J Rheum Dis.
2021 Apr;28(2):101-106. 10.4078/jrd.2021.28.2.101.
A Patient With Late-onset Limb-girdle Muscular Dystrophy Type 2B Mimicking Dermatomyositis: A Case Report and Review
- Affiliations
-
- 1Division of Rheumatology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- 3Department of Neurology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 4Department of Pathology, Seoul National University College of Medicine, Seoul, Korea
- 5Clinical Research Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 6Department of Pediatrics, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2514121
- DOI: http://doi.org/10.4078/jrd.2021.28.2.101
Abstract
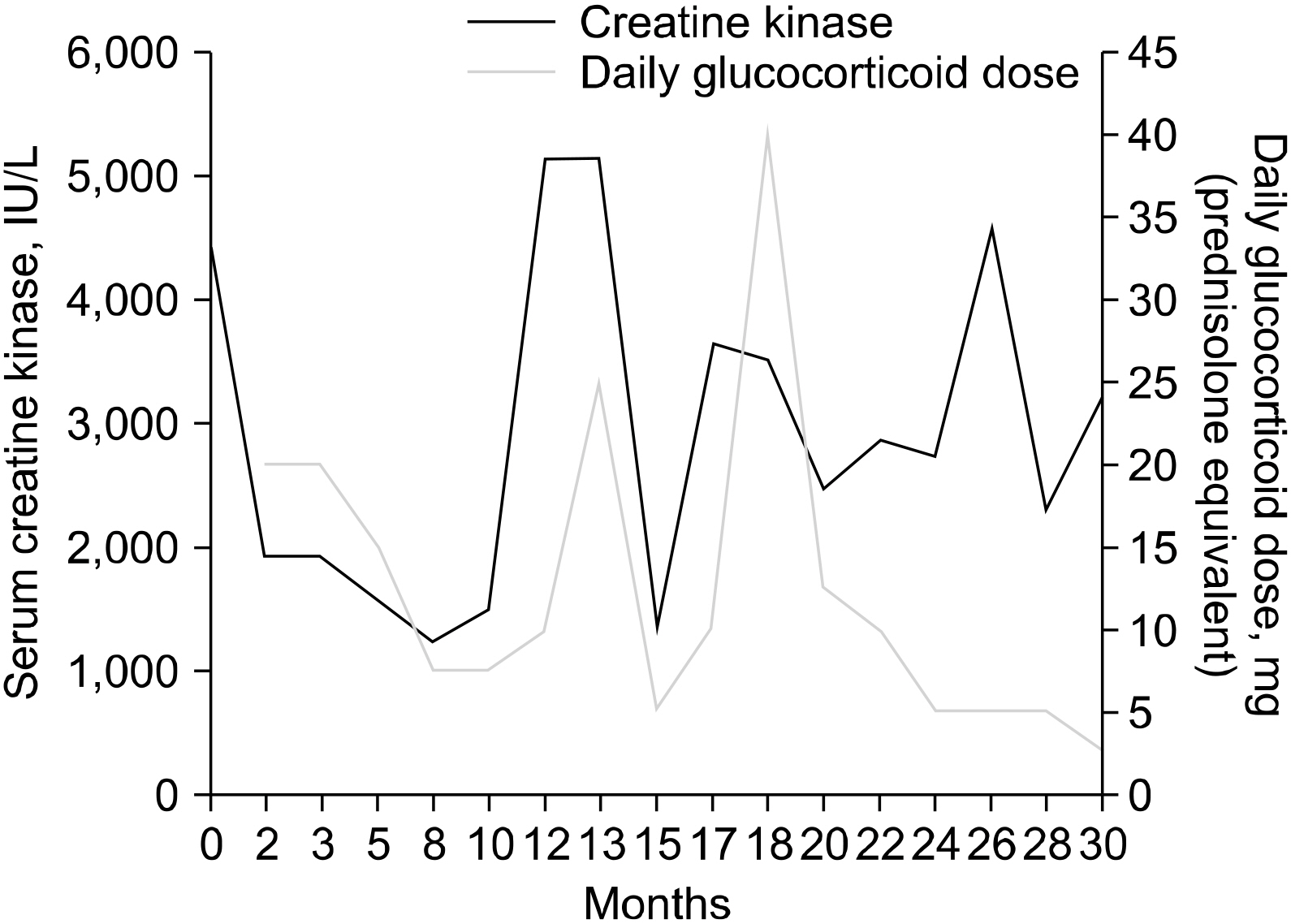
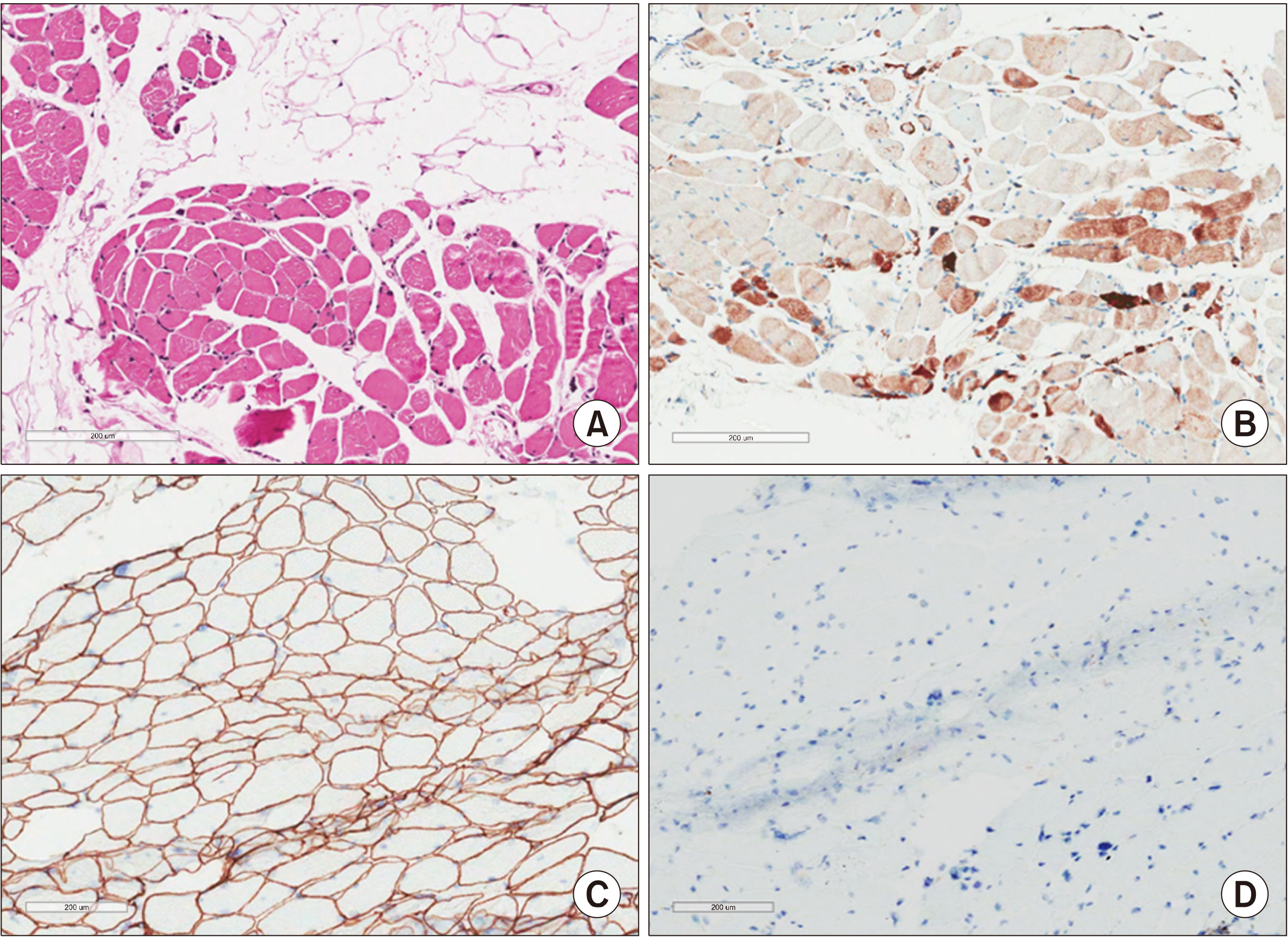
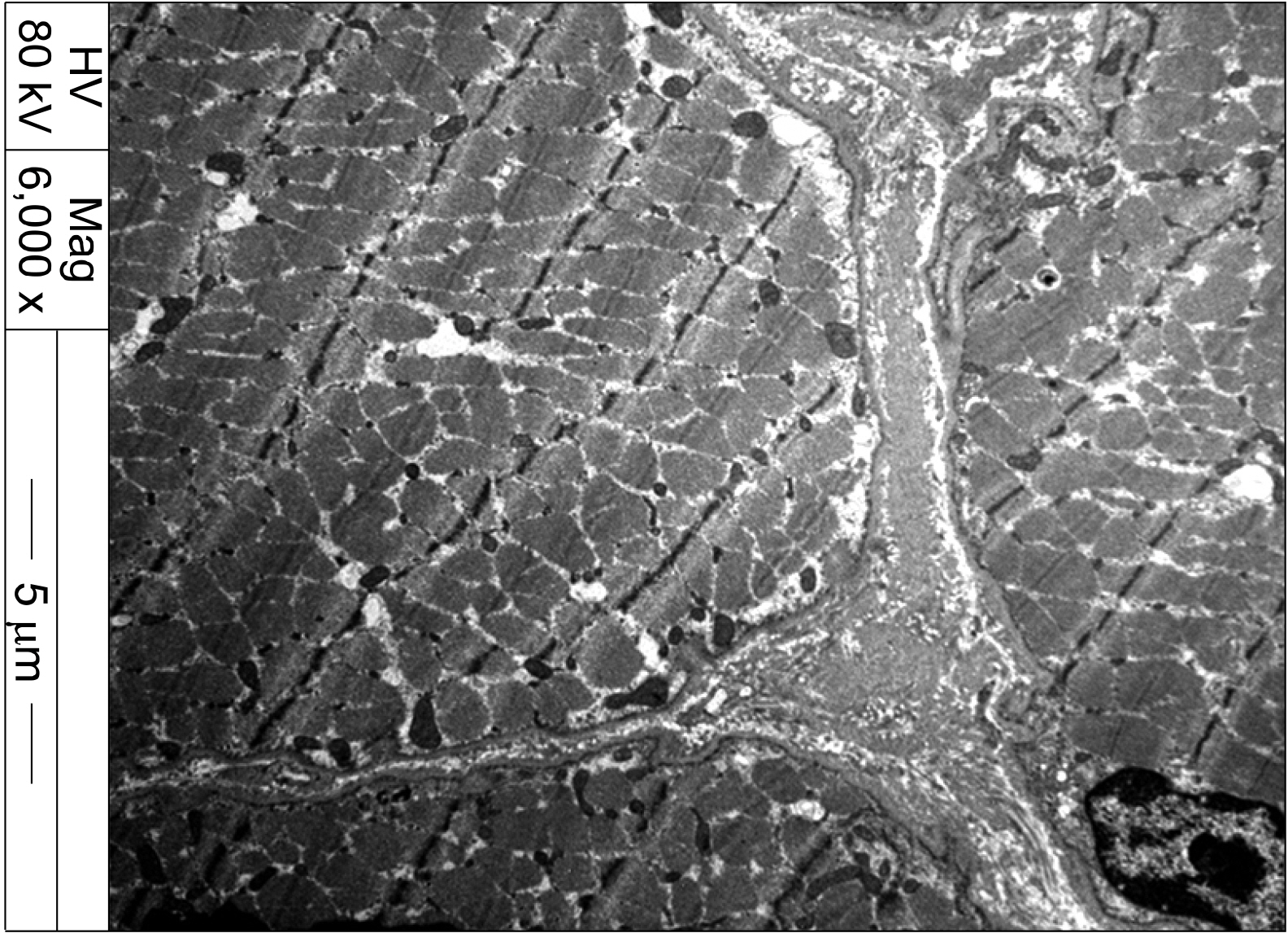
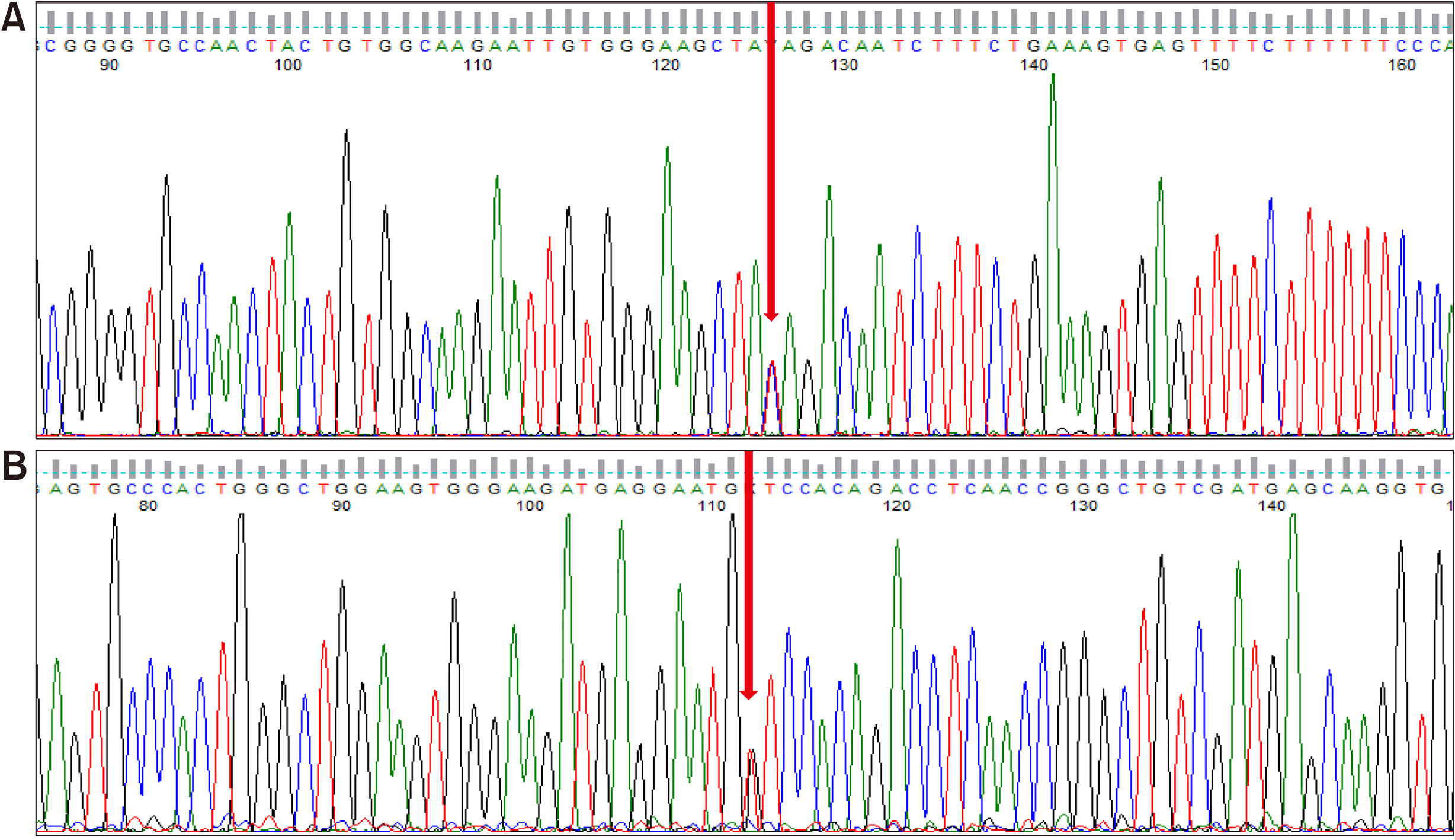
- Limb-Girdle Muscular Dystrophy 2B (LGMD2B) presents with proximal and/or distal muscle weakness and markedly high creatine kinase level. It is caused by the loss of dysferlin due to mutations in the DYSF gene. Due to its similar clinical features as inflammatory myopathy, it is often difficult to distinguish between the two. We present a case of a 48-year-old male who developed progressive proximal muscle weakness, papulosquamous lesions on the knuckles, elevated levels of muscle enzymes, and electromyogram abnormalities. Based on the clinical presentation, the initial impression was dermatomyositis, yet it was refractory to immunosuppressive therapy. Subsequently, dysferlin immunostaining and genetic analysis led to the final diagnosis of LGMD2B. This case shows that LGMD2B can present with extramuscular symptoms mimicking inflammatory myopathy in later stages of life. Dysferlin immunostaining and/or genetic analysis of the DYSF gene are essential for its diagnosis.
Keyword
Figure
Reference
-
1. Dalakas MC. 2015; Inflammatory muscle diseases. N Engl J Med. 372:1734–47. DOI: 10.1056/NEJMra1402225. PMID: 25923553.
Article2. Bohan A, Peter JB. 1975; Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 292:344–7. DOI: 10.1056/NEJM197502132920706. PMID: 1090839.3. Wicklund MP, Kissel JT. 2014; The limb-girdle muscular dystrophies. Neurol Clin. 32:729–49. DOI: 10.1016/j.ncl.2014.04.005. PMID: 25037088.
Article4. Nguyen K, Bassez G, Bernard R, Krahn M, Labelle V, Figarella-Branger D, et al. 2005; Dysferlin mutations in LGMD2B, Miyoshi myopathy, and atypical dysferlinopathies. Hum Mutat. 26:165. DOI: 10.1002/humu.9355. PMID: 16010686.
Article5. Choi JH, Park YE, Kim SI, Kim JI, Lee CH, Park KH, et al. 2009; Differential immunohistological features of inflammatory myopathies and dysferlinopathy. J Korean Med Sci. 24:1015–23. DOI: 10.3346/jkms.2009.24.6.1015. PMID: 19949654. PMCID: PMC2775846.
Article6. Park YE, Kim HS, Lee CH, Nam TS, Choi YC, Kim DS. 2012; Two common mutations (p.Gln832X and c.663+1G>C) account for about a third of the DYSF mutations in Korean patients with dysferlinopathy. Neuromuscul Disord. 22:505–10. DOI: 10.1016/j.nmd.2011.12.007. PMID: 22297152.7. Bansal D, Miyake K, Vogel SS, Groh S, Chen CC, Williamson R, et al. 2003; Defective membrane repair in dysferlin-deficient muscular dystrophy. Nature. 423:168–72. DOI: 10.1038/nature01573. PMID: 12736685.
Article8. Petersen JA, Kuntzer T, Fischer D, von der Hagen M, Huebner A, Kana V, et al. 2015; Dysferlinopathy in Switzerland: clinical phenotypes and potential founder effects. BMC Neurol. 15:182. DOI: 10.1186/s12883-015-0449-3. PMID: 26444858. PMCID: PMC4596355.
Article9. Tarnopolsky MA, Hatcher E, Shupak R. 2016; Genetic myopathies initially diagnosed and treated as inflammatory myopathy. Can J Neurol Sci. 43:381–4. DOI: 10.1017/cjn.2015.386. PMID: 26911292.
Article10. Klinge L, Aboumousa A, Eagle M, Hudson J, Sarkozy A, Vita G, et al. 2010; New aspects on patients affected by dysferlin deficient muscular dystrophy. J Neurol Neurosurg Psychiatry. 81:946–53. DOI: 10.1136/jnnp.2009.178038. PMID: 19528035. PMCID: PMC2975994.
Article11. Biondi O, Villemeur M, Marchand A, Chretien F, Bourg N, Gherardi RK, et al. 2013; Dual effects of exercise in dysferlinopathy. Am J Pathol. 182:2298–309. DOI: 10.1016/j.ajpath.2013.02.045. PMID: 23624156.
Article12. Fanin M, Angelini C. 2016; Progress and challenges in diagnosis of dysferlinopathy. Muscle Nerve. 54:821–35. DOI: 10.1002/mus.25367. PMID: 27501525.
Article13. Vinit J, Samson M Jr, Gaultier JB, Laquerriere A, Ollagnon E, Petiot P, et al. 2010; Dysferlin deficiency treated like refractory polymyositis. Clin Rheumatol. 29:103–6. DOI: 10.1007/s10067-009-1273-1. PMID: 19730931.
Article14. Mammen AL. 2016; Statin-associated autoimmune myopathy. N Engl J Med. 374:664–9. DOI: 10.1056/NEJMra1515161. PMID: 26886523.
Article15. Park HJ, Hong JM, Suh GI, Shin HY, Kim SM, Sunwoo IN, et al. 2012; Heterogeneous characteristics of Korean patients with dysferlinopathy. J Korean Med Sci. 27:423–9. DOI: 10.3346/jkms.2012.27.4.423. PMID: 22468107. PMCID: PMC3314856.
Article16. Takahashi T, Aoki M, Suzuki N, Tateyama M, Yaginuma C, Sato H, et al. 2013; Clinical features and a mutation with late onset of limb girdle muscular dystrophy 2B. J Neurol Neurosurg Psychiatry. 84:433–40. DOI: 10.1136/jnnp-2011-301339. PMID: 23243261. PMCID: PMC3595148.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early-Onset LMNA-Associated Muscular Dystrophy with Later Involvement of Contracture
- Limb-Girdle Muscular Dystrophy
- Clinical and Pathological Characteristics of Four Korean Patients with Limb-Girdle Muscular Dystrophy type 2B
- Progressive Muscular Dystrophy (Report of 32 cases)
- Heterogeneous Characteristics of Korean Patients with Dysferlinopathy