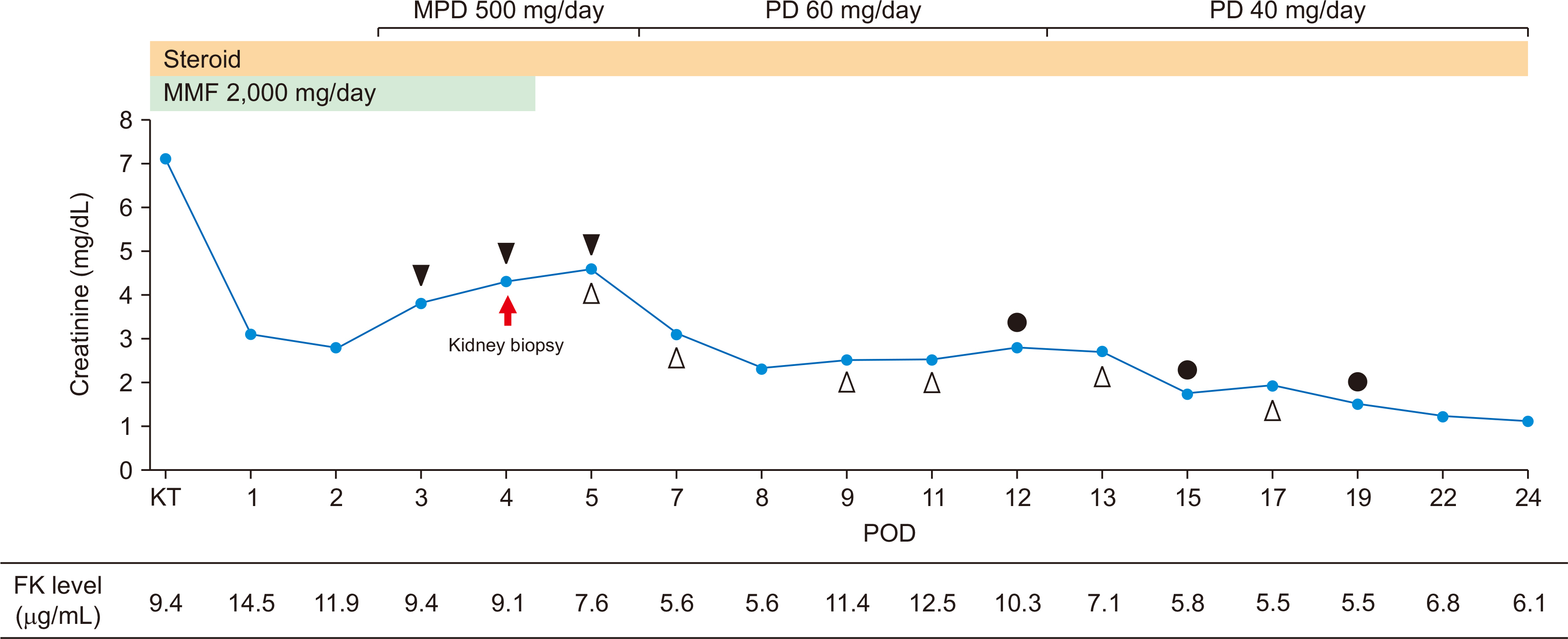
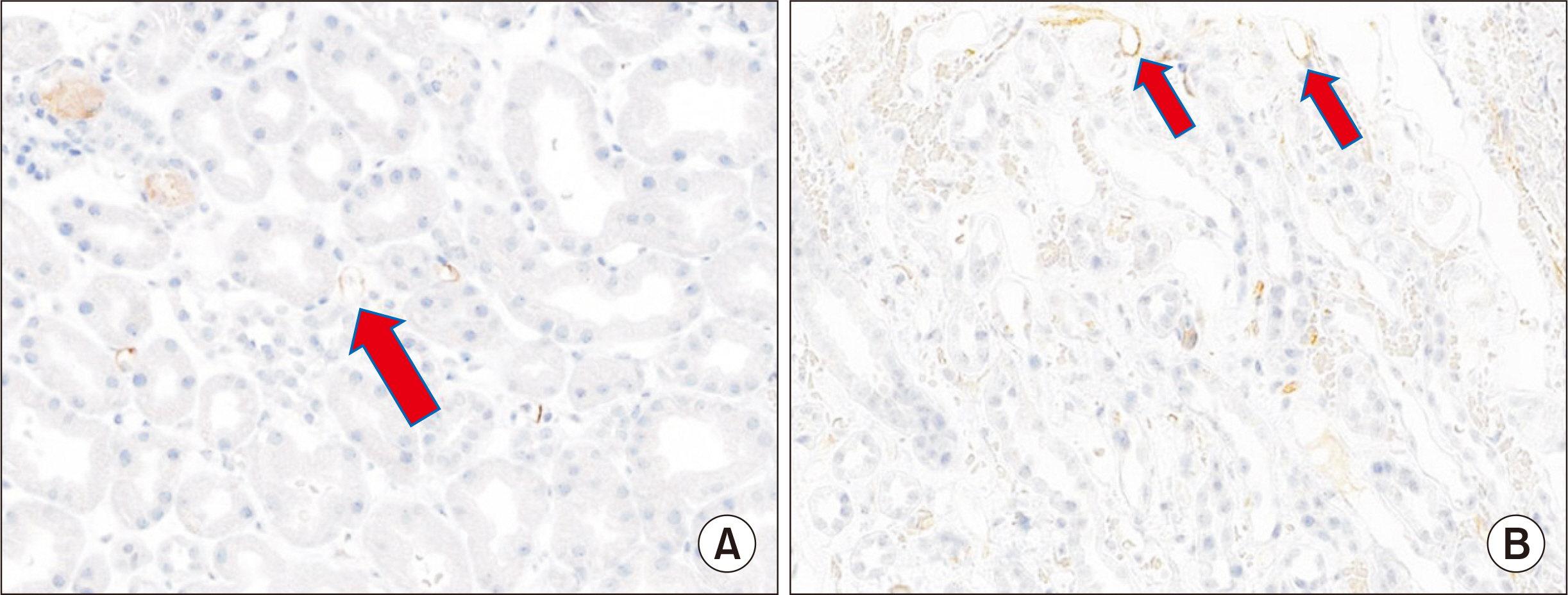
- Anatomical differences between the renal cortex and medulla may influence inflammatory responses. Owing to the difficulty in diagnosing rejections from the medulla, rejection is usually diagnosed through the cortex. However, previous studies have shown that there are no significant differences in renal cortical and medullary lesions in acute allograft rejection. A 60-year-old man with a history of diabetic nephropathy underwent kidney transplant from a living unrelated donor at our hospital in August 2019. Three days after surgery, his urine output suddenly decreased, whereas the serum creatinine levels increased. A kidney biopsy showed only medullary lesions with positive C4d-staining and a Banff score of PTC grade 3. He was diagnosed with acute antibody-mediated rejection (AMR) and treatment was initiated. He did not respond to conventional treatments, including plasma exchange and intravenous immunoglobulin, but his general condition improved after bortezomib administration. There have been a few cases of acute AMR limited to medullary lesions. We consider that rejection cannot be excluded even if the lesions are confined to the medulla.
Figure
Reference
-
1. Bonsib SM, Reznicek MJ, Wright FH. 1989; Renal medulla in the diagnosis of acute cellular rejection. Transplantation. 48:690–2. PMID: 2799925.2. Wang H, Nanra RS, Carney SL, Gillies AH, Hibberd AD, Jones BF, et al. 1995; The renal medulla in acute renal allograft rejection: comparison with renal cortex. Nephrol Dial Transplant. 10:1428–31. PMID: 8538937.3. Visona I, Sementilli A, Kuschnaroff LM, Franco MF. 2015; Medullary nephritis in the diagnosis of acute cellular rejection. Pathol Res Pract. 211:811–5. DOI: 10.1016/j.prp.2015.07.008. PMID: 26296915.
Article4. Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, et al. 1999; The Banff 97 working classification of renal allograft pathology. Kidney Int. 55:713–23. DOI: 10.1046/j.1523-1755.1999.00299.x. PMID: 9987096.5. Shimamura T, Savoca VJ, Cotton J. 1979; Comparative studies of cellular reactions to injuries between the inner medulla and the cortex of rat kidneys. Am J Pathol. 96:143–8. PMID: 380355. PMCID: PMC2042350.6. Andriole VT. 1966; Acceleration of the inflammatory response of the renal medulla by water diuresis. J Clin Invest. 45:847–54. DOI: 10.1172/JCI105400. PMID: 5913294. PMCID: PMC292764.
Article7. Rocha H, Fekety FR Jr. Kass EH, editor. 1965. Delayed granulocyte mobilization in the renal medulla. Progress in pyelonephritis. F.A. Davis Co;Philadelphia, PA: p. 211–20.8. Haas M, Loupy A, Lefaucheur C, Roufosse C, Glotz D, Seron D, et al. 2018; The Banff 2017 Kidney Meeting Report: revised diagnostic criteria for chronic active T cell-mediated rejection, antibody-mediated rejection, and prospects for integrative endpoints for next-generation clinical trials. Am J Transplant. 18:293–307. DOI: 10.1111/ajt.14625. PMID: 29243394. PMCID: PMC5817248.
Article9. Fidler ME, Gloor JM, Lager DJ, Larson TS, Griffin MD, Textor SC, et al. 2004; Histologic findings of antibody-mediated rejection in ABO blood-group-incompatible living-donor kidney transplantation. Am J Transplant. 4:101–7. DOI: 10.1046/j.1600-6135.2003.00278.x. PMID: 14678040.
Article10. Kato M, Morozumi K, Takeuchi O, Oikawa T, Koyama K, Usami T, et al. 2003; Complement fragment C4d deposition in peritubular capillaries in acute humoral rejection after ABO blood group-incompatible human kidney transplantation. Transplantation. 75:663–5. DOI: 10.1097/01.TP.0000053402.87256.6B. PMID: 12640306.
Article11. Takahashi K, Saito K. 2013; ABO-incompatible kidney transplantation. Transplant Rev (Orlando). 27:1–8. DOI: 10.1016/j.trre.2012.07.003. PMID: 22902167.
Article12. Haas M, Rahman MH, Racusen LC, Kraus ES, Bagnasco SM, Segev DL, et al. 2006; C4d and C3d staining in biopsies of ABO- and HLA-incompatible renal allografts: correlation with histologic findings. Am J Transplant. 6:1829–40. DOI: 10.1111/j.1600-6143.2006.01356.x. PMID: 16889542.
Article13. Kanetsuna Y, Yamaguchi Y, Horita S, Tanabe K, Toma H. 2004; C4d and/or immunoglobulins deposition in peritubular capillaries in perioperative graft biopsies in ABO-incompatible renal transplantation. Clin Transplant. 18 Suppl 11:13–7. DOI: 10.1111/j.1399-0012.2004.00241. PMID: 15191367.
Article14. Tobian AA, Shirey RS, Montgomery RA, Cai W, Haas M, Ness PM, et al. 2010; ABO antibody titer and risk of antibody-mediated rejection in ABO-incompatible renal transplantation. Am J Transplant. 10:1247–53. DOI: 10.1111/j.1600-6143.2010.03103.x. PMID: 20420632.
Article15. Everly MJ, Everly JJ, Susskind B, Brailey P, Arend LJ, Alloway RR, et al. 2008; Bortezomib provides effective therapy for antibody- and cell-mediated acute rejection. Transplantation. 86:1754–61. DOI: 10.1097/TP.0b013e318190af83. PMID: 19104417.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful treatment of early acute antibody-mediated rejection in an human leukocyte antigen-incompatible and ABO-incompatible living-donor kidney transplant patient
- The Diagnosis of Acute Antibody-Mediated Rejection in ABO-Incompatible Liver Transplants
- Immunologic strategies and outcomes in ABO-incompatible living donor liver transplantation
- ABO-Incompatible Kidney Transplantation
- ABO-Incompatible Living Donor Liver Transplantation