Ewha Med J.
2021 Jan;44(1):19-25. 10.12771/emj.2021.44.1.19.
Correlation between Systolic Blood Pressure and Triglyceride Level in the Uzbekistan Population
- Affiliations
-
- 1Ewha Womans University School of Medicine, Seoul, Korea
- 2Department of Nursing, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- 3Departments of Emergency Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 4Departments of Cardiology, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2512408
- DOI: http://doi.org/10.12771/emj.2021.44.1.19
Abstract
Objectives
: This study aimed to characteristic the systolic blood pressure (SBP), diastolic pressure, pulse pressure, glucose, creatine, and lipid profile. This study also aimed to investigate the prevalence of hypertension and the relationship between hypertension and the lipid profile in Uzbekistan.
Methods
The subjects consisted of 58 Uzbekistan subjects recruited from Ewha Medical Care patients. Blood samples were collected from the patients for the lipid profile and random glucose and creatinine levels. Paired t tests were used for the group means and a chi-square or Fisher’s exact test for categorical variables. A multiple logistic regression analysis was performed.
Results
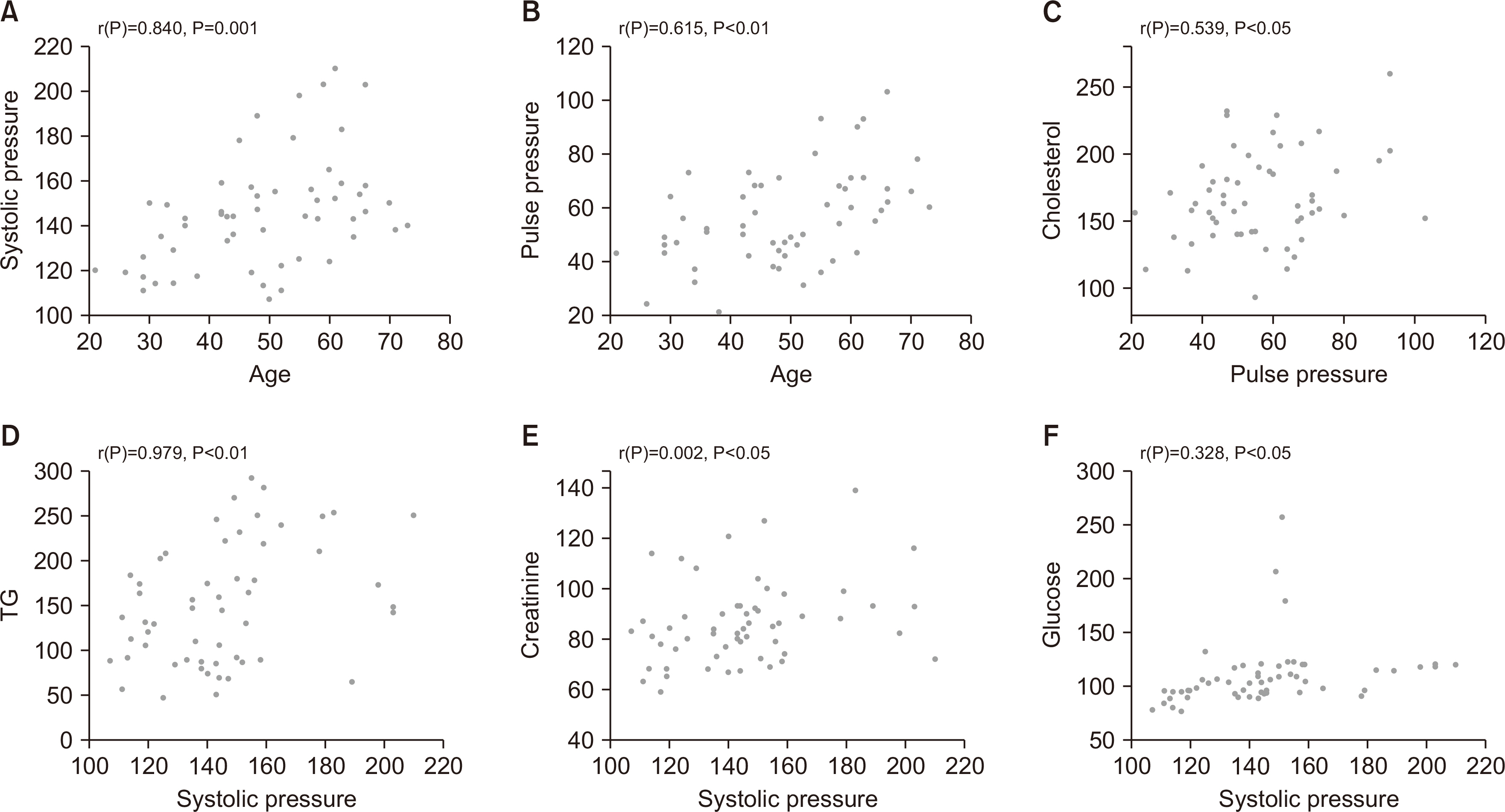
Among the 58 patients constituting the baseline population, hypertension developed in 42 patients. Among them, the triglyceride (TG) level was significantly higher in the hypertension group than normal group (173.19 vs. 127.06 mg/dL, P=0.014). The SBP had a positive correlation with the TG (r=0.979, P<0.01) and creatinine (r=0.002, P<0.05) levels and also, the pulse pressure had a positive correlation with the cholesterol level (r=0.539, P<0.05). A multivariate analysis (adjusted for age and sex) indicated that there was a positive correlation between the SBP and TG level (r=0.941, P<0.05).
Conclusion
There was a positive correlation between the SBP and TG level in the Uzbekistan population according to this study.
Keyword
Figure
Reference
-
1. World Health Organization. 2018. The top 10 causes of death. World Health Organization;Geneva:2. World Health Organization. 2015. Uzbekistan: WHO statistical profile. World Health Organization;Geneva:3. McKee PA, Castelli WP, McNamara PM, Kannel WB. 1971; The natural history of congestive heart failure: the Framingham study. N Engl J Med. 285:1441–1446. DOI: 10.1056/NEJM197112232852601. PMID: 5122894.
Article4. Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. 1977; High density lipoprotein as a protective factor against coronary heart disease: the Framingham Study. Am J Med. 62:707–714. DOI: 10.1016/0002-9343(77)90874-9. PMID: 193398.5. Williams RR, Hunt SC, Hopkins PN, Stults BM, Wu LL, Hasstedt SJ, et al. 1988; Familial dyslipidemic hypertension. Evidence from 58 Utah families for a syndrome present in approximately 12% of patients with essential hypertension. JAMA. 259:3579–3586. DOI: 10.1001/jama.1988.03720240041032. PMID: 3373705.
Article6. Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. 2011; Outdoor temperature is associated with serum HDL and LDL. Environ Res. 111:281–287. DOI: 10.1016/j.envres.2010.12.001. PMID: 21172696. PMCID: PMC4437587.
Article7. World Meteorological Organization. c2020. World weather information service: Tashkent, Uzbekistan [Internet]. World Meteorological Organization;Geneva: Available from: https://worldweather.wmo.int/en/city.html?.cityId=115. cited 2020 Jun 18.8. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2018; 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 71:e13–e115. DOI: 10.1161/HYP.0000000000000065. PMCID: PMC5945323. PMID: 29133356.
Article9. White KT, Moorthy MV, Akinkuolie AO, Demler O, Ridker PM, Cook NR, et al. 2015; Identifying an optimal cutpoint for the diagnosis of hypertriglyceridemia in the nonfasting state. Clin Chem. 61:1156–1163. DOI: 10.1373/clinchem.2015.241752. PMID: 26071491. PMCID: PMC4554926.
Article10. Nordestgaard BG, Langsted A, Mora S, Kolovou G, Baum H, Bruckert E, et al. 2016; Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cut-points-a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Eur Heart J. 37:1944–1958. DOI: 10.1093/eurheartj/ehw152. PMID: 27122601. PMCID: PMC4929379.
Article11. American Diabetes Association. 2014; Diagnosis and classification of diabetes mellitus. Diabetes Care. 37(Suppl 1):S81–S90. DOI: 10.2337/dc14-S081. PMID: 24357215.12. Mishra V, Arnold F, Semenov G, Hong R, Mukuria A. 2006; Epidemiology of obesity and hypertension and related risk factors in Uzbekistan. Eur J Clin Nutr. 60:1355–1366. DOI: 10.1038/sj.ejcn.1602465. PMID: 16788710.
Article13. Aringazina A, Kuandikov T, Arkhipov V. 2018; Burden of the cardiovascular diseases in Central Asia. Cent Asian J Glob Health. 7:321. DOI: 10.5195/CAJGH.2018.321. PMID: 30863664. PMCID: PMC6393056.
Article14. Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. 2008; A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med. 148:102–110. DOI: 10.7326/0003-4819-148-2-200801150-00005. PMID: 18195335.
Article15. Benetos A, Waeber B, Izzo J, Mitchell G, Resnick L, Asmar R, et al. 2002; Influence of age, risk factors, and cardiovascular and renal disease on arterial stiffness: clinical applications. Am J Hypertens. 15:1101–1108. DOI: 10.1016/S0895-7061(02)03029-7. PMID: 12460708.
Article16. Benetos A, Safar M, Rudnichi A, Smulyan H, Richard JL, Ducimetieere P, et al. 1997; Pulse pressure: a predictor of long-term cardiovascular mortality in a French male population. Hypertension. 30:1410–1415. DOI: 10.1161/01.HYP.30.6.1410. PMID: 9403561.17. Mitchell GF, Moye LA, Braunwald E, Rouleau JL, Bernstein V, Geltman EM, et al. 1997; Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. SAVE investigators. Survival and Ventricular Enlargement. Circulation. 96:4254–4260. DOI: 10.1161/01.CIR.96.12.4254. PMID: 9416890.18. Franklin SS, Khan SA, Wong ND, Larson MG, Levy D. 1999; Is pulse pressure useful in predicting risk for coronary heart Disease? The Framingham heart study. Circulation. 100:354–360. DOI: 10.1161/01.CIR.100.4.354. PMID: 10421594.19. Benetos A, Zureik M, Morcet J, Thomas F, Bean K, Safar M, et al. 2000; A decrease in diastolic blood pressure combined with an increase in systolic blood pressure is associated with a higher cardiovascular mortality in men. J Am Coll Cardiol. 35:673–680. DOI: 10.1016/S0735-1097(99)00586-0. PMID: 10716470.
Article20. Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. 2001; Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 37:1236–1241. DOI: 10.1161/01.HYP.37.5.1236. PMID: 11358934.
Article21. Perry HM Jr, Miller JP, Fornoff JR, Baty JD, Sambhi MP, Rutan G, et al. 1995; Early predictors of 15-year end-stage renal disease in hypertensive patients. Hypertension. 25(4 Pt 1):587–594. DOI: 10.1161/01.HYP.25.4.587. PMID: 7721402.
Article22. Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, et al. 1996; Blood pressure and end-stage renal disease in men. N Engl J Med. 334:13–18. DOI: 10.1056/NEJM199601043340103. PMID: 7494564.
Article23. Emdin CA, Anderson SG, Woodward M, Rahimi K. 2015; Usual blood pressure and risk of new-onset diabetes: evidence from 4.1 million adults and a meta-analysis of prospective studies. J Am Coll Cardiol. 66:1552–1562. DOI: 10.1016/j.jacc.2015.07.059. PMID: 26429079. PMCID: PMC4595710.24. McCarty MF. 2003; Does postprandial storage of triglycerides in endothelial cells contribute to the endothelial dysfunction associated with insulin resistance and fatty diets? Med Hypotheses. 61:167–172. DOI: 10.1016/S0306-9877(02)00236-0. PMID: 12888297.
Article25. Lundman P, Eriksson M, Schenck-Gustafsson K, Karpe F, Tornvall P. 1997; Transient triglyceridemia decreases vascular reactivity in young, healthy men without risk factors for coronary heart disease. Circulation. 96:3266–3268. DOI: 10.1161/01.CIR.96.10.3266. PMID: 9396413.
Article26. Fadini GP, de Kreutzenberg S, Agostini C, Boscaro E, Tiengo A, Dimmeler S, et al. 2009; Low CD34+ cell count and metabolic syndrome synergistically increase the risk of adverse outcomes. Atherosclerosis. 207:213–219. DOI: 10.1016/j.atherosclerosis.2009.03.040. PMID: 19406403.
Article27. Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, et al. 2003; Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 348:593–600. DOI: 10.1056/NEJMoa022287. PMID: 12584367.
Article28. Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. 2019; Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 380:11–22. DOI: 10.1056/NEJMoa1812792. PMID: 30415628.
Article29. Meneton P, Jeunemaitre X, de Wardener HE, MacGregor GA. 2005; Links between dietary salt intake, renal salt handling, blood pressure, and cardiovascular diseases. Physiol Rev. 85:679–715. DOI: 10.1152/physrev.00056.2003. PMID: 15788708.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inter-relationships between arteriosclerotic risk factors: a meta-analysis
- Radiation Safety and Radiologist Working Hours in Uzbekistan
- Blood pressure measurement of school-aged children in Goesan
- The Change of Children's Blood Pressure and Factors Affecting the Level of Blood Pressure In Children
- A Study on Blood Pressure and Serum Biochemical Indices of Cerebrovascular Accident Patients in Korean Urban Adults