Clin Endosc.
2021 Mar;54(2):275-279. 10.5946/ce.2020.093.
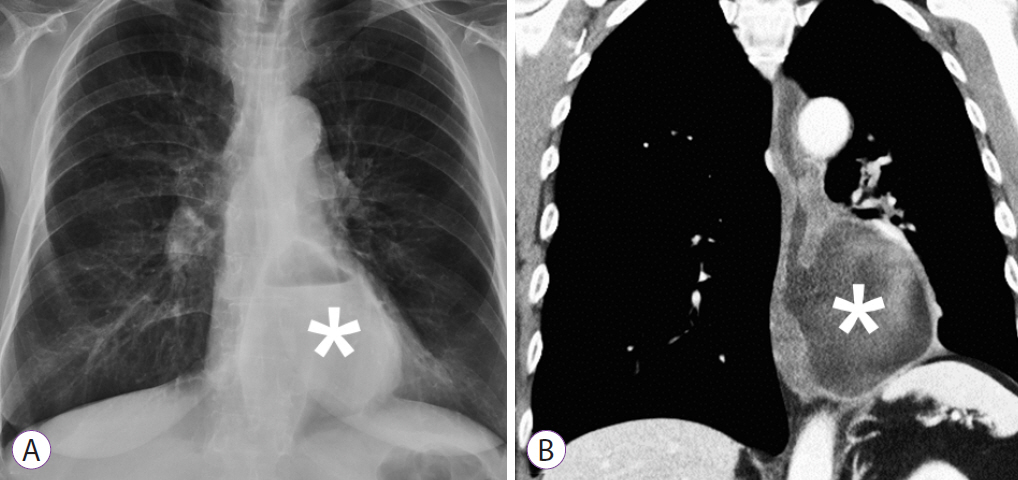
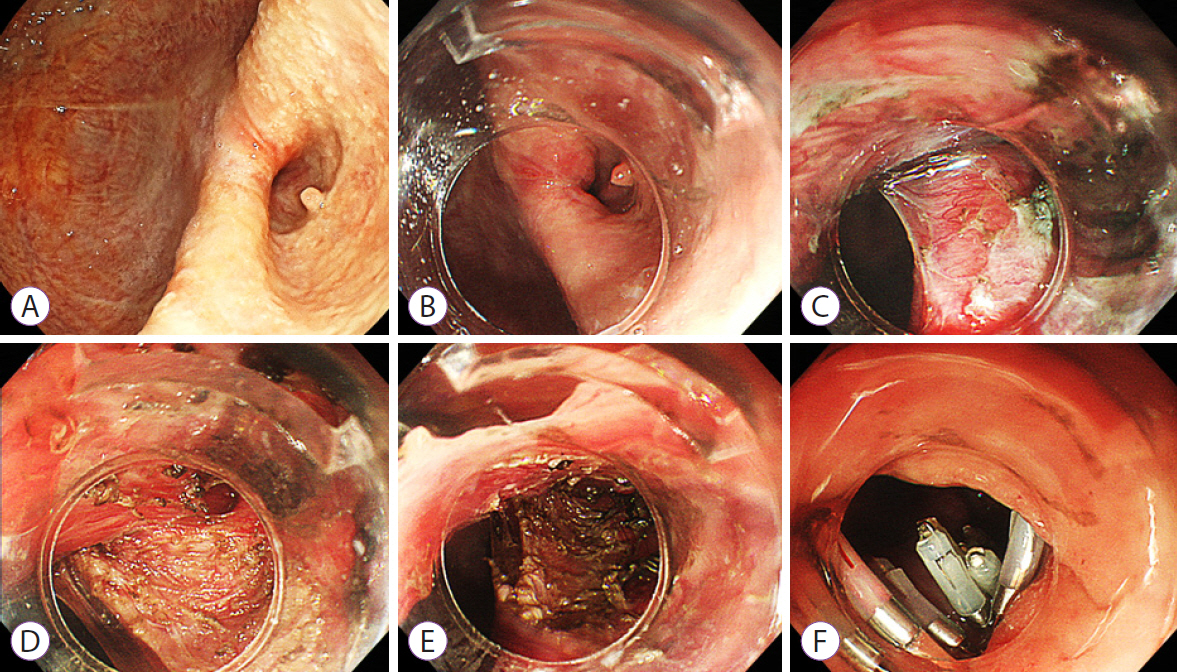
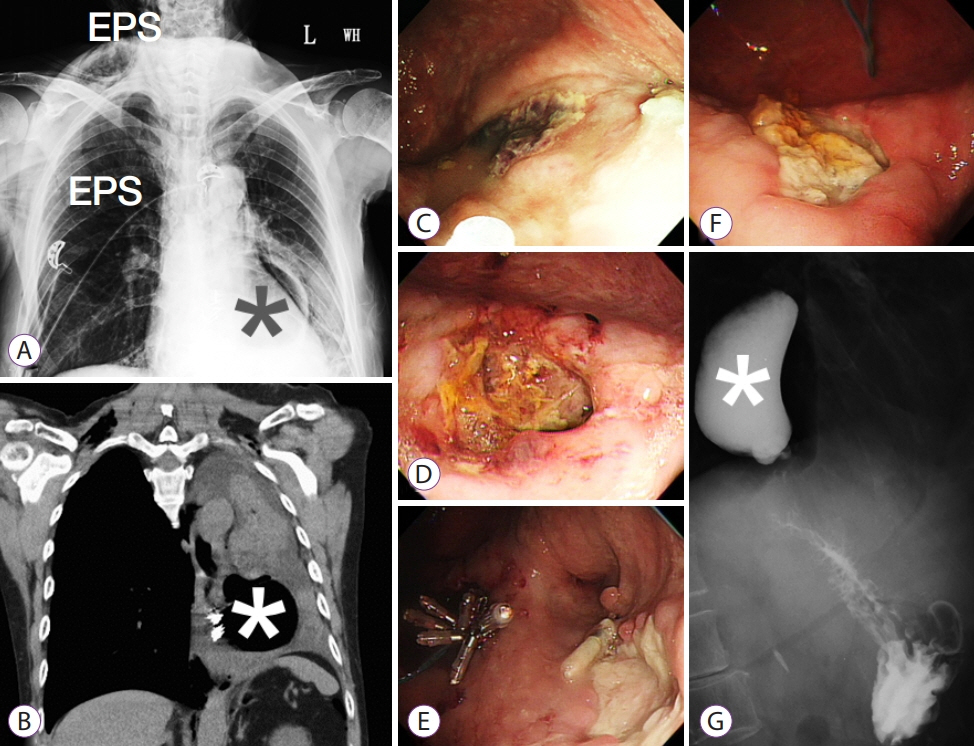
Parapneumonic Effusion and Tension Pneumothorax after Diverticular Peroral Endoscopic Myotomy in a Woman with Large Epiphrenic Diverticulum: A Case Report and Literature Review
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan
- 2Department of Critical Care Medicine, Taichung Veterans General Hospital, Taichung, Taiwan
- 3Evidence-based Practice and Policymaking Committee, Taichung Veterans General Hospital, Taichung, Taiwan
- KMID: 2514184
- DOI: http://doi.org/10.5946/ce.2020.093
Abstract
- Esophageal diverticula (ED) represents a group of rare conditions that warrant intervention when they are symptomatic or coexisting with pulmonary disorders. Few literature reviews have described this patient entity or discussed the postoperative outcome. Therefore, I present the case of a 59-year-old woman with symptoms of dysphagia who was significantly underweight, which was conducive to the diagnosis of symptomatic ED. Because she was a poor candidate for surgery, she received a diverticular peroral endoscopic myotomy. She subsequently developed parapneumonic effusion and tension pneumothorax after the procedure. She was finally discharged on postoperative day 23. I also performed the first known comprehensive literature review of 34 published cases (including my patient) from PubMed and have addressed the demography, intervention, and prognosis for symptomatic ED after the procedure. Prompt treatment as well as prognostic measurement are crucial to successful outcomes.
Keyword
Figure
Reference
-
1. Soares R, Herbella FA, Prachand VN, Ferguson MK, Patti MG. Epiphrenic diverticulum of the esophagus. From pathophysiology to treatment. J Gastrointest Surg. 2010; 14:2009–2015.
Article2. Thomas ML, Anthony AA, Fosh BG, Finch JG, Maddern GJ. Oesophageal diverticula. Br J Surg. 2001; 88:629–642.
Article3. Hoghooghi D, Coakley FV, Breiman RS, Qayyum A, Yeh BM. Frequency and etiology of midesophageal diverticula at barium esophagography. Clin Imaging. 2006; 30:245–247.
Article4. Fisichella PM, Jalilvand A, Dobrowolsky A. Achalasia and epiphrenic diverticulum. World J Surg. 2015; 39:1614–1619.
Article5. Herbella FAM, Patti MG. Achalasia and epiphrenic diverticulum. World J Surg. 2015; 39:1620–1624.
Article6. Eubanks TR, Pellegrini CA. Minimally invasive treatment of esophageal diverticula. Semin Thorac Cardiovasc Surg. 1999; 11:363–367.
Article7. Chan DSY, Foliaki A, Lewis WG, Clark GWB, Blackshaw G. Systematic review and meta-analysis of surgicaltreatment of non-Zenker’s oesophageal diverticula. J Gastrointest Surg. 2017; 21:1067–1075.
Article8. Yang J, Zeng X, Yuan X, et al. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019; 51:346–349.
Article9. Bhalla S, Reddy CA, Watts L, Chang AC, Law R. Greater-curvature peroral endoscopic myotomy with diverticuloseptotomy for the treatment of achalasia in a patient with a large epiphrenic diverticulum. VideoGIE. 2020; 5:77–79.10. Kinoshita M, Tanaka S, Kawara F, et al. Peroral endoscopic myotomy alone is effective for esophageal motility disorders and esophageal epiphrenic diverticulum: a retrospective single-center study. Surg Endosc. 2020; 34:5447–5454.
Article11. Fernando HC, Luketich JD, Samphire J, et al. Minimally invasive operation for esophageal diverticula. Ann Thorac Surg. 2005; 80:2076–2080.
Article12. Manolakis AC, Inoue H, Ueno A, Shimamura Y. 2007-2019: a “Third”- space odyssey in the endoscopic management of gastrointestinal tract diseases. Curr Treat Options Gastroenterol. 2019; 17:202–220.13. Sato H, Takeuchi M, Hashimoto S, et al. Esophageal diverticulum: new perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol. 2019; 25:1457–1464.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of EndoFLIP in Diverticular Peroral Endoscopic Myotomy for Symptomatic Epiphrenic Diverticulum
- Esophageal Diverticulum
- A rare complication: Tension pneumothorax after peroral endoscopic myotomy
- A Case of Dysphagia with Epiphrenic Diverticulum
- Role of Peroral Endoscopic Myotomy (POEM) in the Management of Esophageal Diverticula