J Korean Assoc Oral Maxillofac Surg.
2021 Feb;47(1):34-39. 10.5125/jkaoms.2021.47.1.34.
Cone-beam computed tomography characterization of the intraosseous vascular canal in the lateral wall of the maxillary antrum
- Affiliations
-
- 1Oral Radiology, Department of Oral and Craniofacial Health Sciences, College of Dental Medicine, University of Sharjah, Sharjah, United Arab Emirates
- 2Oral and Maxillofacial Surgery, College of Dentistry, Gulf Medical University, Ajman, United Arab Emirates
- 3Department of Clinical Sciences, College of Dentistry, Ajman University, Ajman, United Arab Emirates
- 4Periodontics, College of Dentistry, Gulf Medical University, Ajman, United Arab Emirates
- KMID: 2513427
- DOI: http://doi.org/10.5125/jkaoms.2021.47.1.34
Abstract
Objectives
The purpose of the study was to assess the occurrence, location, and dimensions of the intraosseous vascular canal in the lateral wall of the maxillary antrum using cone-beam computed tomography (CBCT).
Materials and Methods
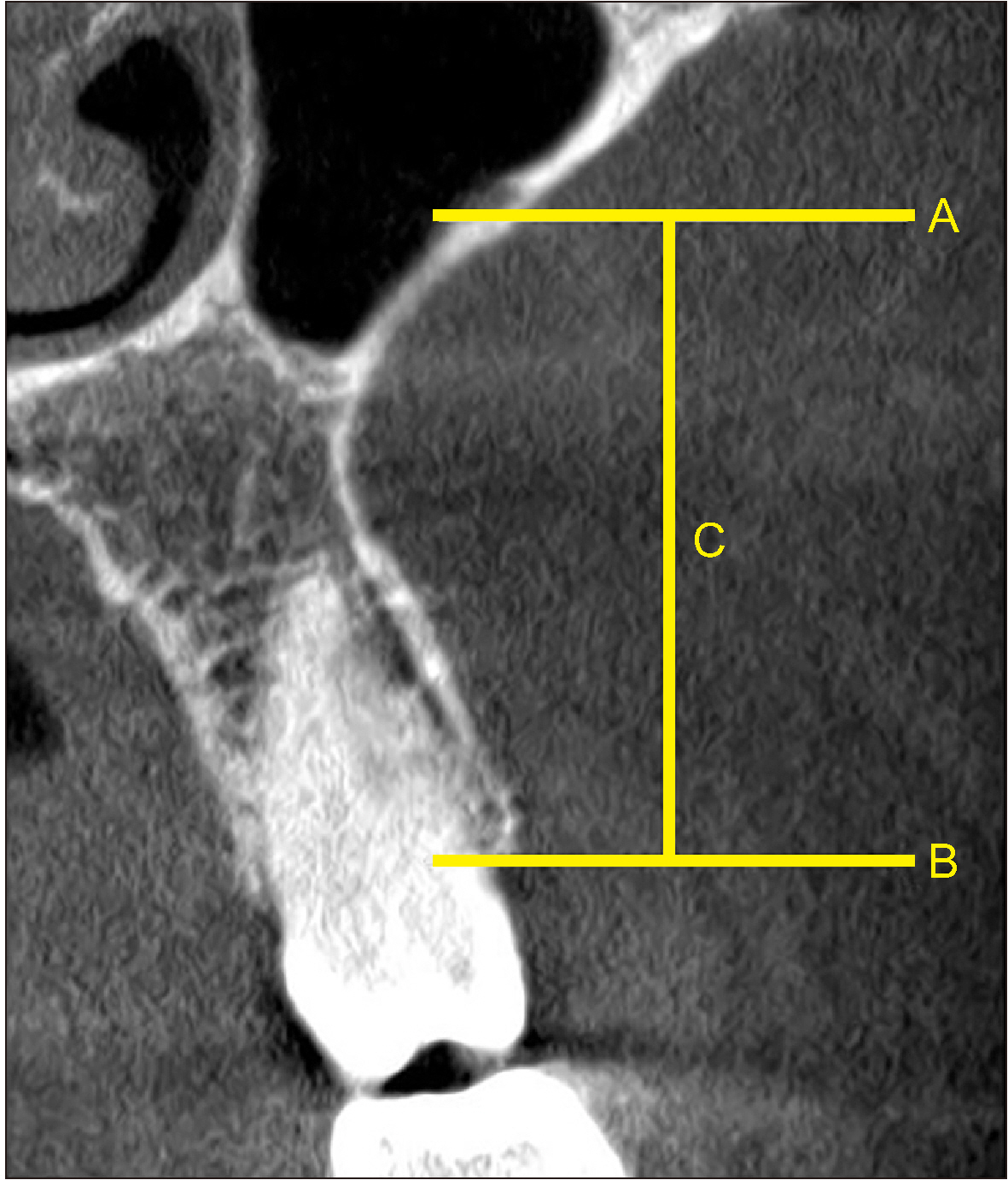
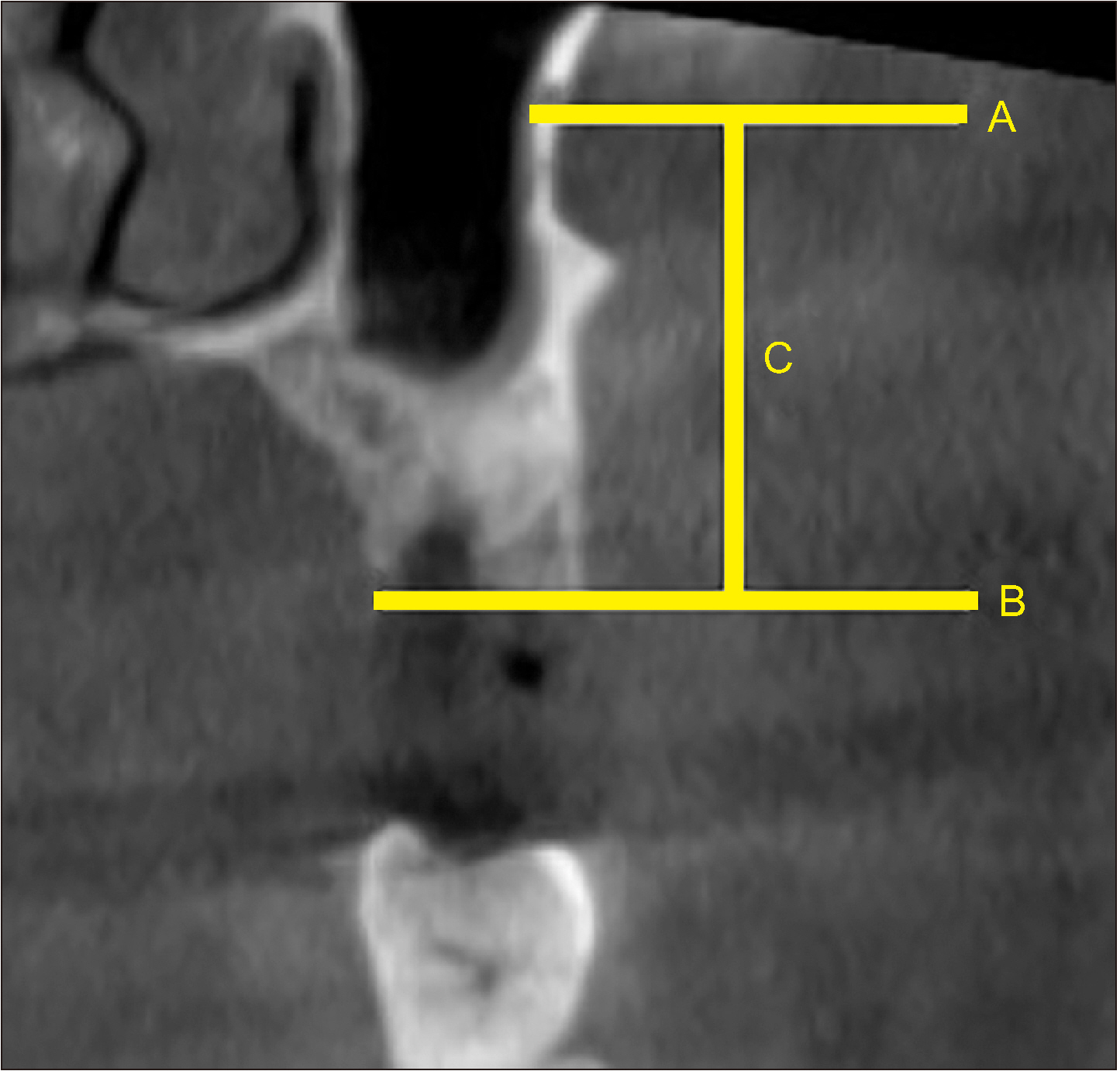
In this retrospective study, we examined 400 CBCT scans from our archive of patients who had earlier reported to a dental teaching hospital in the United Arab Emirates. The prevalence, location, and dimensions of the lateral antral intraosseous canal (LAIC) in the maxillary antrum were evaluated by 2 examiners using standardised methods. A third examiner was consulted in cases of disagreement.
Results
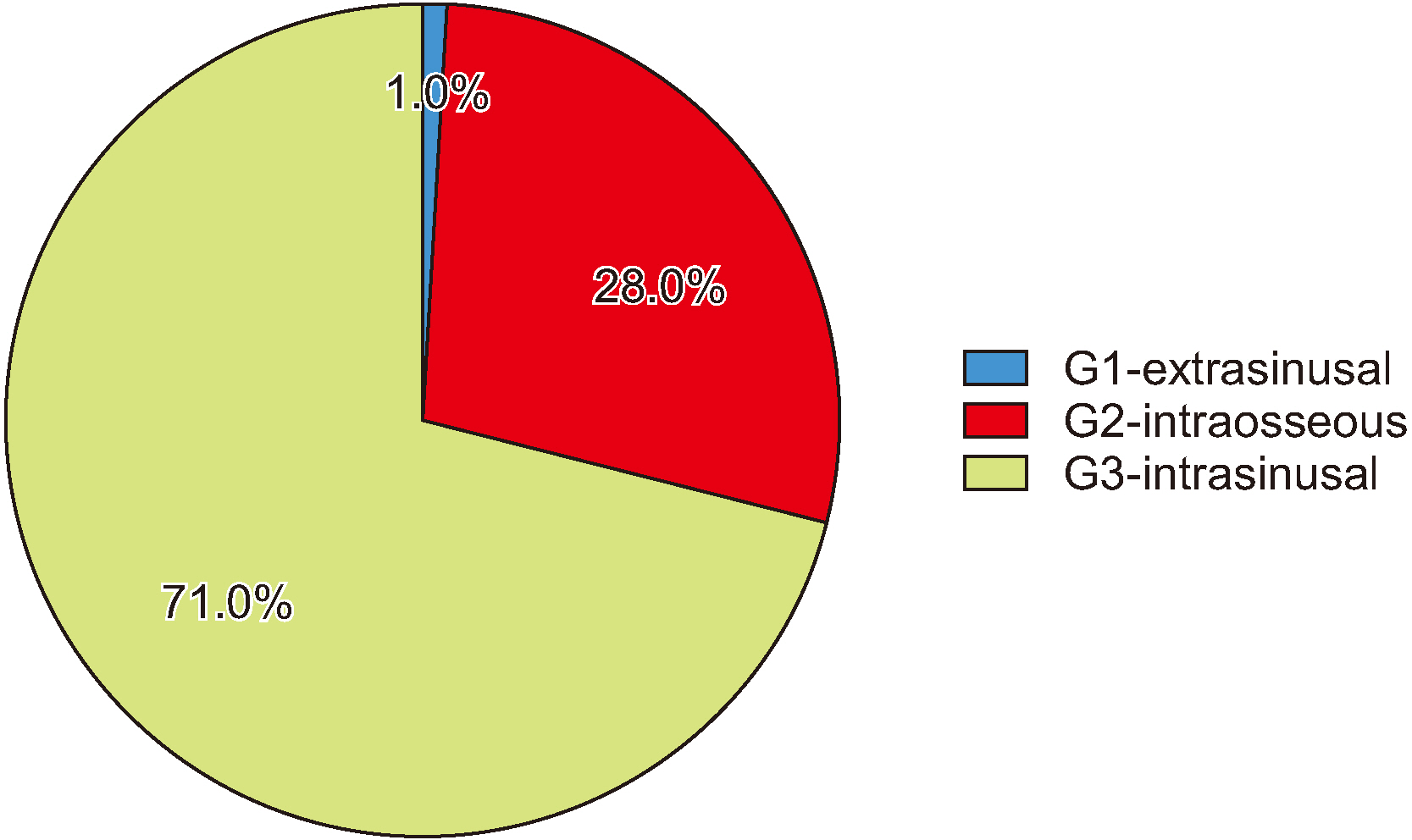
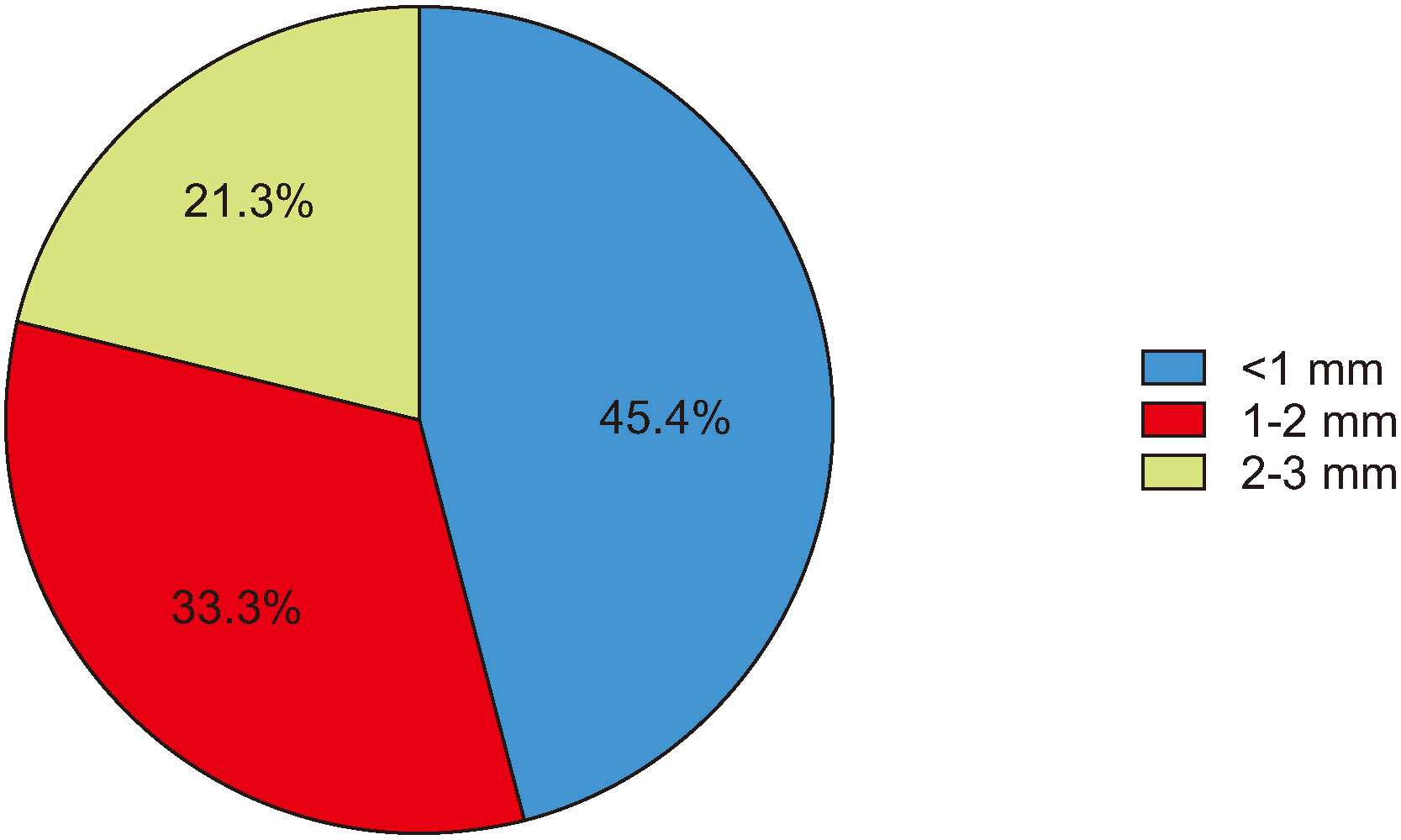
The prevalence of LAIC was 62.3% (249 maxillary antra) among the study population. The mean distance between the most inferior point of the alveolar bone and the inferior border of the LAIC in the posterior maxillary region was 19.83±3.12 mm. There was a significant difference (P=0.05) between the maxillary molar and premolar regions in mean distance from the most inferior point of the alveolar bone and the inferior border of the LAIC. There was no statistically significant difference in mean distance between the most inferior point of the alveolar bone and the inferior border of the LAIC between dentulous and edentulous areas (P=0.1). The G3-intrasinusal type canal less than 1mm in diameter was the most common type of LAIC.
Conclusion
This study established the approximate location of the LAIC in a United Arab Emirates cohort, which will assist the oral surgeon in selecting the appropriate site for sinus lift procedures with reduced risk of surgical hemorrhage.
Keyword
Figure
Reference
-
References
1. Albugami RA, Smith S, Hassan MA, Almas K. 2019; Trends in implant dentistry: implant systems, complications and barriers in Riyadh, Saudi Arabia. Dent Med Probl. 56:223–30. https://doi.org/10.17219/dmp/108659 . DOI: 10.17219/dmp/108659. PMID: 31577066.
Article2. Akeel R. 2003; Attitudes of Saudi male patients toward the replacement of teeth. J Prosthet Dent. 90:571–7. https://doi.org/10.1016/j.prosdent.2003.09.007 . DOI: 10.1016/j.prosdent.2003.09.007. PMID: 14668758.
Article3. Zijderveld SA, van den Bergh JP, Schulten EA, ten Bruggenkate CM. 2008; Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J Oral Maxillofac Surg. 66:1426–38. https://doi.org/10.1016/j.joms.2008.01.027 . DOI: 10.1016/j.joms.2008.01.027. PMID: 18571027.
Article4. Mung San Aung C, Panmekiat S, Pimkhaokham A. 2017; The study of the alveolar antral artery canal in using cone beam computed tomography. Mahidol Dent J. 37:63–9.5. Elian N, Wallace S, Cho SC, Jalbout ZN, Froum S. 2005; Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 20:784–7. PMID: 16274154.6. Varela-Centelles P, Loira M, González-Mosquera A, Romero-Mendez A, Seoane J, García-Pola MJ, et al. 2020; Study of factors influencing preoperative detection of alveolar antral artery by CBCT in sinus floor elevation. Sci Rep. 10:10820. https://doi.org/10.1038/s41598-020-67644-9 . DOI: 10.1038/s41598-020-67644-9. PMID: 32616752. PMCID: PMC7331631.
Article7. Rahpeyma A, Khajehahmadi S, Amini P. 2014; Alveolar antral artery: does its diameter correlate with maxillary lateral wall thickness in dentate patients? Iran J Otorhinolaryngol. 26:163–7. PMID: 25009806. PMCID: PMC4087855.8. Park WH, Choi SY, Kim CS. 2012; Study on the position of the posterior superior alveolar artery in relation to the performance of the maxillary sinus bone graft procedure in a Korean population. J Korean Assoc Oral Maxillofac Surg. 38:71–7. https://doi.org/10.5125/jkaoms.2012.38.2.71 .
Article9. Kim JH, Ryu JS, Kim KD, Hwang SH, Moon HS. 2011; A radiographic study of the posterior superior alveolar artery. Implant Dent. 20:306–10. https://doi.org/10.1097/ID.0b013e31822634bd . DOI: 10.1097/ID.0b013e31822634bd. PMID: 21778887.
Article10. Güncü GN, Yildirim YD, Wang HL, Tözüm TF. 2011; Location of posterior superior alveolar artery and evaluation of maxillary sinus anatomy with computerized tomography: a clinical study. Clin Oral Implants Res. 22:1164–7. https://doi.org/10.1111/j.1600-0501.2010.02071.x . DOI: 10.1111/j.1600-0501.2010.02071.x. PMID: 21244499.
Article11. Ilgüy D, Ilgüy M, Dolekoglu S, Fisekcioglu E. 2013; Evaluation of the posterior superior alveolar artery and the maxillary sinus with CBCT. Braz Oral Res. 27:431–7. https://doi.org/10.1590/S1806-83242013000500007 . DOI: 10.1590/S1806-83242013000500007. PMID: 24036981.
Article12. Mardinger O, Abba M, Hirshberg A, Schwartz-Arad D. 2007; Prevalence, diameter and course of the maxillary intraosseous vascular canal with relation to sinus augmentation procedure: a radiographic study. Int J Oral Maxillofac Surg. 36:735–8. https://doi.org/10.1016/j.ijom.2007.05.005 . DOI: 10.1016/j.ijom.2007.05.005. PMID: 17629462.
Article13. Lee J, Kang N, Moon YM, Pang EK. 2016; Radiographic study of the distribution of maxillary intraosseous vascular canal in Koreans. Maxillofac Plast Reconstr Surg. 38:1. https://doi.org/10.1186/s40902-015-0045-x . DOI: 10.1186/s40902-015-0045-x. PMID: 26767186. PMCID: PMC4700055.
Article14. Sun W, Liu A, Gong Y, Shu R, Xie Y. 2018; Evaluation of the anastomosis canal in lateral maxillary sinus wall with cone beam computerized tomography: a clinical study. J Oral Implantol. 44:5–13. https://doi.org/10.1563/aaid-joi-D-17-00129 . DOI: 10.1563/aaid-joi-D-17-00129. PMID: 29064762.
Article15. Cruz ILA, Palacios VDE, Miranda VJE, Cazar AM, Martínez OPA. 2016; [CBCT evaluation of the alveolar antral artery in a Mexican cohort and its relationship to maxillary sinus floor lifting]. Rev ADM. 73:286–90. Spanish.16. Lechuga L, Weidlich GA. 2016; Cone beam CT vs. fan beam CT: a comparison of image quality and dose delivered between two differing CT imaging modalities. Cureus. 8:e778. https://doi.org/10.7759/cureus.778 . DOI: 10.7759/cureus.778. PMID: 27752404. PMCID: PMC5063198.
Article17. Watanabe H, Honda E, Tetsumura A, Kurabayashi T. 2011; A comparative study for spatial resolution and subjective image characteristics of a multi-slice CT and a cone-beam CT for dental use. Eur J Radiol. 77:397–402. https://doi.org/10.1016/j.ejrad.2009.09.023 . DOI: 10.1016/j.ejrad.2009.09.023. PMID: 19819091.
Article18. Hur MS, Kim JK, Hu KS, Bae HE, Park HS, Kim HJ. 2009; Clinical implications of the topography and distribution of the posterior superior alveolar artery. J Craniofac Surg. 20:551–4. https://doi.org/10.1097/SCS.0b013e31819ba1c1 . DOI: 10.1097/SCS.0b013e31819ba1c1. PMID: 19305253.
Article19. Yoshida S, Kawai T, Asaumi R, Miwa Y, Imura K, Koseki H, et al. 2010; Evaluation of the blood and nerve supply patterns in the molar region of the maxillary sinus in Japanese cadavers. Okajimas Folia Anat Jpn. 87:129–33. https://doi.org/10.2535/ofaj.87.129 . DOI: 10.2535/ofaj.87.129. PMID: 21174942.
Article20. Kim J, Jang H. 2019; A review of complications of maxillary sinus augmentation and available treatment methods. J Korean Assoc Oral Maxillofac Surg. 45:220–4. https://doi.org/10.5125/jkaoms.2019.45.4.220 . DOI: 10.5125/jkaoms.2019.45.4.220. PMID: 31508355. PMCID: PMC6728618.
Article21. Kim YK, Ku JK. 2020; Sinus membrane elevation and implant placement. J Korean Assoc Oral Maxillofac Surg. 46:292–8. https://doi.org/10.5125/jkaoms.2020.46.4.292 . DOI: 10.5125/jkaoms.2020.46.4.292. PMID: 32855378. PMCID: PMC7469962.
Article22. Maridati P, Stoffella E, Speroni S, Cicciu M, Maiorana C. 2014; Alveolar antral artery isolation during sinus lift procedure with the double window technique. Open Dent J. 8:95–103. https://doi.org/10.2174/1874210601408010095 . DOI: 10.2174/1874210601408010095. PMID: 24949106. PMCID: PMC4062959.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the posterior superior alveolar artery canal by cone-beam computed tomography in a sample of the Egyptian population
- Detection of maxillary second molar with two palatal roots using cone beam computed tomography: a case report
- Distribution of Vascular Canal at Lateral Wall of Maxillary Sinus in Korean Population Using Computed Tomography
- Endodontic treatment of maxillary lateral incisors with anatomical variations
- Assessment of the relationship between the mandibular third molar and the mandibular canal using panoramic radiograph and cone beam computed tomography