Ann Rehabil Med.
2021 Feb;45(1):24-32. 10.5535/arm.20158.
Comparison of the Effectiveness of Three Lumbosacral Orthoses on Early Spine Surgery Patients: A Prospective Cohort Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Veterans Health Service Medical Center, Seoul, Korea
- 2Department of Orthopedic Surgery, Veterans Health Service Medical Center, Seoul, Korea
- 3Department of Neurosurgery, Veterans Health Service Medical Center, Seoul, Korea
- 4Veterans Medical Research Institute, Veterans Health Service Medical Center, Seoul, Korea
- 5Center of Prosthetics and Orthotics, Veterans Health Service Medical Center, Seoul, Korea
- KMID: 2513227
- DOI: http://doi.org/10.5535/arm.20158
Abstract
Objective
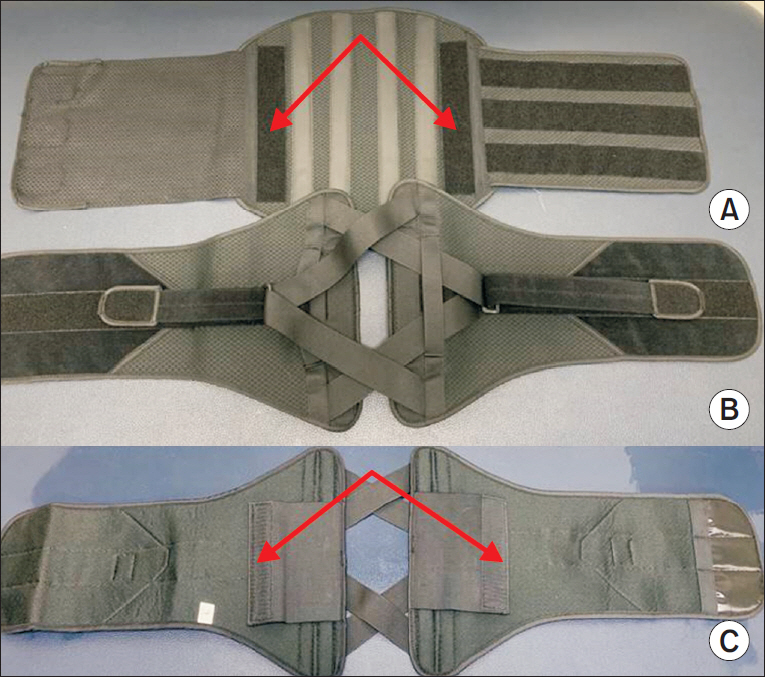
To compare the convenience and effectiveness of the existing lumbosacral orthoses (LSO) (classic LSO and Cybertech) and a newly developed LSO (V-LSO) by analyzing postoperative data.
Methods
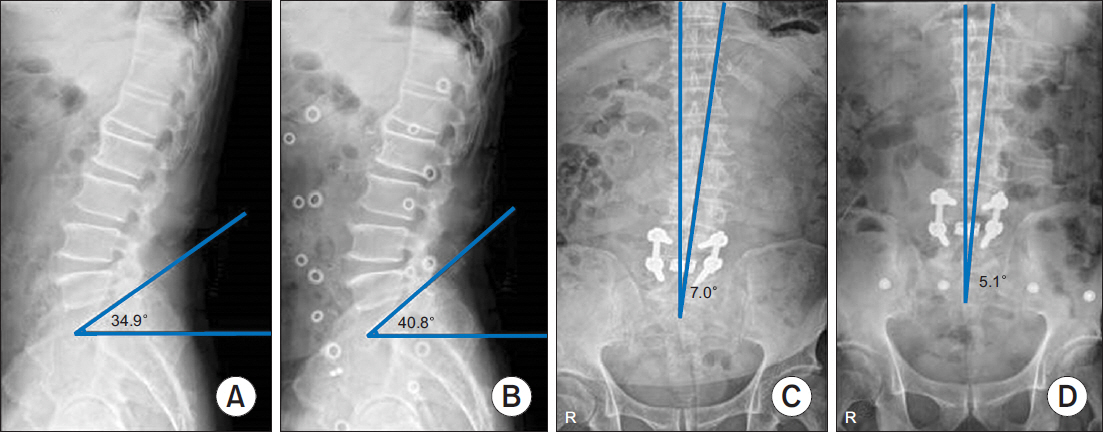
This prospective cohort study was performed from May 2019 to November 2019 and enrolled and analyzed 88 patients with degenerative lumbar spine disease scheduled for elective lumbar surgery. Three types of LSO that were provided according to the time of patient registration were applied for 6 weeks. Patients were randomized into the classic LSO group (n=31), Cybertech group (n=26), and V-LSO group (n=31). All patients were assessed using the Oswestry Disability Index (ODI) preoperatively and underwent plain lumbar radiography (anteroposterior and lateral views) 10 days postoperatively. Lumbar lordosis (LS angle) and frontal imbalance were measured with and without LSO. At the sixth postoperative week, a follow-up assessment with the ODI and orthosis questionnaire was conducted.
Results
No significant differences were found among the three groups in terms of the LS angle, frontal imbalance, ODI, and orthosis questionnaire results. When the change in the LS angle and frontal imbalance toward the reference value was defined as a positive change with and without LSO, the rate of positive change was significantly different in the V-LSO group (LS angle: 41.94% vs. 61.54% vs. 83.87%; p=0.003).
Conclusion
The newly developed LSO showed no difference regarding its effectiveness and compliance when compared with the existing LSO, but it was more effective in correcting lumbar lordosis.
Figure
Reference
-
1. Soliman HA, Barchi S, Parent S, Maurais G, Jodoin A, Mac-Thiong JM. Early impact of postoperative bracing on pain and quality of life after posterior instrumented fusion for lumbar degenerative conditions: a randomized trial. Spine (Phila Pa 1976). 2018; 43:155–60.2. Machado GC, Ferreira PH, Yoo RI, Harris IA, Pinheiro MB, Koes BW, et al. Surgical options for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016; 11:CD012421.
Article3. Connolly PJ, Grob D. Bracing of patients after fusion for degenerative problems of the lumbar spine: yes or no? Spine (Phila Pa 1976). 1998; 23:1426–8.4. Bogaert L, Van Wambeke P, Thys T, Swinnen TW, Dankaerts W, Brumagne S, et al. Postoperative bracing after lumbar surgery: a survey amongst spinal surgeons in Belgium. Eur Spine J. 2019; 28:442–9.
Article5. Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN. Postoperative bracing after spine surgery for degenerative conditions: a questionnaire study. Spine J. 2009; 9:309–16.
Article6. Agabegi SS, Asghar FA, Herkowitz HN. Spinal orthoses. J Am Acad Orthop Surg. 2010; 18:657–67.
Article7. Nachemson A, Schultz A, Andersson G. Mechanical effectiveness studies of lumbar spine orthoses. Scand J Rehabil Med Suppl. 1983; 9:139–49.8. Azadinia F, Ebrahimi E Takamjani, Kamyab M, Parnianpour M, Cholewicki J, et al. Can lumbosacral orthoses cause trunk muscle weakness? A systematic review of literature. Spine J. 2017; 17:589–602.
Article9. Cho KH, Beom JW, Lee TS, Lim JH, Lee TH, Yuk JH. Trunk muscles strength as a risk factor for nonspecific low back pain: a pilot study. Ann Rehabil Med. 2014; 38:234–40.
Article10. Lee JH, Hoshino Y, Nakamura K, Kariya Y, Saita K, Ito K. Trunk muscle weakness as a risk factor for low back pain: a 5-year prospective study. Spine (Phila Pa 1976). 1999; 24:54–7.11. Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011; 90:805–15.12. Sato N, Sekiguchi M, Kikuchi S, Shishido H, Sato K, Konno S. Effects of long-term corset wearing on chronic low back pain. Fukushima J Med Sci. 2012; 58:60–5.
Article13. Krag MH, Fox MS J, Haugh LD. Comparison of three lumbar orthoses using motion assessment during task performance. Spine (Phila Pa 1976). 2003; 28:2359–67.
Article14. Fujimoto Y, Sakai T, Sairyo K. What type of orthosis is optimal for conservative treatment of lumbar spondylolysis?: a biomechanical analysis. Spine Surg Relat Res. 2019; 4:74–80.
Article15. Cholewicki J, Lee AS, Peter Reeves N, Morrisette DC. Comparison of trunk stiffness provided by different design characteristics of lumbosacral orthoses. Clin Biomech (Bristol, Avon). 2010; 25:110–4.
Article16. Hellems HK Jr, Keats TE. Measurement of the normal lumbosacral angle. Am J Roentgenol Radium Ther Nucl Med. 1971; 113:642–5.
Article17. Dillane JB, Fry J, Kalton G. Acute back syndrome: a study from general practice. Br Med J. 1966; 2:82–4.18. Ferguson AB. The clinical and roentgenographic interpretation of lumbosacral anomalies. Radiology. 1934; 22:548–58.
Article19. Meschan I, Farrer-Meschan RM. Important aspects in the roentgen study of the normal lumbosacral spine. Radiology. 1958; 70:637–48.
Article20. Moreton RD, Winston JR, Bibey DE, Williams C. Radiologic considerations in preplacement examinations of the lumbar spine; summary of four thousand consecutive cases. Radiology. 1954; 63:667–72.21. Okpala FO. Comparison of four radiographic angular measures of lumbar lordosis. J Neurosci Rural Pract. 2018; 9:298–304.
Article22. Tuong NH, Dansereau J, Maurais G, Herrera R. Three-dimensional evaluation of lumbar orthosis effects on spinal behavior. J Rehabil Res Dev. 1998; 35:34–42.23. Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002; 82:8–24.
Article24. Fairbank JC. Oswestry disability index. J Neurosurg Spine. 2014; 20:239–41.25. Curfs I, van Rooij W, Senden R, Grimm B, Van Hemert W. Evaluating the immobilization effect of spinal orthoses using sensor-based motion analysis. J Prosthet Orthot. 2016; 28:23–9.
Article26. Utter A, Anderson ML, Cunniff JG, Kaufman KR, Jelsing EJ, Patrick TA, et al. Video fluoroscopic analysis of the effects of three commonly-prescribed off-the-shelf orthoses on vertebral motion. Spine (Phila Pa 1976). 2010; 35:E525–9.
Article27. Yao YC, Lin HH, Chang MC. Bracing following transforaminal lumbar interbody fusion is not necessary for patients with degenerative lumbar spine disease: a prospective, randomized trial. Clin Spine Surg. 2018; 31:E441–5.28. Yee AJ, Yoo JU, Marsolais EB, Carlson G, Poe-Kochert C, Bohlman HH, et al. Use of a postoperative lumbar corset after lumbar spinal arthrodesis for degenerative conditions of the spine: a prospective randomized trial. J Bone Joint Surg Am. 2008; 90:2062–8.29. Nasi D, Dobran M, Pavesi G. The efficacy of postoperative bracing after spine surgery for lumbar degenerative diseases: a systematic review. Eur Spine J. 2020; 29:321–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of orthoses for treatment in patients with spinal pain
- Relative Contribution of Upper and Lower Lumbar Spinal Segments to Flexion/Extension: Comparison between Normal Spines and Spines with Disc Disease in Asian Patients
- Treatment for the Lumbosacral Soft Tissue Defect after Spine Surgery
- A Comparison of Interside Asymmetries of Lower Extremity Somatosensory Evoked Potentials in Anesthetized Patients with Unilateral Lumbosacral Radiculopathy
- Preemptive Caudal Ropivacaine: An Effective Analgesic during Degenerative Lumbar Spine Surgery