Obstet Gynecol Sci.
2021 Jan;64(1):80-89. 10.5468/ogs.20186.
Impact of lymphadenectomy on the treatment of endometrial cancer using data from the JSOG cancer registry
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Keio University School of Medicine, Tokyo, Japan
- 2Department of Obstetrics and Gynecology, Tokai University School of Medicine, Kanagawa, Japan
- 3Department of Obstetrics and Gynecology, Sapporo City General Hospital, Sapporo, Japan
- 4Department of Obstetrics and Gynecology, Kyorin University School of Medicine, Tokyo, Japan
- 5Department of Obstetrics and Gynecology, Tokyo Women’s Medical University, Tokyo, Japan
- 6Department of Obstetrics and Gynecology, Otaru General Hospital, Sapporo, Japan
- 7Department of Obstetrics and Gynecology, Yamagata University, Yamagata, Japan
- 8Department of Obstetrics and Gynecology, Niigata University School of Medicine, Niigata, Japan
- KMID: 2511568
- DOI: http://doi.org/10.5468/ogs.20186
Abstract
Objective
Regional lymph node (LN) dissection is a standard surgical procedure for endometrial cancer, but there is currently no clear consensus on its therapeutic significance. We aimed to determine the impact of regional LN dissection on the outcome of endometrial cancer.
Methods
Study subjects comprised 36,813 patients who were registered in the gynecological tumor registry of the Japan Society of Obstetrics and Gynecology, had undergone initial surgery for endometrial cancer between 2004 and 2011, and whose clinicopathological factors and prognosis were appropriate for our investigation. The following clinicopathological factors were obtained from the registry: age, surgical stage classification, Union for International Cancer Control tumor, node, metastasis classification, histological type, histological differentiation, presence or absence of LN dissection, and postoperative treatment. We retrospectively analyzed the clinicopathological factors and therapeutic outcomes for patients with endometrial cancer.
Results
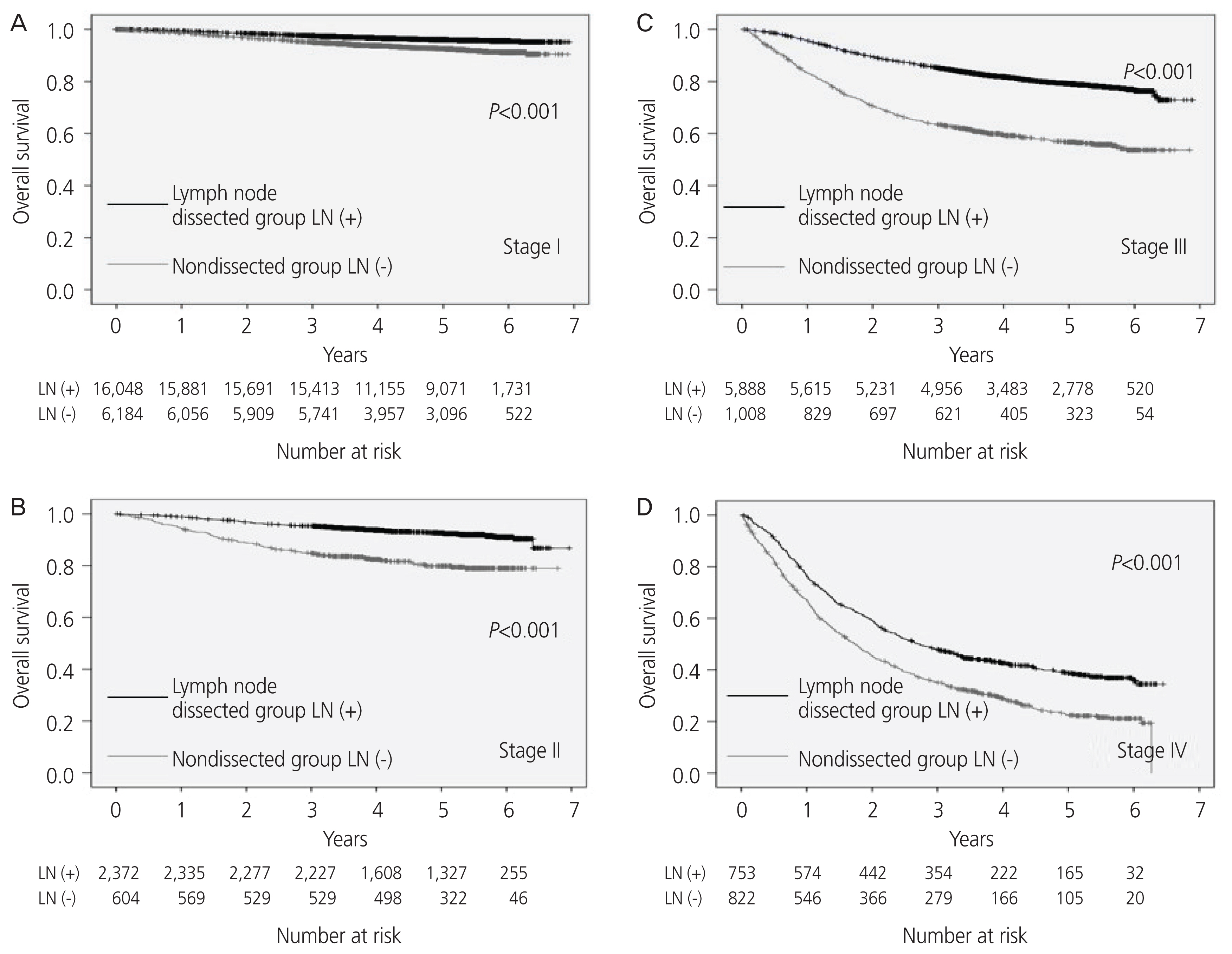
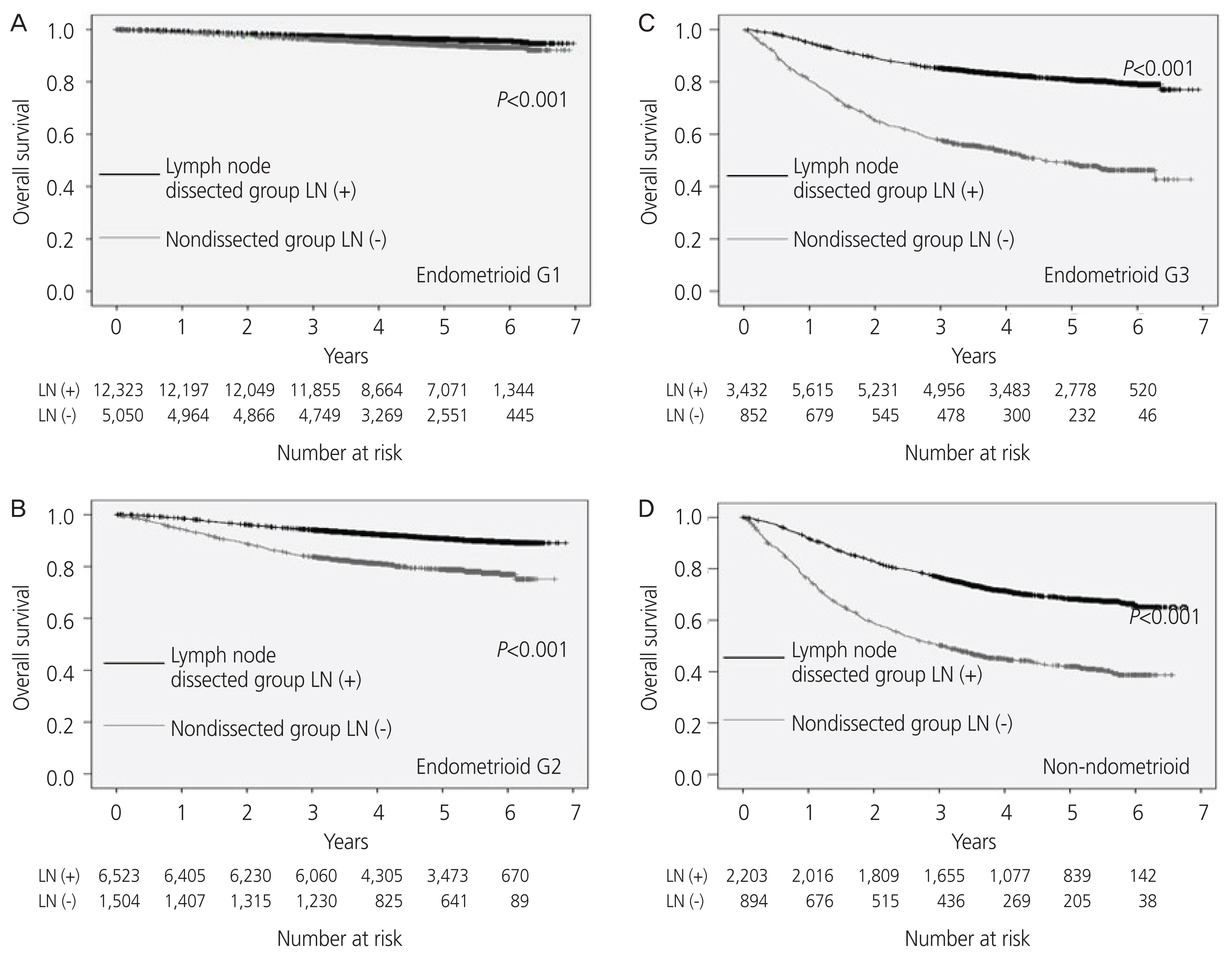
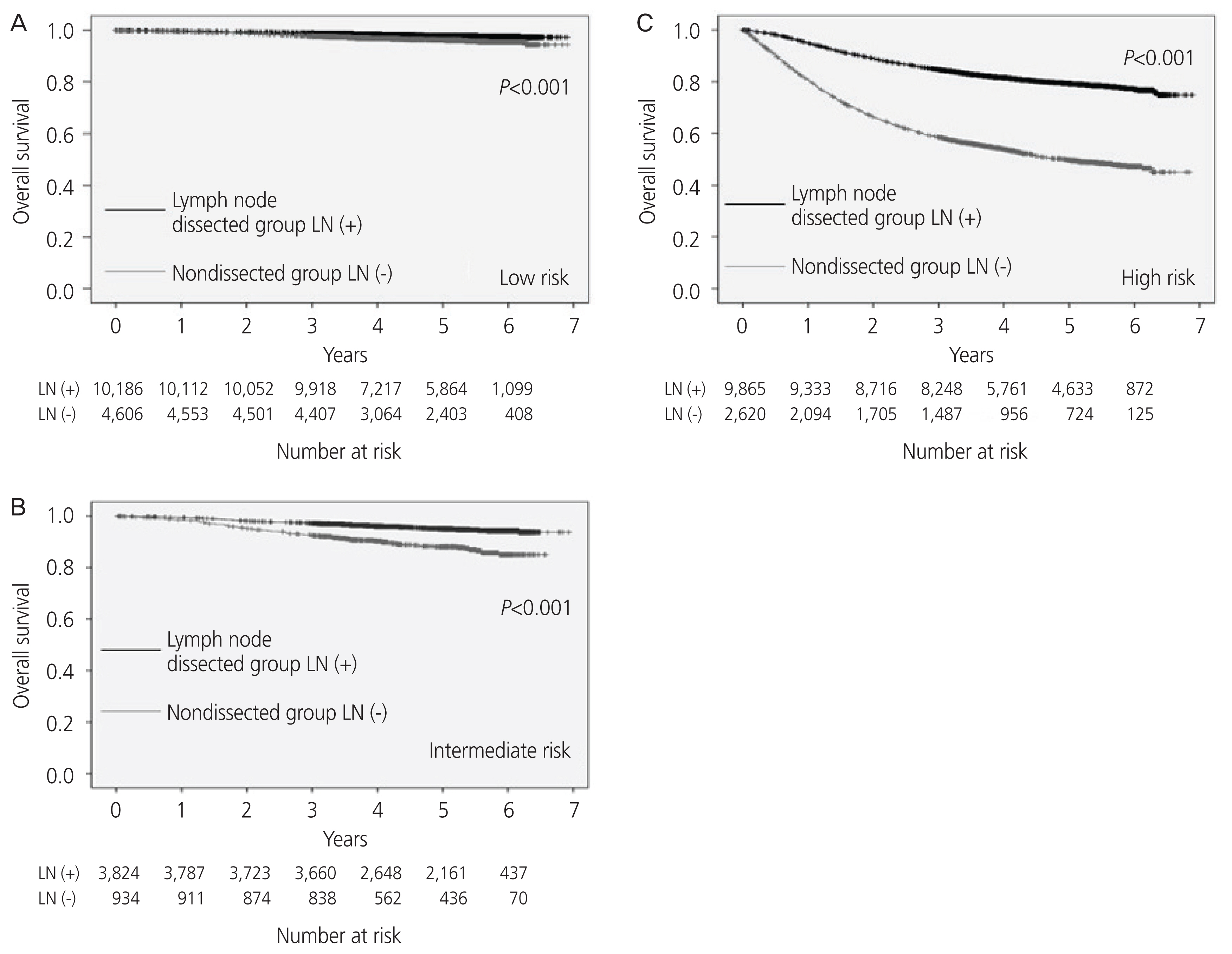
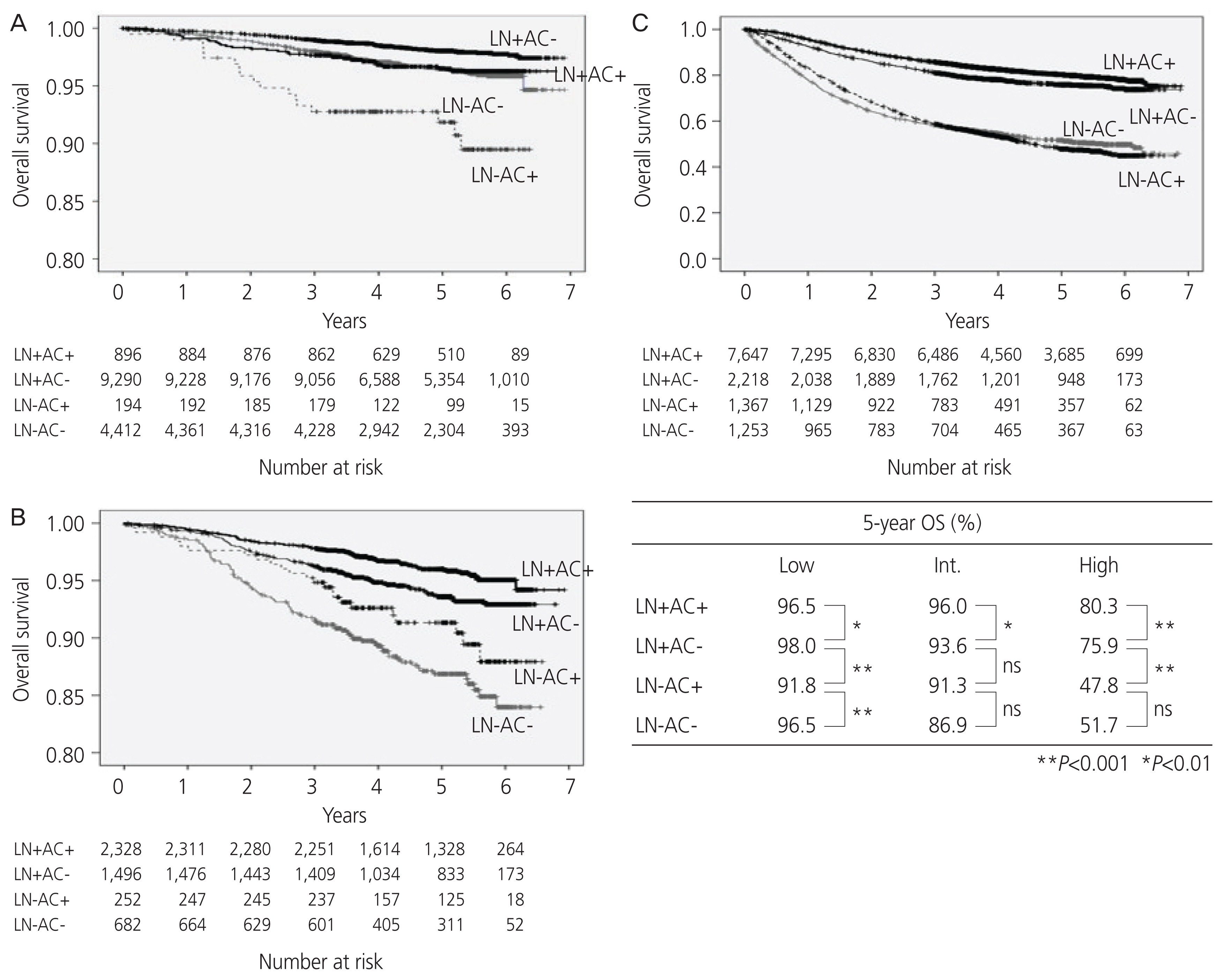
Analysis of all subjects showed that the group that underwent LN dissection had a significantly better overall survival than the group that did not undergo dissection. Analysis based on stage showed similar results across groups, except for stage Ia. Analysis based on stage and histological type showed similar results across groups, except for stage Ia endometrial carcinoma G1 or Ia G2. Multivariate analysis of prognostic factors indicated that LN dissection is an independent prognostic factor and that it has a greater impact on prognosis than adjuvant chemotherapy.
Conclusion
Despite the limitations of a retrospective study with some biases, the results suggest that LN dissection in endometrial cancer has a prognostic effect.
Figure
Cited by 2 articles
-
Sentinel lymph node biopsy in high-risk endometrial cancer: performance, outcomes, and future avenues
Yoo-Na Kim, Young Tae Kim
Obstet Gynecol Sci. 2022;65(5):395-405. doi: 10.5468/ogs.22146.A personalized nomogram for predicting 3-year overall survival of patients with uterine carcinosarcoma in a tertiary care hospital in Southern Thailand
Kulisara Nanthamongkolkul, Pacharadol Taweerat, Ingporn Jiamset
Obstet Gynecol Sci. 2023;66(3):198-207. doi: 10.5468/ogs.22262.
Reference
-
References
1. Yamagami W, Nagase S, Takahashi F, Ino K, Hachisuga T, Aoki D, et al. Clinical statistics of gynecologic cancers in Japan. J Gynecol Oncol. 2017; 28:e32.
Article2. Shigeta S, Nagase S, Mikami M, Ikeda M, Shida M, Sakaguchi I, et al. Assessing the effect of guideline introduction on clinical practice and outcome in patients with endometrial cancer in Japan: a project of the Japan Society of Gynecologic Oncology (JSGO) guideline evaluation committee. J Gynecol Oncol. 2017; 28:e76.
Article3. Nagase S, Ohta T, Takahashi F, Enomoto T. 2017 Committee on Gynecologic Oncology of the Japan Society of Obstetrics and Gynecology. Annual report of the committee on gynecologic oncology, the Japan Society of Obstetrics and Gynecology: annual patients report for 2015 and annual treatment report for 2010. J Obstet Gynaecol Res. 2019; 45:289–98.
Article4. Yamagami W, Mikami M, Nagase S, Tabata T, Kobayashi Y, Kaneuchi M, et al. Japan Society of Gynecologic Oncology 2018 guidelines for treatment of uterine body neoplasms. J Gynecol Oncol. 2020; 31:e18.
Article5. Trimble EL, Kosary C, Park RC. Lymph node sampling and survival in endometrial cancer. Gynecol Oncol. 1998; 71:340–3.
Article6. Chan JK, Cheung MK, Huh WK, Osann K, Husain A, Teng NN, et al. Therapeutic role of lymph node resection in endometrioid corpus cancer: a study of 12,333 patients. Cancer. 2006; 107:1823–30.7. Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. ASTEC study group. Efficacy of systematic pelvic lymph-adenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009; 373:125–36.8. Benedetti Panici P, Basile S, Maneschi F, Alberto Lissoni A, Signorelli M, Scambia G, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008; 100:1707–16.9. Todo Y, Kato H, Kaneuchi M, Watari H, Takeda M, Sakuragi N. Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL study): a retrospective cohort analysis. Lancet. 2010; 375:1165–72.
Article10. Watanabe Y, Kitagawa R, Aoki D, Takeuchi S, Sagae S, Sakuragi N, et al. Practice pattern for postoperative management of endometrial cancer in Japan: a survey of the Japanese Gynecologic Oncology Group. Gynecol Oncol. 2009; 115:456–9.
Article11. Ko EM, Funk MJ, Clark LH, Brewster WR. Did GOG99 and PORTEC1 change clinical practice in the United States? Gynecol Oncol. 2013; 129:12–7.
Article12. Press JZ, Gotlieb WH. Controversies in the treatment of early stage endometrial carcinoma. Obstet Gynecol Int. 2012; 2012:578490.
Article13. Matei D, Filiaci V, Randall ME, Mutch D, Steinhoff MM, DiSilvestro PA, et al. Adjuvant chemotherapy plus radiation for locally advanced endometrial cancer. N Engl J Med. 2019; 380:2317–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of lymphadenectomy in surgical staging of endometrial cancer
- The effect of lymphadenectomy on the survival rate of clinical stage I endometrial cancer
- Lymphadenectomy issues in endometrial cancer
- Contemporary trends of endometrial cancer in Korean women
- Emerging concept of tailored lymphadenectomy in endometrial cancer