Obstet Gynecol Sci.
2021 Mar;64(2):174-189. 10.5468/ogs.20174.
A systematic review of clinical and laboratory parameters of 3,000 COVID-19 cases
- Affiliations
-
- 1Laboratory Oncology Unit, Dr.B.R.A.-Institute Rotary Cancer Hospital, New Delhi, India
- 2All India Institute of Medical Sciences, New Delhi, India
- 3Department of Anaesthesia and Intensive Care, Vardhaman Mahavir Medical College & Safdarjung Hospital, New Delhi, India
- 4UPMC Hillman Cancer Center, Erie, PA, USA
- 5Department of Radiotherapy, Dr. B.R.A.- Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India
- KMID: 2513947
- DOI: http://doi.org/10.5468/ogs.20174
Abstract
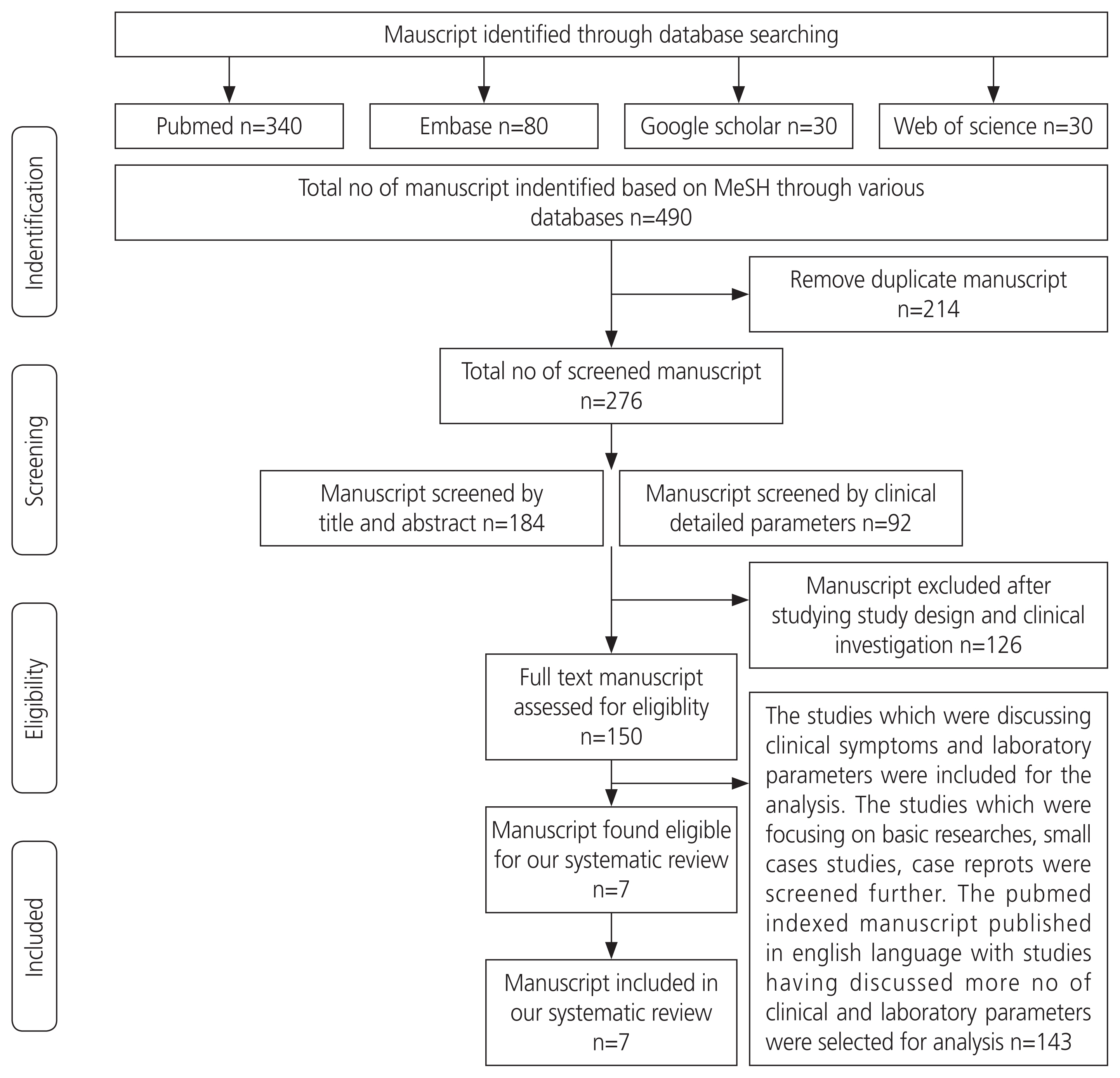
- The coronavirus disease 2019 (COVID-19) has spread worldwide. It is still a pandemic and poses major health problem across the globe. In our review, clinical characteristics and laboratory parameters of COVID-19 patients were compiled systematically, with special reference to pregnant women in order to understand the disease course. An extensive literature search on various scientific databases for relevant manuscripts was conducted, which yielded 7 manuscripts for final analysis. The most common symptoms were fever (85%), cough (70.63%), chest tightness (37.36%), expectoration (33.27%), fatigue (32%), dyspnea (31.95%), and shortness of breath (31.19%), while hemoptysis (1.0%) was the least common. The associated comorbidities were hypertension (21.6%) and diabetes (10.0%). In terms of hematological parameters, lower total leukocyte counts were observed in 65% of cases and biochemical parameters, patients demonstrated elevated levels of albumin (53.72%), lactate dehydrogenase (45.71%), and natriuretic peptide (34.84%); however, total bilirubin was elevated in only 8% of cases. In the acute inflammatory cytokine profile, C-reactive protein (59.0%), tumor necrosis factor (58.0%), erythrocyte sedimentation rate (57.0%), interleukin-2 (IL- 2, 54.0%), and IL-6 (52.0%) levels were increased, while prolactin levels (6.5%) were minimally elevated. The recovery rate was approximately 41%, and mortality was about 6.5%. The study also concluded that the clinical symptoms of COVID-19 were similar among pregnant and non-pregnant women. There was no evidence of vertical transmission of COVID-19 infection. This review critically analyzed COVID-19 as a public health hazard in order to help policy makers, health care givers, and primary physicians to promote early diagnosis and prevention.
Keyword
Figure
Cited by 1 articles
-
The complement system in preeclampsia: a review of its activation and endothelial injury in the triad of COVID-19 infection and HIV-associated preeclampsia
Mikyle David, Thajasvarie Naicker
Obstet Gynecol Sci. 2023;66(4):253-269. doi: 10.5468/ogs.22175.
Reference
-
References
1. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020; 395:565–74.2. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020; 579:270–3.
Article3. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506.
Article4. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–20.
Article5. Wu Y, Ho W, Huang Y, Jin DY, Li S, Liu SL, et al. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020; 395:949–50.
Article6. World Health Organization. WHO director-general’s statement on IHR emergency committee on novel Coronavirus (2019-nCoV) [Internet]. Geneva: World Health Organization;c2020. [cited 2020 Jan 30]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov).7. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020; 5:536–44.8. Ramadan N, Shaib H. Middle East respiratory syndrome coronavirus (MERS-CoV): a review. Germs. 2019; 9:35–42.
Article9. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727–33.
Article10. Lei H, Li Y, Xiao S, Lin CH, Norris SL, Wei D, et al. Routes of transmission of influenza A H1N1, SARS CoV, and norovirus in air cabin: comparative analyses. Indoor Air. 2018; 28:394–403.
Article11. Otter JA, Donskey C, Yezli S, Douthwaite S, Goldenberg SD, Weber DJ. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect. 2016; 92:235–50.
Article12. Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. 2015; 386:995–1007.
Article13. Minodier L, Charrel RN, Ceccaldi PE, van der Werf S, Blanchon T, Hanslik T, et al. Prevalence of gastrointestinal symptoms in patients with influenza, clinical significance, and pathophysiology of human influenza viruses in faecal samples: what do we know? Virol J. 2015; 12:215.
Article14. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel Coronavirus-infected pneumonia. N Engl J Med. 2020; 382:1199–207.
Article15. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395:507–13.
Article16. Kim KH, Tandi TE, Choi JW, Moon JM, Kim MS. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in South Korea, 2015: epidemiology, characteristics and public health implications. J Hosp Infect. 2017; 95:207–13.
Article17. World Health Organization. WHO COVID-19: case definitions updated in public health surveillance for COVID-19 [Internet]. Geneva: World Health Organization;c2020. [cited 2020 Jan 30]. Available from: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Surveillance_Case_Definition-2020.1 .18. Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020; 201:1380–8.
Article19. Yu X, Sun X, Cui P, Pan H, Lin S, Han R, et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai, China. Transbound Emerg Dis. 2020; 67:1697–707.
Article20. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020; 368:m1091.
Article21. Chen T, Dai Z, Mo P, Li X, Ma Z, Song S, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: a single-centered, retrospective study. Gerontol A Biol Sci Med Sci. 2020; 75:1788–95.
Article22. Cai Q, Huang D, Ou P, Yu H, Zhu Z, Xia Z, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020; 75:1742–52.
Article23. Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020; 146:110–8.
Article24. Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet Gynecol. 2020; 56:15–27.
Article25. Galang RR, Chang K, Strid P, Snead MC, Woodworth KR, House LD, et al. Severe Coronavirus infections in pregnancy: a systematic review. Obstet Gynecol. 2020; 136:262–72.26. Yoon SH, Kang JM, Ahn JG. Clinical outcomes of 201 neonates born to mothers with COVID-19: a systematic review. Eur Rev Med Pharmacol Sci. 2020; 24:7804–15.27. Trippella G, Ciarcià M, Ferrari M, Buzzatti C, Maccora I, Azzari C, et al. COVID-19 in pregnant women and neonates: a systematic review of the literature with quality assessment of the studies. Pathogens. 2020; 9:485.
Article28. Smith V, Seo D, Warty R, Payne O, Salih M, Chin KL, et al. Maternal and neonatal outcomes associated with COVID-19 infection: a systematic review. PLoS One. 2020; 15:e0234187.
Article29. World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003 [Internet]. Geneva: World Health Organization;c2020. [cited 2020 Feb 10]. Available from: https://www.who.int/csr/sars/country/table2004_04_21/en/ .30. World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV) [Internet]. Geneva: World Health Organization;c2020. [cited 2020 Feb 10]. Available from: http://www.who.int/emergencies/merscov/en/ .31. Taiwan center for disease control. Weekly number of suspected COVID-19 cases. [Internet]. Taipei city: Taiwan center for disease control;c2020. [cited 2020 Sep 13]. Available from: https://www.cdc.gov.tw/En .32. Sanchez-Ramirez DC, Mackey D. Underlying respiratory diseases, specifically COPD, and smoking are associated with severe COVID-19 outcomes: a systematic review and meta-analysis. Respir Med. 2020; 171:106096.
Article33. Zhan T, Liu M, Tang Y, Han Z, Cheng X, Deng J, et al. Retrospective analysis of clinical characteristics of 405 patients with COVID-19. J Int Med Res. 2020. Aug. 31. [Epub]. https://doi.org/10.1177/0300060520949039 .
Article34. Xiao M, Hou M, Liu X, Li Z, Zhao Q. Clinical characteristics of 71 patients with coronavirus disease 2019. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2020; 45:790–6.35. Ssentongo P, Ssentongo AE, Heilbrunn ES, Ba DM, Chinchilli VM. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: a systematic review and meta-analysis. PLoS One. 2020; 15:e0238215.
Article36. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180:934–43.
Article37. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395:1054–62.38. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020; 8:475–81.
Article39. Biguenet A, Bouiller K, Marty-Quinternet S, Brunel AS, Chirouze C, Lepiller Q. SARS-CoV-2 respiratory viral loads and association with clinical and biological features. J Med Virol. 2020. Sep. 5. [Epub]. https://doi.org/10.1002/jmv.26489 .
Article40. Min CK, Cheon S, Ha NY, Sohn KM, Kim Y, Aigerim A, et al. Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Sci Rep. 2016; 6:25359.
Article41. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017; 39:529–39.
Article42. Lu J, Zhang Y, Cheng G, He J, Wu F, Hu H, et al. Clinical characteristics and outcomes of adult critically ill patients with COVID-19 in Honghu, Hubei Province. Nan Fang Yi Ke Da Xue Xue Bao. 2020; 40:778–85.43. Patel U, Malik P, Usman MS, Mehta D, Sharma A, Malik FA, et al. Age-adjusted risk factors associated with mortality and mechanical ventilation utilization amongst COVID-19 hospitalizations-a systematic review and meta-analysis. SN Compr Clin Med. 2020. Aug. 29. [Epub]. https://doi.org/10.1007/s42399-020-00476-w .
Article44. Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health. 2020; 13:667–73.
Article45. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395:809–15.
Article46. Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020; 370:m3320.
Article47. Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020; 25:39.
Article48. Panahi L, Amiri M, Pouy S. Risks of novel coronavirus disease (COVID-19) in pregnancy; a narrative review. Arch Acad Emerg Med. 2020; 8:e34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current laboratory diagnosis of coronavirus disease 2019
- Clinical and Laboratory Features of Pediatric Patients with COVID-19: Systematic Review and Meta-analysis
- COVID-19 Patients: A Systematic Review and Meta-Analysis of Laboratory Findings, Comorbidities, and Clinical Outcomes Comparing Medical Staff versus the General Population
- Efficacy and Safety of COVID-19 Vaccines in Children Aged 5 to 11 Years: A Systematic Review
- Systematic Review for Remdesivir Use in Pediatric Patients under 3.5 kg with COVID-19