J Korean Diabetes.
2020 Dec;21(4):191-196. 10.4093/jkd.2020.21.4.191.
Adjustment of Insulin Therapy: New Insights from Continuous Glucose Monitoring
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2511884
- DOI: http://doi.org/10.4093/jkd.2020.21.4.191
Abstract
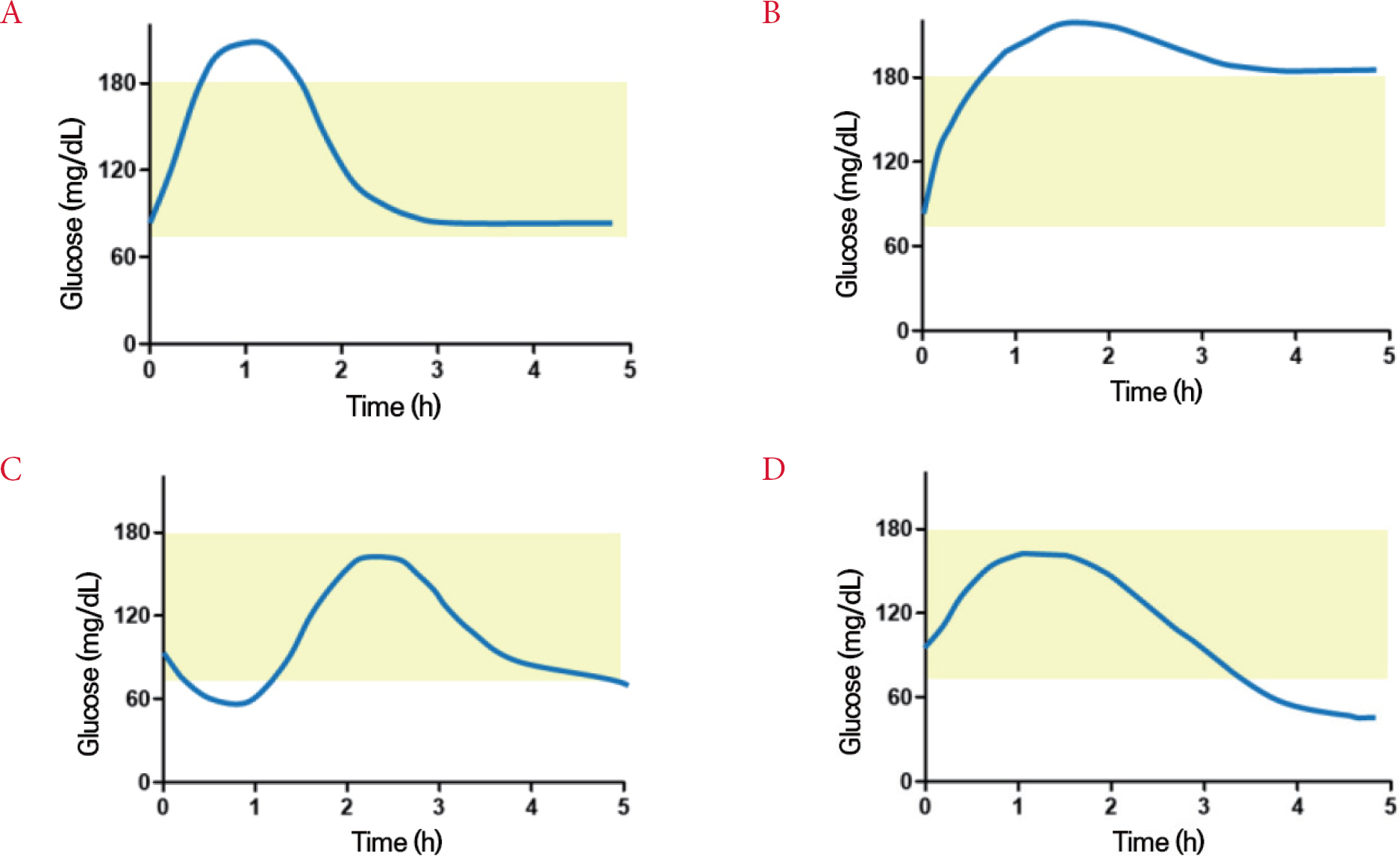
- Diabetes management technology has advanced dramatically in recent decades, particularly real time continuous glucose monitoring (rtCGM) systems. A recent meta-analysis showed that rtCGM can reduce HbA1c by around 0.3% compared to standard care, and prevent hypoglycemia. In the CGM era, new treatment targets such as time in range should be considered in conjunction with HbA1c. One study using rtCGM demonstrated an increase of time in range compared to conventional treatment. rtCGM presents current glucose concentration data, as well as the direction and rate of change in glucose level every 1 to 5 minutes. This information enables development of new insulin dosing algorithms. This fine-tuning of insulin therapy should be based on healthy eating behavior. Furthermore, as the patient is the center of diabetes management patient education is needed regarding how this new technology can improve glucose management. This manuscript summarizes the utility of rtCGM for insulin adjustment.
Keyword
Figure
Cited by 1 articles
-
Individualized Medical Nutrition Therapy for Diabetic Patients according to Diabetes Medication
Juyeon Park
J Korean Diabetes. 2022;23(1):50-56. doi: 10.4093/jkd.2022.23.1.50.
Reference
-
1. Beck RW., Bergenstal RM., Laffel LM., Pickup JC. Advances in technology for management of type 1 diabetes. Lancet. 2019. 394:1265–73.
Article2. Aleppo G., Ruedy KJ., Riddlesworth TD., Kruger DF., Peters AL., Hirsch I, et al. REPLACE-BG Study Group. REPLACE-BG: a randomized trial comparing continuous glucose monitoring with and without routine blood glucose monitoring in adults with well-controlled type 1 diabetes. Diabetes Care. 2017. 40:538–45.
Article3. Battelino T., Danne T., Bergenstal RM., Amiel SA., Beck R., Biester T, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019. 42:1593–603.4. Bergenstal RM., Beck RW., Close KL., Grunberger G., Sacks DB., Kowalski A, et al. Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes Care. 2018. 41:2275–80.
Article5. Beck RW., Bergenstal RM., Riddlesworth TD., Kollman C., Li Z., Brown AS, et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019. 42:400–5.
Article6. Maiorino MI., Signoriello S., Maio A., Chiodini P., Bellastella G., Scappaticcio L, et al. Effects of continuous glucose monitoring on metrics of glycemic control in diabetes: a systematic review with meta-analysis of randomized controlled trials. Diabetes Care. 2020. 43:1146–56.
Article7. Johnson ML., Martens TW., Criego AB., Carlson AL., Simonson GD., Bergenstal RM. Utilizing the ambulatory glucose profile to standardize and implement continuous glucose monitoring in clinical practice. Diabetes Technol Ther. 2019. 21(S2):S217–25.
Article8. Bell KJ., Barclay AW., Petocz P., Colagiuri S., Brand-Miller JC. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2014. 2:133–40.
Article9. Ajjan RA., Cummings MH., Jennings P., Leelarathna L., Rayman G., Wilmot EG. Optimising use of rate-of-change trend arrows for insulin dosing decisions using the FreeStyle Libre flash glucose monitoring system. Diab Vasc Dis Res. 2019. 16:3–12.
Article10. Nakamura T., Hirota Y., Hashimoto N., Matsuda T., Takabe M., Sakaguchi K, et al. Diurnal variation of carbohydrate insulin ratio in adult type 1 diabetic patients treated with continuous subcutaneous insulin infusion. J Diabetes Investig. 2014. 5:48–50.
Article11. Smart CE., Evans M., O’Connell SM., McElduff P., Lopez PE., Jones TW, et al. Both dietary protein and fat increase postprandial glucose excursions in children with type 1 diabetes, and the effect is additive. Diabetes Care. 2013. 36:3897–902.
Article12. Bell KJ., Smart CE., Steil GM., Brand-Miller JC., King B., Wolpert HA. Impact of fat, protein, and glycemic index on postprandial glucose control in type 1 diabetes: implications for intensive diabetes management in the continuous glucose monitoring era. Diabetes Care. 2015. 38:1008–15.
Article13. Kuroda A., Kaneto H., Yasuda T., Matsuhisa M., Miyashita K., Fujiki N, et al. Basal insulin requirement is ∼30% of the total daily insulin dose in type 1 diabetic patients who use the insulin pump. Diabetes Care. 2011. 34:1089–90.
Article14. Ostrovski I., Lovblom LE., Scarr D., Weisman A., Cardinez N., Orszag A, et al. Analysis of prevalence, magnitude and timing of the dawn phenomenon in adults and adolescents with type 1 diabetes: descriptive analysis of 2 insulin pump trials. Can J Diabetes. 2020. 44:229–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Glucose Management Using Continuous Glucose Monitors
- Application of Continuous Glucose Monitoring System (CGMS) and Patient Education
- Continuous Glucose Monitoring Sensors for Diabetes Management: A Review of Technologies and Applications
- 2023 Clinical Practice Guidelines for Diabetes: Continuous Glucose Monitoring and Insulin Pumps
- Transient Neonatal Diabetes Mellitus Managed with Continuous Subcutaneous Insulin Infusion (CSII) and Continuous Glucose Monitoring