Clin Endosc.
2021 Jan;54(1):113-121. 10.5946/ce.2020.083.
Cyst Fluid Carcinoembryonic Antigen Level Difference between Mucinous Cystic Neoplasms and Intraductal Papillary Mucinous Neoplasms
- Affiliations
-
- 1Department of Gastroenterology, Bezmialem Vakif University Medicine Faculty, Istanbul, Turkey
- 2Department of Pathology, Bezmialem Vakif University Medicine Faculty, Istanbul, Turkey
- 3Department of General Surgery, Bezmialem Vakif University Medicine Faculty, Istanbul, Turkey
- 4Department of Biostatistics, Bezmialem Vakif University Medicine Faculty, Istanbul, Turkey
- KMID: 2512316
- DOI: http://doi.org/10.5946/ce.2020.083
Abstract
- Background/Aims
The role of cyst fluid carcinoembryonic antigen (CEA) level in differentiating mucinous pancreatic cystic lesions (PCLs) is controversial. We investigated the role of cyst fluid CEA in differentiating low-risk (LR)-intraductal papillary mucinous neoplasms (IPMNs) from high-risk (HR)-IPMNs and LR-mucinous cystic neoplasms (MCNs).
Methods
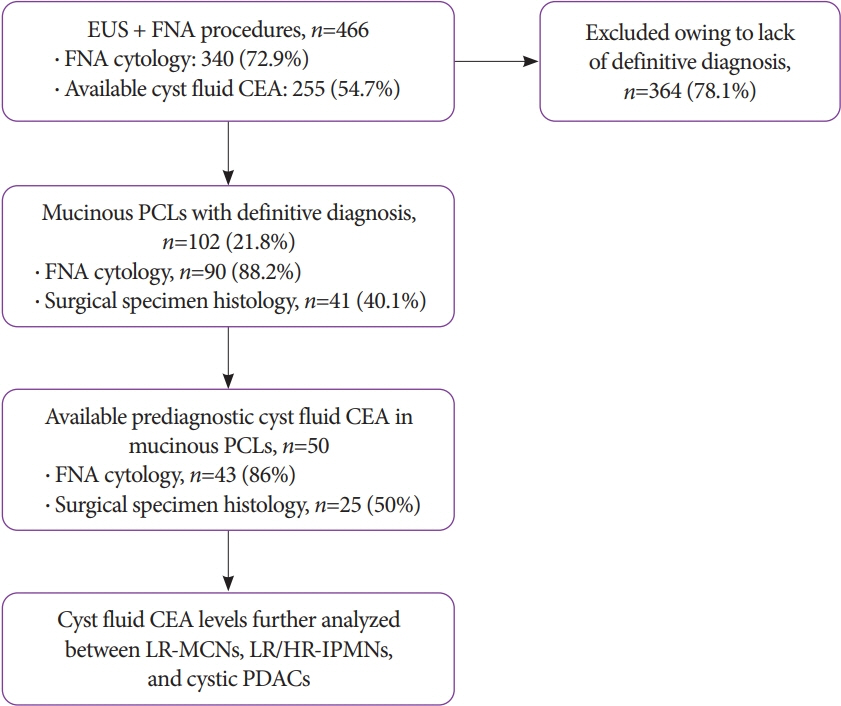
This was a retrospective study of 466 patients with PCLs who underwent endoscopic ultrasound-guided fine-needleaspiration over a 7-year period. On histology, low-grade dysplasia and intermediate-grade dysplasia were considered LR, whereas high-grade dysplasia and invasive carcinoma were considered HR.
Results
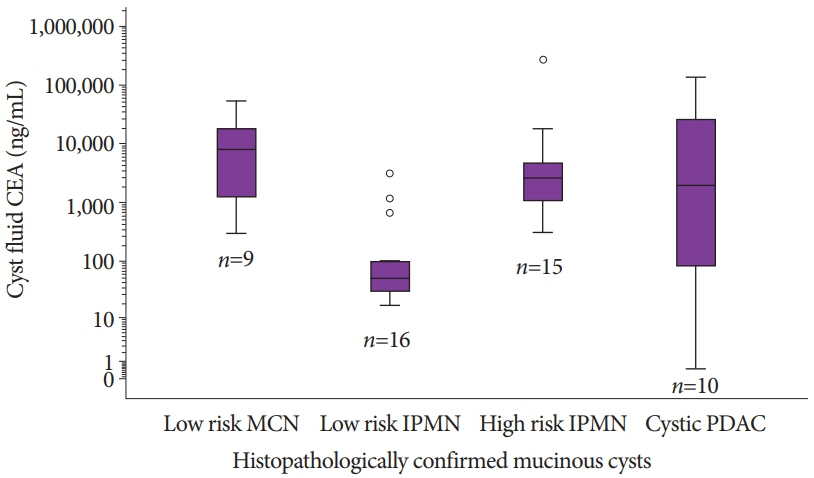
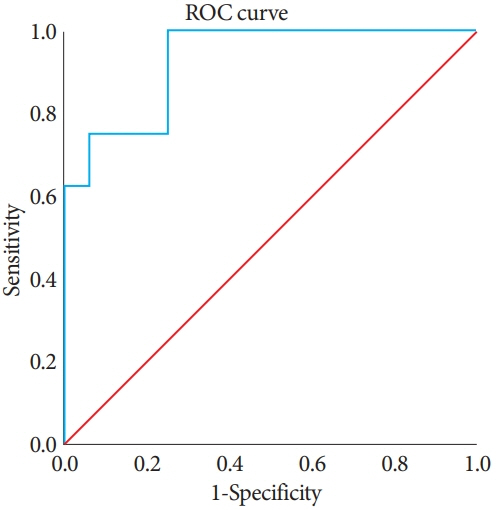
Data on cyst fluid CEA levels were available for 50/102 mucinous PCLs with definitive diagnoses. The median CEA (range) levels were significantly higher in HR cysts than in LR cysts (2,624 [0.5–266,510] ng/mL vs. 100 [16.8–53,445]ng/mL, p=0.0012). The area under the receiver operating characteristic curve (AUROC) was 0.930 (95% confidence interval [CI], 0.5–0.8; p<0.001) for differentiating LR-IPMNs from LR-MCNs. The AUROC was 0.921 (95% CI, 0.823–1.000; p<0.001) for differentiating LR-IPMNs from HR-IPMNs. Both had a CEA cutoff level of >100ng/mL, with a negative predictive value (NPV) of 100%.
Conclusions
Cyst fluid CEA levels significantly vary between LR-IPMNs, LR-MCNs, and HR-IPMNs. A CEA cutoff level of >100ng/mL had a 100% NPV in differentiating LR-IPMNs from LR-MCNs and HR-IPMNs.
Figure
Cited by 1 articles
-
Is Carcinoembryonic Antigen the Holy Grail for Pancreatic Cyst Risk Stratification?
Ahmad Najdat Bazarbashi, Linda S. Lee
Clin Endosc. 2021;54(1):7-8. doi: 10.5946/ce.2021.046.
Reference
-
1. Zerboni G, Signoretti M, Crippa S, Falconi M, Arcidiacono PG, Capurso G. Systematic review and meta-analysis: prevalence of incidentally detected pancreatic cystic lesions in asymptomatic individuals. Pancreatology. 2019; 19:2–9.
Article2. Basturk O, Coban I, Adsay NV. Pancreatic cysts: pathologic classification, differential diagnosis, and clinical implications. Arch Pathol Lab Med. 2009; 133:423–438.
Article3. van Huijgevoort NCM, Del Chiaro M, Wolfgang CL, van Hooft JE, Besselink MG. Diagnosis and management of pancreatic cystic neoplasms: current evidence and guidelines. Nat Rev Gastroenterol Hepatol. 2019; 16:676–689.4. Sentürk H. Management of cystic diseases of the pancreas. Turk J Gastroenterol. 2014; 25:1–18.
Article5. Basturk O, Hong SM, Wood LD, et al. A revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol. 2015; 39:1730–1741.
Article6. Adsay NV, Fukushima N, Furukawa T, et al. Intraductal neoplasms of the pancreas. In : Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumours of the digestive system. 4th ed. Lyon: International Agency for Research on Cancer;2010. p. 304–313.7. Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006; 6:17–32.
Article8. Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12:183–197.
Article9. Senturk H, Köker IH, Keskin EB, Ünver N, Ince AT, Basaranoglu M. Needle based confocal laser endomicroscopy examination of pancreatic cysts: single center real life results. Gastroenterology. 2018; 154(6 Suppl 1):S–528.10. Basar O, Yuksel O, Yang DJ, et al. Feasibility and safety of microforceps biopsy in the diagnosis of pancreatic cysts. Gastrointest Endosc. 2018; 88:79–86.
Article11. Mittal C, Obuch JC, Hammad H, et al. Technical feasibility, diagnostic yield, and safety of microforceps biopsies during EUS evaluation of pancreatic cystic lesions (with video). Gastrointest Endosc. 2018; 87:1263–1269.
Article12. Oh SH, Lee JK, Lee KT, Lee KH, Woo YS, Noh DH. The combination of cyst fluid carcinoembryonic antigen, cytology and viscosity increases the diagnostic accuracy of mucinous pancreatic cysts. Gut Liver. 2017; 11:283–289.
Article13. Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.
Article14. European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018; 67:789–804.15. Elta GH, Enestvedt BK, Sauer BG, Lennon AM. ACG clinical guideline: diagnosis and management of pancreatic cysts. Am J Gastroenterol. 2018; 113:464–479.
Article16. Brugge WR, Lewandrowski K, Lee-Lewandrowski E, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004; 126:1330–1336.
Article17. van der Waaij LA, van Dullemen HM, Porte RJ. Cyst fluid analysis in the differential diagnosis of pancreatic cystic lesions: a pooled analysis. Gastrointest Endosc. 2005; 62:383–389.
Article18. Nagula S, Kennedy T, Schattner MA, et al. Evaluation of cyst fluid CEA analysis in the diagnosis of mucinous cysts of the pancreas. J Gastrointest Surg. 2010; 14:1997–2003.
Article19. Park WG, Mascarenhas R, Palaez-Luna M, et al. Diagnostic performance of cyst fluid carcinoembryonic antigen and amylase in histologically confirmed pancreatic cysts. Pancreas. 2011; 40:42–45.
Article20. Cizginer S, Turner BG, Bilge AR, Karaca C, Pitman MB, Brugge WR. Cyst fluid carcinoembryonic antigen is an accurate diagnostic marker of pancreatic mucinous cysts. Pancreas. 2011; 40:1024–1028.
Article21. Al-Rashdan A, Schmidt CM, Al-Haddad M, et al. Fluid analysis prior to surgical resection of suspected mucinous pancreatic cysts. A single centre experience. J Gastrointest Oncol. 2011; 2:208–214.22. Ngamruengphong S, Bartel MJ, Raimondo M. Cyst carcinoembryonic antigen in differentiating pancreatic cysts: a meta-analysis. Dig Liver Dis. 2013; 45:920–926.
Article23. Nagashio Y, Hijioka S, Mizuno N, et al. Combination of cyst fluid CEA and CA 125 is an accurate diagnostic tool for differentiating mucinous cystic neoplasms from intraductal papillary mucinous neoplasms. Pancreatology. 2014; 14:503–509.
Article24. Gaddam S, Ge PS, Keach JW, et al. Suboptimal accuracy of carcinoembryonic antigen in differentiation of mucinous and nonmucinous pancreatic cysts: results of a large multicenter study. Gastrointest Endosc. 2015; 82:1060–1069.
Article25. Kawai M, Uchiyama K, Tani M, et al. Clinicopathological features of malignant intraductal papillary mucinous tumors of the pancreas: the differential diagnosis from benign entities. Arch Surg. 2004; 139:188–192.26. Maire F, Voitot H, Aubert A, et al. Intraductal papillary mucinous neoplasms of the pancreas: performance of pancreatic fluid analysis for positive diagnosis and the prediction of malignancy. Am J Gastroenterol. 2008; 103:2871–2877.
Article27. Oppong KW, Dawwas MF, Charnley RM, et al. EUS and EUS-FNA diagnosis of suspected pancreatic cystic neoplasms: is the sum of the parts greater than the CEA? Pancreatology. 2015; 15:531–537.
Article28. Correa-Gallego C, Warshaw AL, Fernandez-del Castillo C. Fluid CEA in IPMNs: a useful test or the flip of a coin? Am J Gastroenterol. 2009; 104:796–797.
Article29. Kucera S, Centeno BA, Springett G, et al. Cyst fluid carcinoembryonic antigen level is not predictive of invasive cancer in patients with intraductal papillary mucinous neoplasm of the pancreas. JOP. 2012; 13:409–413.30. Scourtas A, Dudley JC, Brugge WR, Kadayifci A, Mino-Kenudson M, Pitman MB. Preoperative characteristics and cytological features of 136 histologically confirmed pancreatic mucinous cystic neoplasms. Cancer Cytopathol. 2017; 125:169–177.
Article31. Hayakawa H, Fukasawa M, Sato T, et al. Carcinoembryonic antigen level in the pancreatic juice is effective in malignancy diagnosis and prediction of future malignant transformation of intraductal papillary mucinous neoplasm of the pancreas. J Gastroenterol. 2019; 54:1029–1037.
Article32. Hirono S, Kawai M, Okada KI, et al. Factors associated with invasive intraductal papillary mucinous carcinoma of the pancreas. JAMA Surg. 2017; 152:e165054.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Mucinous Cystic Tumor and Intraductal Papillary Mucinous Tumor
- Cystic Neoplasms and Intraductal Papillary Mucinous Neoplasms of the Pancreas
- Oncocytic Type Intraductal Papillary Mucinous Neoplasm Mimicking Mucinous Cystic Neoplasm of the Pancreas: A Case Report
- A Case of Epidermoid Cyst in the Intrapancreatic Accessory Spleen Mimicking Pancreas Mucinous Cystic Neoplasm
- Mucinous Non-neoplastic Cyst of the Pancreas