J Surg Ultrasound.
2020 Nov;7(2):21-28. 10.46268/jsu.2020.7.2.21.
Efficacy of Ultrasound-Guided Core Needle Biopsy in Detecting Metastatic Axillary Lymph Nodes in Breast Cancer
- Affiliations
-
- 1Department of Surgery, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2511907
- DOI: http://doi.org/10.46268/jsu.2020.7.2.21
Abstract
- Purpose
Axillary lymph node status is an important prognostic factor in breast cancer. Axillary lymph nodes can be evaluated using fine-needle aspiration cytology (FNAC) or core needle biopsy (CNB) before surgery. This study compared the accuracy and false-negative rates between FNAC and CNB in patients with breast cancer who either did or did not receive neoadjuvant chemotherapy (NAC).
Methods
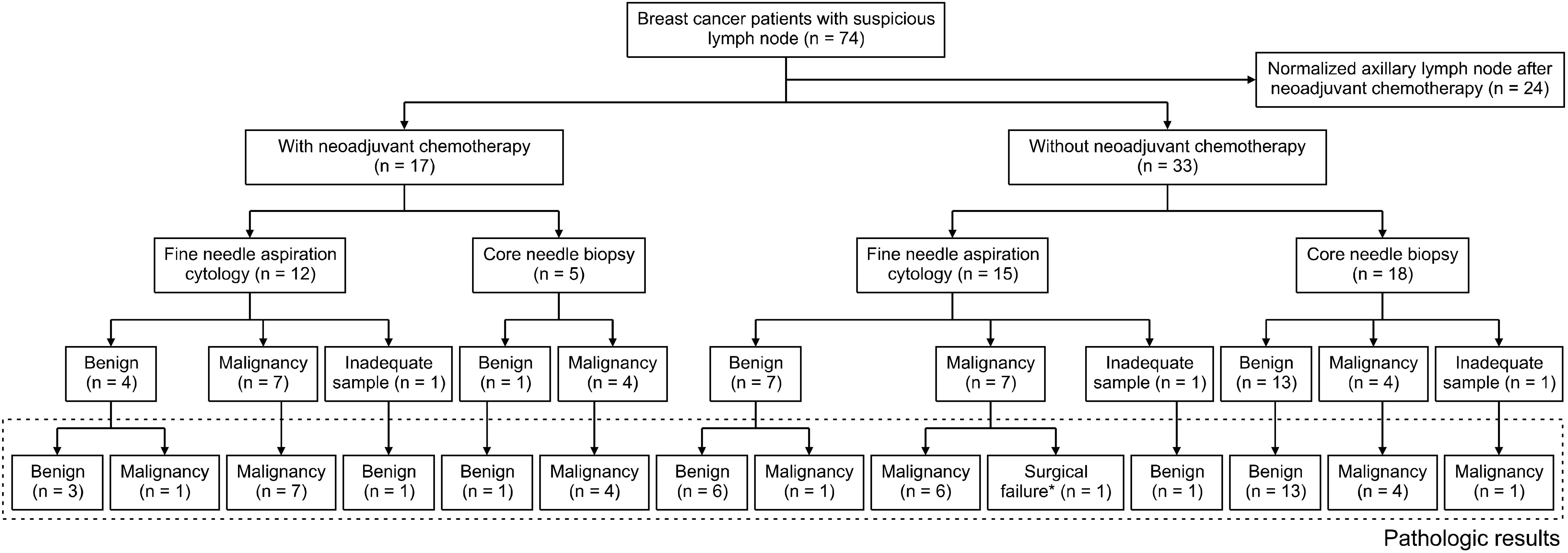
The clinicopathological factors of the patients were analyzed retrospectively, and the sensitivity, specificity, positive and negative predictive values, false-positive and false-negative rates, and accuracy of FNAC (n = 27) and CNB (n = 23) were compared.
Results
Regardless of whether or not NAC was performed, the CNB evaluation of the metastatic axillary lymph nodes had a 100.0% sensitivity, specificity, negative predictive value, and accuracy, except for one case with an inadequate sample. In the FNAC group, the false-negative rate was higher in patients with breast cancer who received NAC before evaluating the lymph nodes (9.1% vs. 7.7%). Moreover, ultrasound imaging was the most sensitive imaging modality that can detect the suspicious axillary lymph node.
Conclusion
CNB was more effective in evaluating the axillary lymph nodes in breast cancer than FNAC and was performed without major complications.
Keyword
Figure
Reference
-
1. Reynolds C, Mick R, Donohue JH, Grant CS, Farley DR, Callans LS, et al. 1999; Sentinel lymph node biopsy with metastasis: can axillary dissection be avoided in some patients with breast cancer? J Clin Oncol. 17:1720–6. DOI: 10.1200/JCO.1999.17.6.1720. PMID: 10561208.
Article2. Lovrics PJ, Chen V, Coates G, Cornacchi SD, Goldsmith CH, Law C, et al. 2004; A prospective evaluation of positron emission tomography scanning, sentinel lymph node biopsy, and standard axillary dissection for axillary staging in patients with early stage breast cancer. Ann Surg Oncol. 11:846–53. DOI: 10.1245/ASO.2004.11.033. PMID: 15313737.
Article3. Langer I, Guller U, Berclaz G, Koechli OR, Schaer G, Fehr MK, et al. 2007; Morbidity of sentinel lymph node biopsy (SLN) alone versus SLN and completion axillary lymph node dissection after breast cancer surgery: a prospective Swiss multicenter study on 659 patients. Ann Surg. 245:452–61. DOI: 10.1097/01.sla.0000245472.47748.ec. PMID: 17435553. PMCID: PMC1877006.4. Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. 2003; A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 349:546–53. DOI: 10.1056/NEJMoa012782. PMID: 12904519.
Article5. Gipponi M, Bassetti C, Canavese G, Catturich A, Di Somma C, Vecchio C, et al. 2004; Sentinel lymph node as a new marker for therapeutic planning in breast cancer patients. J Surg Oncol. 85:102–11. DOI: 10.1002/jso.20022. PMID: 14991881.
Article6. Sanuki N, Takeda A, Amemiya A, Ofuchi T, Ono M, Ogata H, et al. 2013; Outcomes of clinically node-negative breast cancer without axillary dissection: can preserved axilla be safely treated with radiation after a positive sentinel node biopsy? Clin Breast Cancer. 13:69–76. DOI: 10.1016/j.clbc.2012.09.005. PMID: 23062706.
Article7. Gentilini O, Veronesi U. 2012; Abandoning sentinel lymph node biopsy in early breast cancer? A new trial in progress at the European Institute of Oncology of Milan (SOUND: Sentinel node vs Observation after axillary UltraSouND). Breast. 21:678–81. DOI: 10.1016/j.breast.2012.06.013. PMID: 22835916.8. van Roozendaal LM, Vane MLG, van Dalen T, van der Hage JA, Strobbe LJA, Boersma LJ, et al. 2017; Clinically node negative breast cancer patients undergoing breast conserving therapy, sentinel lymph node procedure versus follow-up: a Dutch randomized controlled multicentre trial (BOOG 2013-08). BMC Cancer. 17:459. DOI: 10.1186/s12885-017-3443-x. PMID: 28668073. PMCID: PMC5494134.
Article9. Yu YH, Mo QG, Zhu X, Gao LQ, Liang C, Huang Z, et al. 2016; Axillary fine needle aspiration cytology is a sensitive and highly specific technique for the detection of axillary lymph node metastasis: a meta-analysis and systematic review. Cytopathology. 27:59–69. DOI: 10.1111/cyt.12224. PMID: 25496004.
Article10. Rautiainen S, Masarwah A, Sudah M, Sutela A, Pelkonen O, Joukainen S, et al. 2013; Axillary lymph node biopsy in newly diagnosed invasive breast cancer: comparative accuracy of fine-needle aspiration biopsy versus core-needle biopsy. Radiology. 269:54–60. DOI: 10.1148/radiol.13122637. PMID: 23771915.
Article11. Bhandari A, Xia E, Wang Y, Sindan N, Kc R, Guan Y, et al. 2018; Impact of sentinel lymph node biopsy in newly diagnosed invasive breast cancer patients with suspicious node: a comparative accuracy survey of fine-needle aspiration biopsy versus core-needle biopsy. Am J Transl Res. 10:1860–73. PMID: 30018726. PMCID: PMC6038083.12. Kane G, Fleming C, Heneghan H, McCartan D, James P, Trueick R, et al. 2019; False-negative rate of ultrasound-guided fine-needle aspiration cytology for identifying axillary lymph node metastasis in breast cancer patients. Breast J. 25:848–52. DOI: 10.1111/tbj.13402. PMID: 31197915.
Article13. Ewing DE, Layfield LJ, Joshi CL, Travis MD. 2015; Determinants of false-negative fine-needle aspirates of axillary lymph nodes in women with breast cancer: lymph node size, cortical thickness and hilar fat retention. Acta Cytol. 59:311–4. DOI: 10.1159/000440797. PMID: 26422248.
Article14. Wang Y, Dong H, Wu H, Zhang L, Yuan K, Chen H, et al. 2015; Improved false negative rate of axillary status using sentinel lymph node biopsy and ultrasound-suspicious lymph node sampling in patients with early breast cancer. BMC Cancer. 15:382. DOI: 10.1186/s12885-015-1331-9. PMID: 25956308. PMCID: PMC4435774.
Article15. Vidya R, Iqbal FM, Bickley B. 2017; Pre-operative axillary staging: should core biopsy be preferred to fine needle aspiration cytology? Ecancermedicalscience. 11:724. DOI: 10.3332/ecancer.2017.724. PMID: 28386294. PMCID: PMC5365337.
Article16. Fisher B, Redmond C, Poisson R, Margolese R, Wolmark N, Wickerham L, et al. 1989; Eight-year results of a randomized clinical trial comparing total mastectomy and lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 320:822–8. DOI: 10.1056/NEJM198903303201302. PMID: 2927449.
Article17. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. 2002; Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 347:1233–41. DOI: 10.1056/NEJMoa022152. PMID: 12393820.
Article18. Huang J, Mo Q, Zhuang Y, Qin Q, Huang Z, Mo J, et al. 2018; Oncological safety of nipple-sparing mastectomy in young patients with breast cancer compared with conventional mastectomy. Oncol Lett. 15:4813–20. DOI: 10.3892/ol.2018.7913. PMID: 29541245. PMCID: PMC5835917.
Article19. Caruso F, Ferrara M, Castiglione G, Trombetta G, De Meo L, Catanuto G, et al. 2006; Nipple sparing subcutaneous mastectomy: sixty-six months follow-up. Eur J Surg Oncol. 32:937–40. DOI: 10.1016/j.ejso.2006.05.013. PMID: 16829015.
Article20. Sacchini V, Pinotti JA, Barros AC, Luini A, Pluchinotta A, Pinotti M, et al. 2006; Nipple-sparing mastectomy for breast cancer and risk reduction: oncologic or technical problem? J Am Coll Surg. 203:704–14. DOI: 10.1016/j.jamcollsurg.2006.07.015. PMID: 17084333.
Article21. Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. 2014; Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 15:1303–10. DOI: 10.1016/S1470-2045(14)70460-7. PMID: 25439688. PMCID: PMC4291166.
Article22. Poodt IGM, Spronk PER, Vugts G, van Dalen T, Peeters MTFDV, Rots ML, et al. 2018; on axillary surgery in nondistant metastatic breast cancer patients treated between 2011 and 2015: a Dutch population-based study in the ACOSOG-Z0011 and AMAROS era. Ann Surg. 268:1084–90. DOI: 10.1097/SLA.0000000000002440. PMID: 28742702.23. Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. 2011; Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 305:569–75. DOI: 10.1001/jama.2011.90. PMID: 21304082. PMCID: PMC5389857.
Article24. Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. 2017; Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 318:918–26. DOI: 10.1001/jama.2017.11470. PMID: 28898379. PMCID: PMC5672806.
Article25. Akıncı M, Bulut SP, Erözgen F, Gürbüzel M, Gülşen G, Kocakuşak A, et al. 2016; Predictive value of fine needle aspiration biopsy of axillary lymph nodes in preoperative breast cancer staging. Ulus Cerrahi Derg. 32:191–6. DOI: 10.5152/UCD.2015.2913. PMID: 27528822. PMCID: PMC4970777.
Article26. Ganott MA, Zuley ML, Abrams GS, Lu AH, Kelly AE, Sumkin JH, et al. 2014; Ultrasound guided core biopsy versus fine needle aspiration for evaluation of axillary lymphadenopathy in patients with breast cancer. ISRN Oncol. 2014:703160. DOI: 10.1155/2014/703160. PMID: 24649373. PMCID: PMC3932200.
Article27. Nathanson SD. 2012; Ultrasound-guided core needle biopsy of axillary lymph nodes in breast cancer. J Am Coll Surg. 214:871–2. DOI: 10.1016/j.jamcollsurg.2012.02.002. PMID: 22520698.
Article28. Balasubramanian I, Fleming CA, Corrigan MA, Redmond HP, Kerin MJ, Lowery AJ. 2018; Meta-analysis of the diagnostic accuracy of ultrasound-guided fine-needle aspiration and core needle biopsy in diagnosing axillary lymph node metastasis. Br J Surg. 105:1244–53. DOI: 10.1002/bjs.10920. PMID: 29972239.
Article29. Solon JG, Power C, Al-Azawi D, Duke D, Hill AD. 2012; Ultrasound-guided core biopsy: an effective method of detecting axillary nodal metastases. J Am Coll Surg. 214:12–7. DOI: 10.1016/j.jamcollsurg.2011.09.024. PMID: 22079880.
Article30. Arslan G, Altintoprak KM, Yirgin IK, Atasoy MM, Celik L. 2016; Diagnostic accuracy of metastatic axillary lymph nodes in breast MRI. Springerplus. 5:735. DOI: 10.1186/s40064-016-2419-7. PMID: 27376003. PMCID: PMC4909659.
Article31. Kuijs VJ, Moossdorff M, Schipper RJ, Beets-Tan RG, Heuts EM, Keymeulen KB, et al. 2015; The role of MRI in axillary lymph node imaging in breast cancer patients: a systematic review. Insights Imaging. 6:203–15. DOI: 10.1007/s13244-015-0404-2. PMID: 25800994. PMCID: PMC4376816.
Article32. Hyun SJ, Kim EK, Moon HJ, Yoon JH, Kim MJ. 2016; Preoperative axillary lymph node evaluation in breast cancer patients by breast magnetic resonance imaging (MRI): can breast MRI exclude advanced nodal disease? Eur Radiol. 26:3865–73. DOI: 10.1007/s00330-016-4235-4. PMID: 26843011.
Article33. Nakamura R, Yamamoto N, Miyaki T, Itami M, Shina N, Ohtsuka M. 2018; Impact of sentinel lymph node biopsy by ultrasound-guided core needle biopsy for patients with suspicious node positive breast cancer. Breast Cancer. 25:86–93. DOI: 10.1007/s12282-017-0795-7. PMID: 28735457.
Article34. Rao R, Lilley L, Andrews V, Radford L, Ulissey M. 2009; Axillary staging by percutaneous biopsy: sensitivity of fine-needle aspiration versus core needle biopsy. Ann Surg Oncol. 16:1170–5. DOI: 10.1245/s10434-009-0421-9. PMID: 19263171.
Article35. Ahn HS, Kim SM, Jang M, Yun BL, Kim SW, Kang E, et al. 2013; Comparison of sonography with sonographically guided fine-needle aspiration biopsy and core-needle biopsy for initial axillary staging of breast cancer. J Ultrasound Med. 32:2177–84. DOI: 10.7863/ultra.32.12.2177. PMID: 24277901.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Ultrasound-Guided Fine Needle Aspiration in Breast Lesions
- The Safety and Efficiency of the Ultrasound-guided Large Needle Core Biopsy of Axilla Lymph Nodes
- Ductal carcinoma in situ diagnosed using an ultrasound-guided 14-gauge core needle biopsy of breast masses: can underestimation be predicted preoperatively?
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Solitary Axillary Lymph Node Metastasis without Breast Involvement from Ovarian Cancer: Case Report and Brief Literature Review