Blood Res.
2021 Mar;56(1):6-16. 10.5045/br.2021.2020083.
Updated recommendations for the treatment of venous thromboembolism
- Affiliations
-
- 1Division of Hematology-Medical Oncology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Department of Hematology-Oncology, Korea.
- 2Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 3Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 4Division of Hematology and Oncology, Department of Internal Medicine, Dong-A University College of Medicine, Dong-A University Hospital, Busan, Korea.
- 5Division of Pediatric Hematology and Oncology, Department of Pediatrics, Yonsei University College of Medicine, Yonsei University Health System, Jeonju, Korea.
- 6Department of Oncology and Hematology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Department of Internal Medicine, Jeonju, Korea.
- 7Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea.
- 8Veterans Health Service Medical Center, Seoul, Korea.
- 9Department of Laboratory Medicine & Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 10Department of Laboratory Medicine, Yonsei University College of Medicine, Severance Hospital, Seoul, Korea.
- 11Division of Hematology-Medical Oncology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 12Division of Hematology, Department of Internal Medicine, Yonsei University College of Medicine, Severance Hospital, Department of Internal Medicine, Seoul, Korea
- 13Ewha Womans University College of Medicine, Seoul, Korea.
- 14Daegu Catholic University School of Medicine, Daegu Catholic University Hospital, Daegu, Department of Laboratory Medicine, Korea.
- 15Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
- 16University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 17Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 18Department of Pediatrics, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 19Division of Hematology-Oncology, Department of Internal Medicine, CHA University School of Medicine, Seongnam, Korea.
- KMID: 2514059
- DOI: http://doi.org/10.5045/br.2021.2020083
Abstract
- Venous thromboembolism (VTE), which includes pulmonary embolism and deep vein thrombosis, is a condition characterized by abnormal blood clot formation in the pulmonary arteries and the deep venous vasculature. It is often serious and sometimes even fatal if not promptly and appropriately treated. Moreover, the later consequences of VTE may result in reduced quality of life. The treatment of VTE depends on various factors, including the type, cause, and patient comorbidities. Furthermore, bleeding may occur as a side effect of VTE treatment. Thus, it is necessary to carefully weigh the benefits versus the risks of VTE treatment and to actively monitor patients undergoing treatment. Asian populations are known to have lower VTE incidences than Western populations, but recent studies have shown an increase in the incidence of VTE in Asia. A variety of treatment options are currently available owing to the introduction of direct oral anticoagulants. The current VTE treatment recommendation is based on evidence from previous studies, but it should be applied with careful consideration of the racial, genetic, and social characteristics in the Korean population.
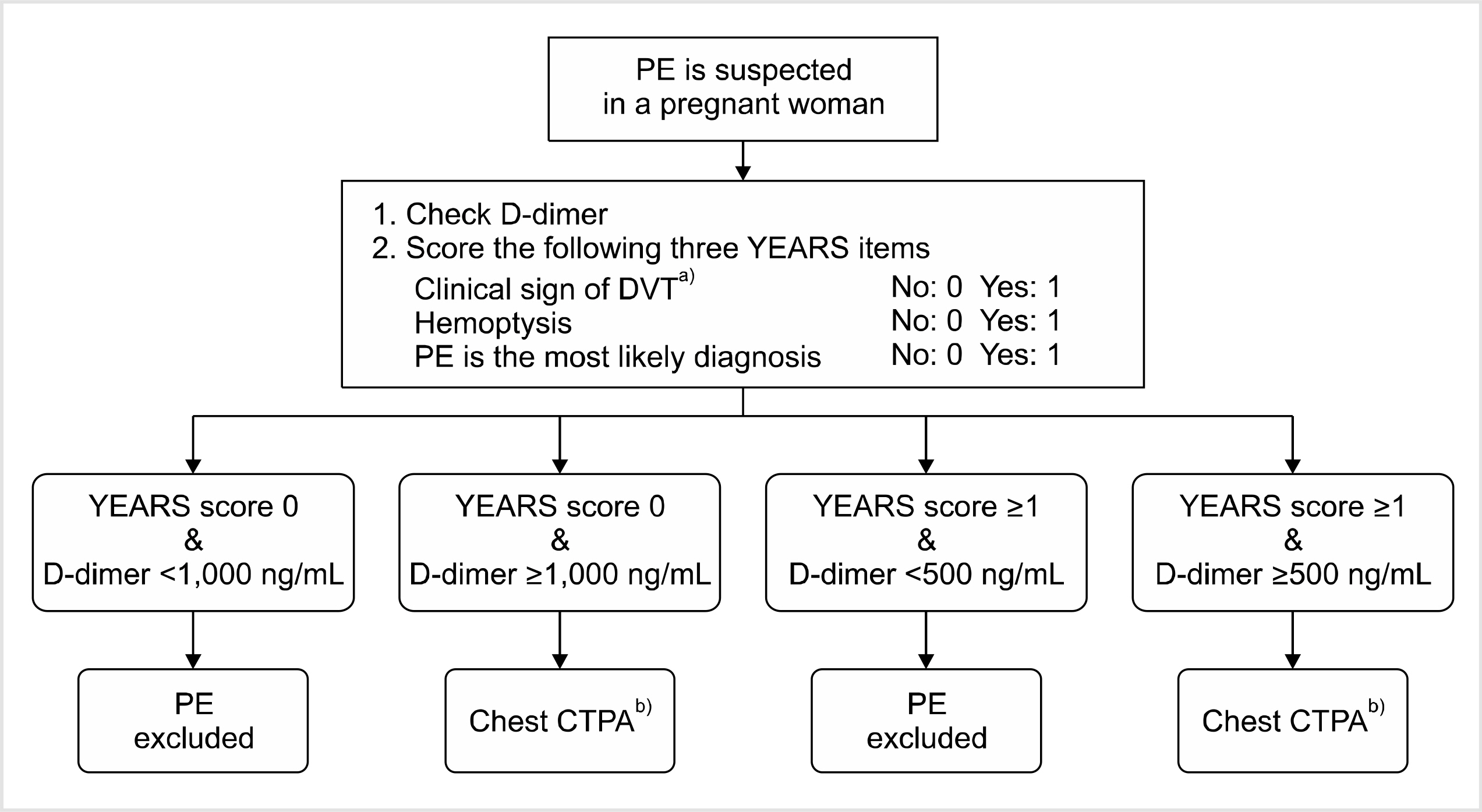
Figure
Reference
-
1. Lee CH, Lin LJ, Cheng CL, Kao Yang YH, Chen JY, Tsai LM. 2010; Incidence and cumulative recurrence rates of venous thrombo-embolism in the Taiwanese population. J Thromb Haemost. 8:1515–23. DOI: 10.1111/j.1538-7836.2010.03873.x. PMID: 20345707.2. Jang MJ, Bang SM, Oh D. 2011; Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 9:85–91. DOI: 10.1111/j.1538-7836.2010.04108.x. PMID: 20942850.3. Hong J, Lee JH, Yhim HY, et al. 2018; Incidence of venous thrombo-embolism in Korea from 2009 to 2013. PLoS One. 13:e0191897. DOI: 10.1371/journal.pone.0191897. PMID: 29370290. PMCID: PMC5785001.4. Goldhaber SZ, Bounameaux H. 2012; Pulmonary embolism and deep vein thrombosis. Lancet. 379:1835–46. DOI: 10.1016/S0140-6736(11)61904-1. PMID: 22494827.5. White RH. 2003; The epidemiology of venous thromboembolism. Circulation. 107(23 Suppl 1):I4–8. DOI: 10.1161/01.CIR.0000078468.11849.66. PMID: 12814979.6. Yhim HY, Choi WI, Kim SH, et al. 2019; Long-term rivaroxaban for the treatment of acute venous thromboembolism in patients with active cancer in a prospective multicenter trial. Korean J Intern Med. 34:1125–35. DOI: 10.3904/kjim.2018.097. PMID: 29788694. PMCID: PMC6718768.7. Boon GJAM, Van Dam LF, Klok FA, Huisman MV. 2018; Management and treatment of deep vein thrombosis in special populations. Expert Rev Hematol. 11:685–95. DOI: 10.1080/17474086.2018.1502082. PMID: 30016119.8. EINSTEIN-PE Investigators. 2012; Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 366:1287–97. DOI: 10.1056/NEJMoa1113572. PMID: 22449293.9. Agnelli G, Buller HR, Cohen A, et al. 2013; Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 369:799–808. DOI: 10.1056/NEJMoa1302507. PMID: 23808982.10. Hokusai-VTE Investigators. 2013; Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 369:1406–15. DOI: 10.1056/NEJMoa1306638. PMID: 23991658.11. Schulman S, Kearon C, Kakkar AK, et al. 2009; Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 361:2342–52. DOI: 10.1056/NEJMoa0906598. PMID: 19966341.12. Hakeam HA, Al-Sanea N. 2017; Effect of major gastrointestinal tract surgery on the absorption and efficacy of direct acting oral anticoagulants (DOACs). J Thromb Thrombolysis. 43:343–51. DOI: 10.1007/s11239-016-1465-x. PMID: 28050755.13. Raskob GE, van Es N, Verhamme P, et al. 2018; Edoxaban for the treatment of cancer-associated venous thromboembolism. N Engl J Med. 378:615–24. DOI: 10.1056/NEJMoa1711948. PMID: 29231094.14. Lee AY, Levine MN, Baker RI, et al. 2003; Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 349:146–53. DOI: 10.1056/NEJMoa025313. PMID: 12853587.15. Galanaud JP, Laroche JP, Righini M. 2013; The history and historical treatments of deep vein thrombosis. J Thromb Haemost. 11:402–11. DOI: 10.1111/jth.12127. PMID: 23297815.16. Kearon C, Akl EA, Ornelas J, et al. 2016; Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 149:315–52. DOI: 10.1016/j.chest.2015.11.026. PMID: 26867832.17. Horner D, Hogg K, Body R, Nash MJ, Baglin T, Mackway-Jones K. 2014; The anticoagulation of calf thrombosis (ACT) project: results from the randomized controlled external pilot trial. Chest. 146:1468–77. DOI: 10.1378/chest.14-0235. PMID: 25010443.18. Lagerstedt CI, Olsson CG, Fagher BO, Oqvist BW, Albrechtsson U. 1985; Need for long-term anticoagulant treatment in symptomatic calf-vein thrombosis. Lancet. 2:515–8. DOI: 10.1016/S0140-6736(85)90459-3. PMID: 2863541.19. Pinede L, Ninet J, Duhaut P, et al. 2001; Comparison of 3 and 6 months of oral anticoagulant therapy after a first episode of proximal deep vein thrombosis or pulmonary embolism and comparison of 6 and 12 weeks of therapy after isolated calf deep vein thrombosis. Circulation. 103:2453–60. DOI: 10.1161/01.CIR.103.20.2453. PMID: 11369685.20. Schwarz T, Buschmann L, Beyer J, Halbritter K, Rastan A, Schellong S. 2010; Therapy of isolated calf muscle vein thrombosis: a randomized, controlled study. J Vasc Surg. 52:1246–50. DOI: 10.1016/j.jvs.2010.05.094. PMID: 20630682.21. Franco L, Giustozzi M, Agnelli G, Becattini C. 2017; Anticoagulation in patients with isolated distal deep vein thrombosis: a meta-analysis. J Thromb Haemost. 15:1142–54. DOI: 10.1111/jth.13677. PMID: 28316124.22. Righini M, Galanaud JP, Guenneguez H, et al. 2016; Anticoagulant therapy for symptomatic calf deep vein thrombosis (CACTUS): a randomised, double-blind, placebo-controlled trial. Lancet Haematol. 3:e556–62. DOI: 10.1016/S2352-3026(16)30131-4. PMID: 27836513.23. Ho P, Lim HY, Chua CC, et al. 2016; Retrospective review on isolated distal deep vein thrombosis (IDDVT) - a benign entity or not? Thromb Res. 142:11–6. DOI: 10.1016/j.thromres.2016.04.003. PMID: 27093232.24. Chatterjee S, Chakraborty A, Weinberg I, et al. 2014; Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA. 311:2414–21. DOI: 10.1001/jama.2014.5990. PMID: 24938564.25. Schulman S, Kakkar AK, Goldhaber SZ, et al. 2014; Treatment of acute venous thromboembolism with dabigatran or warfarin and pooled analysis. Circulation. 129:764–72. DOI: 10.1161/CIRCULATIONAHA.113.004450. PMID: 24344086.26. Carrier M, Righini M, Le Gal G. 2012; Symptomatic subsegmental pulmonary embolism: what is the next step? J Thromb Haemost. 10:1486–90. DOI: 10.1111/j.1538-7836.2012.04804.x. PMID: 22672341.27. Goy J, Lee J, Levine O, Chaudhry S, Crowther M. 2015; Sub-segmental pulmonary embolism in three academic teaching hospitals: a review of management and outcomes. J Thromb Haemost. 13:214–8. DOI: 10.1111/jth.12803. PMID: 25442511.28. Raskob GE. 2013; Importance of subsegmental pulmonary embolism. Blood. 122:1094–5. DOI: 10.1182/blood-2013-06-508440. PMID: 23950170.29. den Exter PL, van Es J, Klok FA, et al. 2013; Risk profile and clinical outcome of symptomatic subsegmental acute pulmonary embolism. Blood. 122:1144–9. quiz 1329DOI: 10.1182/blood-2013-04-497545. PMID: 23736701.30. O'Connell C. 2015; Incidentally found pulmonary embolism: what's the clinician to do? Hematology Am Soc Hematol Educ Program. 2015:197–201. DOI: 10.1182/asheducation-2015.1.197. PMID: 26637721.31. Lee AYY, Kamphuisen PW, Meyer G, et al. 2015; Tinzaparin vs warfarin for treatment of acute venous thromboembolism in patients with active cancer: a randomized clinical trial. JAMA. 314:677–86. DOI: 10.1001/jama.2015.9243. PMID: 26284719.32. Vedovati MC, Germini F, Agnelli G, Becattini C. 2015; Direct oral anticoagulants in patients with VTE and cancer: a systematic review and meta-analysis. Chest. 147:475–83. DOI: 10.1378/chest.14-0402. PMID: 25211264.33. Young AM, Marshall A, Thirlwall J, et al. 2018; Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: results of a randomized trial (SELECT-D). J Clin Oncol. 36:2017–23. DOI: 10.1200/JCO.2018.78.8034. PMID: 29746227.34. Key NS, Khorana AA, Kuderer NM, et al. 2020; Venous thrombo-embolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 38:496–520. DOI: 10.1200/JCO.19.01461. PMID: 31381464.35. Kim SA, Yhim HY, Bang SM. 2019; Current management of cancer-associated venous thromboembolism: focus on direct oral anticoagulants. J Korean Med Sci. 34:e52. DOI: 10.3346/jkms.2019.34.e52. PMID: 30787683. PMCID: PMC6374546.36. Scott G, Mahdi AJ, Alikhan R. 2015; Superficial vein thrombosis: a current approach to management. Br J Haematol. 168:639–45. DOI: 10.1111/bjh.13255. PMID: 25521017.37. Di Nisio M, Wichers I, Middeldorp S. 2018; Treatment of lower extremity superficial thrombophlebitis. JAMA. 320:2367–8. DOI: 10.1001/jama.2018.16623. PMID: 30383173.38. Maddox RP, Seupaul RA. 2016; What is the most effective treatment of superficial thrombophlebitis? Ann Emerg Med. 67:671–2. DOI: 10.1016/j.annemergmed.2015.10.018. PMID: 26707361.39. Beyer-Westendorf J, Schellong SM, Gerlach H, et al. 2017; Prevention of thromboembolic complications in patients with superficial-vein thrombosis given rivaroxaban or fondaparinux: the open-label, randomised, non-inferiority SURPRISE phase 3b trial. Lancet Haematol. 4:e105–13. DOI: 10.1016/S2352-3026(17)30014-5. PMID: 28219692.40. Debourdeau P, Farge D, Beckers M, et al. 2013; International clinical practice guidelines for the treatment and prophylaxis of thrombosis associated with central venous catheters in patients with cancer. J Thromb Haemost. 11:71–80. DOI: 10.1111/jth.12071. PMID: 23217208.41. Barco S, Atema JJ, Coppens M, Serlie MJ, Middeldorp S. 2017; Anticoagulants for the prevention and treatment of catheter-related thrombosis in adults and children on parenteral nutrition: a systematic review and critical appraisal. Blood Transfus. 15:369–77. DOI: 10.2450/2016.0031-16. PMID: 27483479. PMCID: PMC5490734.42. Baumann Kreuziger L, Jaffray J, Carrier M. 2017; Epidemiology, diagnosis, prevention and treatment of catheter-related thrombosis in children and adults. Thromb Res. 157:64–71. DOI: 10.1016/j.thromres.2017.07.002. PMID: 28710972.43. Kahale LA, Tsolakian IG, Hakoum MB, et al. 2018; Anticoagulation for people with cancer and central venous catheters. Cochrane Database Syst Rev. 6:CD006468. DOI: 10.1002/14651858.CD006468.pub6. PMID: 29856471. PMCID: PMC6389340.44. Kahn SR, Lim W, Dunn AS, et al. 2012; Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 141(2 Suppl):e195S–e226S. DOI: 10.1378/chest.141.5.1369b. PMID: 22315261. PMCID: PMC3278052.45. De Stefano V, Martinelli I. 2010; Splanchnic vein thrombosis: clinical presentation, risk factors and treatment. Intern Emerg Med. 5:487–94. DOI: 10.1007/s11739-010-0413-6. PMID: 20532730.46. Riva N, Ageno W. 2017; Approach to thrombosis at unusual sites: splanchnic and cerebral vein thrombosis. Vasc Med. 22:529–40. DOI: 10.1177/1358863X17734057. PMID: 29202678.47. Smalberg JH, Arends LR, Valla DC, Kiladjian JJ, Janssen HL, Leebeek FW. 2012; Myeloproliferative neoplasms in Budd-Chiari syndrome and portal vein thrombosis: a meta-analysis. Blood. 120:4921–8. DOI: 10.1182/blood-2011-09-376517. PMID: 23043069.48. Kearon C, Akl EA, Comerota AJ, et al. 2012; Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 141(2 Suppl):e419S–e96S. DOI: 10.1378/chest.141.5.1369b. PMID: 22315268. PMCID: PMC3278049.49. DeLeve LD, Valla DC, Garcia-Tsao G. American Association for the Study Liver Diseases. 2009; Vascular disorders of the liver. Hepatology. 49:1729–64. DOI: 10.1002/hep.22772. PMID: 19399912. PMCID: PMC6697263.50. Ageno W, Riva N, Schulman S, et al. 2015; Long-term clinical outcomes of splanchnic vein thrombosis: results of an international registry. JAMA Intern Med. 175:1474–80. DOI: 10.1001/jamainternmed.2015.3184. PMID: 26168152.51. Ageno W, Beyer-Westendorf J, Garcia DA, Lazo-Langner A, McBane RD, Paciaroni M. 2016; Guidance for the management of venous thrombosis in unusual sites. J Thromb Thrombolysis. 41:129–43. DOI: 10.1007/s11239-015-1308-1. PMID: 26780742. PMCID: PMC4715841.52. Kourlaba G, Relakis J, Kontodimas S, Holm MV, Maniadakis N. 2016; A systematic review and meta-analysis of the epidemiology and burden of venous thromboembolism among pregnant women. Int J Gynaecol Obstet. 132:4–10. DOI: 10.1016/j.ijgo.2015.06.054. PMID: 26489486.53. Bates SM, Rajasekhar A, Middeldorp S, et al. 2018; American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2:3317–59. DOI: 10.1182/bloodadvances.2018024802. PMID: 30482767. PMCID: PMC6258928.54. van der Pol LM, Tromeur C, Bistervels IM, et al. 2019; Pregnancy-adapted YEARS algorithm for diagnosis of suspected pulmonary embolism. N Engl J Med. 380:1139–49. DOI: 10.1056/NEJMoa1813865. PMID: 30893534.55. Lameijer H, Aalberts JJJ, van Veldhuisen DJ, Meijer K, Pieper PG. 2018; Efficacy and safety of direct oral anticoagulants during pregnancy; a systematic literature review. Thromb Res. 169:123–7. DOI: 10.1016/j.thromres.2018.07.022. PMID: 30036784.56. Knol HM, Schultinge L, Veeger NJ, Kluin-Nelemans HC, Erwich JJ, Meijer K. 2012; The risk of postpartum hemorrhage in women using high dose of low-molecular-weight heparins during pregnancy. Thromb Res. 130:334–8. DOI: 10.1016/j.thromres.2012.03.007. PMID: 22475315.57. Klaassen IL, van Ommen CH, Middeldorp S. 2015; Manifestations and clinical impact of pediatric inherited thrombophilia. Blood. 125:1073–7. DOI: 10.1182/blood-2014-05-536060. PMID: 25564402.58. Nowak-Göttl U, von Kries R, Göbel U. 1997; Neonatal symptomatic thromboembolism in Germany: two year survey. Arch Dis Child Fetal Neonatal Ed. 76:F163–7. DOI: 10.1136/fn.76.3.F163. PMID: 9175945. PMCID: PMC1720641.59. van Ommen CH, Heijboer H, Büller HR, Hirasing RA, Heijmans HS, Peters M. 2001; Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr. 139:676–81. DOI: 10.1067/mpd.2001.118192. PMID: 11713446.60. Chalmers EA. 2006; Epidemiology of venous thromboembolism in neonates and children. Thromb Res. 118:3–12. DOI: 10.1016/j.thromres.2005.01.010. PMID: 16709473.61. Andrew M, David M, Adams M, et al. 1994; Venous thromboembolic complications (VTE) in children: first analyses of the Canadian Registry of VTE. Blood. 83:1251–7. DOI: 10.1182/blood.V83.5.1251.1251. PMID: 8118029.62. Miletich J, Sherman L, Broze G Jr. 1987; Absence of thrombosis in subjects with heterozygous protein C deficiency. N Engl J Med. 317:991–6. DOI: 10.1056/NEJM198710153171604. PMID: 3657866.63. Tait RC, Walker ID, Reitsma PH, et al. 1995; Prevalence of protein C deficiency in the healthy population. Thromb Haemost. 73:87–93. DOI: 10.1055/s-0038-1653730. PMID: 7740502.64. Mateo J, Oliver A, Borrell M, Sala N, Fontcuberta J. 1997; Laboratory evaluation and clinical characteristics of 2,132 consecutive unselected patients with venous thromboembolism--results of the Spanish Multicentric Study on Thrombophilia (EMET-Study). Thromb Haemost. 77:444–51. DOI: 10.1055/s-0038-1655986. PMID: 9065991.65. Heijboer H, Brandjes DP, Büller HR, Sturk A, ten Cate JW. 1990; Deficiencies of coagulation-inhibiting and fibrinolytic proteins in outpatients with deep-vein thrombosis. N Engl J Med. 323:1512–6. DOI: 10.1056/NEJM199011293232202. PMID: 2146503.66. Pintao MC, Ribeiro DD, Bezemer ID, et al. 2013; Protein S levels and the risk of venous thrombosis: results from the MEGA case-control study. Blood. 122:3210–9. DOI: 10.1182/blood-2013-04-499335. PMID: 24014240.67. Tait RC, Walker ID, Perry DJ, et al. 1994; Prevalence of antithrombin deficiency in the healthy population. Br J Haematol. 87:106–12. DOI: 10.1111/j.1365-2141.1994.tb04878.x. PMID: 7947234.68. Raffini L. 2008; Thrombophilia in children: who to test, how, when, and why? Hematology Am Soc Hematol Educ Program. 2008:228–35. DOI: 10.1182/asheducation-2008.1.228. PMID: 19074088.69. Andrew M, Paes B, Milner R, et al. 1987; Development of the human coagulation system in the full-term infant. Blood. 70:165–72. DOI: 10.1182/blood.V70.1.165.165. PMID: 3593964.70. Appel IM, Grimminck B, Geerts J, Stigter R, Cnossen MH, Beishuizen A. 2012; Age dependency of coagulation parameters during childhood and puberty. J Thromb Haemost. 10:2254–63. DOI: 10.1111/j.1538-7836.2012.04905.x. PMID: 22909016.71. Gavva C, Sarode R, Zia A. 2017; A clinical audit of thrombophilia testing in pediatric patients with acute thromboembolic events: impact on management. Blood Adv. 1:2386–91. DOI: 10.1182/bloodadvances.2017009514. PMID: 29296888. PMCID: PMC5729621.72. Young G. 2017; How I treat pediatric venous thromboembolism. Blood. 130:1402–8. DOI: 10.1182/blood-2017-04-742320. PMID: 28774877. PMCID: PMC5813720.73. Manco-Johnson MJ, Grabowski EF, Hellgreen M, et al. 2002; Laboratory testing for thrombophilia in pediatric patients. On behalf of the Subcommittee for Perinatal and Pediatric Thrombosis of the Scientific and Standardization Committee of the International Society of Thrombosis and Haemostasis (ISTH). Thromb Haemost. 88:155–6. DOI: 10.1055/s-0037-1613169. PMID: 12152657.74. Ageno W, Dentali F, Squizzato A, et al. 2010; Evidence and clinical judgment: treatment of cerebral vein thrombosis. Thromb Haemost. 103:1109–15. DOI: 10.1160/TH09-12-0827. PMID: 20390232.75. De Stefano V, Rossi E. 2013; Testing for inherited thrombophilia and consequences for antithrombotic prophylaxis in patients with venous thromboembolism and their relatives. A review of the Guidelines from Scientific Societies and Working Groups. Thromb Haemost. 110:697–705. DOI: 10.1160/TH13-01-0011. PMID: 23846575.76. Neshat-Vahid S, Pierce R, Hersey D, Raffini LJ, Faustino EV. 2016; Association of thrombophilia and catheter-associated thrombosis in children: a systematic review and meta-analysis. J Thromb Haemost. 14:1749–58. DOI: 10.1111/jth.13388. PMID: 27306795. PMCID: PMC5035642.77. Monagle P, Chan AKC, Goldenberg NA, et al. 2012; Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 141:e737S–e801S. DOI: 10.1378/chest.11-2308. PMID: 22315277. PMCID: PMC3278066.78. Monagle P, Cuello CA, Augustine C, et al. 2018; American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thrombo-embolism. Blood Adv. 2:3292–316. DOI: 10.1182/bloodadvances.2018024786. PMID: 30482766. PMCID: PMC6258911.79. Raffini LJ, Scott JP. 2016; Thrombotic disorders in children. In: Kliegman RM, Stanton BF, St Geme JW, Schor N, eds. Nelson textbook of pediatrics. 20th ed. Philadelphia, PA:. Elsevier,. 2394–7.80. Male C, Thom K, O'Brien SH. 2019; Direct oral anticoagulants: what will be their role in children? Thromb Res. 173:178–85. DOI: 10.1016/j.thromres.2018.06.021. PMID: 30017225.81. Thomas S, Makris M. 2018; The reversal of anticoagulation in clinical practice. Clin Med (Lond). 18:314–9. DOI: 10.7861/clinmedicine.18-4-314. PMID: 30072557. PMCID: PMC6334060.82. Keeling D, Baglin T, Tait C, et al. 2011; Guidelines on oral anticoagulation with warfarin - fourth edition. Br J Haematol. 154:311–24. DOI: 10.1111/j.1365-2141.2011.08753.x. PMID: 21671894.83. Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI. 2008; Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 133(6 Suppl):141S–59S. DOI: 10.1378/chest.08-0689. PMID: 18574264.84. Pollack CV Jr, Reilly PA, van Ryn J, et al. 2017; Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 377:431–41. DOI: 10.1056/NEJMoa1707278. PMID: 28693366.85. Connolly SJ, Crowther M, Eikelboom JW, et al. 2019; Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 380:1326–35. DOI: 10.1056/NEJMoa1814051. PMID: 30730782. PMCID: PMC6699827.86. Ansell JE, Bakhru SH, Laulicht BE, et al. 2017; Single-dose ciraparantag safely and completely reverses anticoagulant effects of edoxaban. Thromb Haemost. 117:238–45. DOI: 10.1160/TH16-03-0224. PMID: 27853809. PMCID: PMC6260118.87. Connors JM. 2018; Testing and monitoring direct oral anticoagulants. Blood. 132:2009–15. DOI: 10.1182/blood-2018-04-791541. PMID: 30201757.88. van Ryn J, Stangier J, Haertter S, et al. 2010; Dabigatran etexilate--a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost. 103:1116–27. DOI: 10.1160/TH09-11-0758. PMID: 20352166.89. Hawes EM, Deal AM, Funk-Adcock D, et al. 2013; Performance of coagulation tests in patients on therapeutic doses of dabigatran: a cross-sectional pharmacodynamic study based on peak and trough plasma levels. J Thromb Haemost. 11:1493–502. DOI: 10.1111/jth.12308. PMID: 23718677.90. Hillarp A, Baghaei F, Fagerberg Blixter I, et al. 2011; Effects of the oral, direct factor Xa inhibitor rivaroxaban on commonly used coagulation assays. J Thromb Haemost. 9:133–9. DOI: 10.1111/j.1538-7836.2010.04098.x. PMID: 20946166.91. Seiffge DJ, Traenka C, Polymeris AA, et al. 2017; Intravenous thrombolysis in patients with stroke taking rivaroxaban using drug specific plasma levels: experience with a standard operation procedure in clinical practice. J Stroke. 19:347–55. DOI: 10.5853/jos.2017.00395. PMID: 28877563. PMCID: PMC5647628.92. Schmitz EM, Boonen K, van den Heuvel DJ, et al. 2014; Determination of dabigatran, rivaroxaban and apixaban by ultra-performance liquid chromatography - tandem mass spectrometry (UPLC-MS/MS) and coagulation assays for therapy monitoring of novel direct oral anticoagulants. J Thromb Haemost. 12:1636–46. DOI: 10.1111/jth.12702. PMID: 25142183.93. Forbes HL, Polasek TM. 2017; Potential drug-drug interactions with direct oral anticoagulants in elderly hospitalized patients. Ther Adv Drug Saf. 8:319–28. DOI: 10.1177/2042098617719815. PMID: 29593860. PMCID: PMC5865464.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Year in Review of Venous Thromboembolism
- Updates of Evidence-Based Nursing Practice Guideline for Prevention of Venous Thromboembolism
- Challenging issues in the management of cancer-associated venous thromboembolism
- Anticoagulation Treatment Using NOAC in Patients with Venous Thromboembolism
- Venous thromboembolism in children and adolescents