Endocrinol Metab.
2020 Dec;35(4):811-819. 10.3803/EnM.2020.709.
Trends in the Diagnosis and Treatment of Patients with Medullary Thyroid Carcinoma in Korea
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 2Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- KMID: 2511008
- DOI: http://doi.org/10.3803/EnM.2020.709
Abstract
- Background
Thyroid cancer is becoming increasingly common worldwide, but little is known about the epidemiology of medullary thyroid carcinoma (MTC). This study investigated the current status of the incidence and treatment of MTC using Korean National Health Insurance Service (NHIS) data for the entire Korean population from 2004 to 2016.
Methods
This study included 1,790 MTC patients identified from the NHIS database.
Results
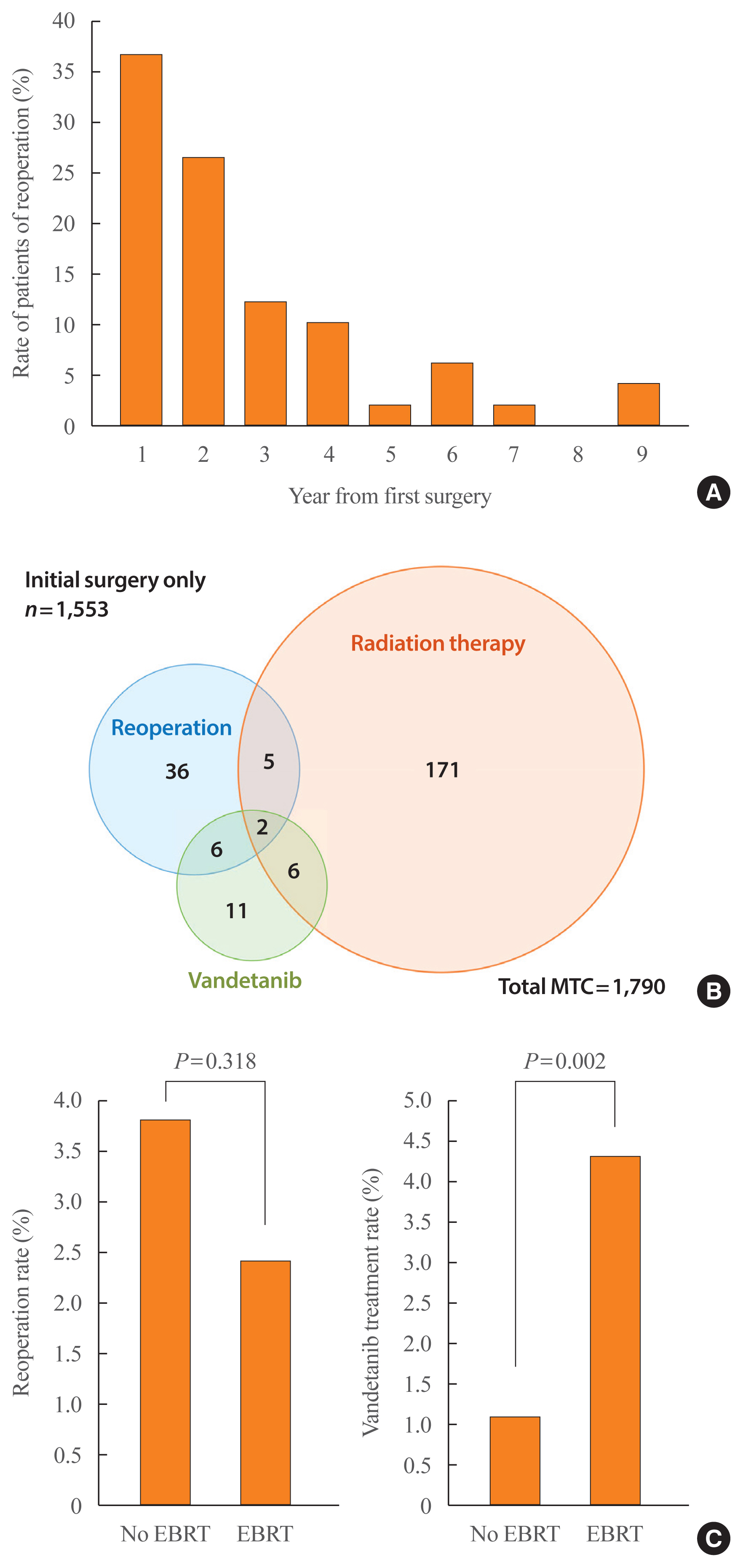
The age-standardized incidence rate showed a slightly decreasing or stationary trend during the period, from 0.25 per 100,000 persons in 2004 to 0.19 in 2016. The average proportion of MTC among all thyroid cancers was 0.5%. For initial surgical treatment, 65.4% of patients underwent total thyroidectomy. After surgery, external-beam radiation therapy (EBRT) was performed in 10% of patients, a proportion that increased from 6.7% in 2004 to 11.0% in 2016. Reoperations were performed in 2.7% of patients (n=49) at a median of 1.9 years of follow-up (interquartile range, 1.2 to 3.4). Since November 2015, 25 (1.4%) patients with MTC were prescribed vandetanib by December 2016.
Conclusion
The incidence of MTC decreased slightly with time, and the proportion of patients who underwent total thyroidectomy was about 65%. EBRT, reoperation, and tyrosine kinase inhibitor therapy are additional treatments after initial surgery for advanced MTC in Korea.
Keyword
Figure
Cited by 2 articles
-
A High Frequency of Lobectomy Instead of Total Thyroidectomy to Treat Medullary Thyroid Cancer in Korea: Data from the Korean National Health Insurance Service
Sun Wook Cho
Endocrinol Metab. 2020;35(4):784-785. doi: 10.3803/EnM.2020.408.Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinol Metab. 2023;38(1):10-24. doi: 10.3803/EnM.2023.102.
Reference
-
1. Kebebew E, Ituarte PH, Siperstein AE, Duh QY, Clark OH. Medullary thyroid carcinoma: clinical characteristics, treatment, prognostic factors, and a comparison of staging systems. Cancer. 2000; 88:1139–48.2. Faik Erdogan M, Gursoy A, Erdogan G, Kamel N. Radioactive iodine treatment in medullary thyroid carcinoma. Nucl Med Commun. 2006; 27:359–62.
Article3. Schwartz DL, Rana V, Shaw S, Yazbeck C, Ang KK, Morrison WH, et al. Postoperative radiotherapy for advanced medullary thyroid cancer: local disease control in the modern era. Head Neck. 2008; 30:883–8.
Article4. Wells SA Jr, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015; 25:567–610.
Article5. Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review 1975–2016, National Cancer Institute [Internet]. Bethesda: SEER;2019. [cited 2020 Oct 19]. Available from: https://seer.cancer.gov/csr/1975_2016/.6. Oh CM, Jung KW, Won YJ, Shin A, Kong HJ, Lee JS. Age-period-cohort analysis of thyroid cancer incidence in Korea. Cancer Res Treat. 2015; 47:362–9.
Article7. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA. 2017; 317:1338–48.
Article8. Sanabria A, Kowalski LP, Shah JP, Nixon IJ, Angelos P, Williams MD, et al. Growing incidence of thyroid carcinoma in recent years: factors underlying overdiagnosis. Head Neck. 2018; 40:855–66.
Article9. Park S, Oh CM, Cho H, Lee JY, Jung KW, Jun JK, et al. Association between screening and the thyroid cancer “epidemic” in South Korea: evidence from a nationwide study. BMJ. 2016; 355:i5745.
Article10. Randle RW, Balentine CJ, Leverson GE, Havlena JA, Sippel RS, Schneider DF, et al. Trends in the presentation, treatment, and survival of patients with medullary thyroid cancer over the past 30 years. Surgery. 2017; 161:137–46.
Article11. Ellison LF, Bushnik T. Changing trends in thyroid cancer incidence in Canada: a histologic examination, 1992 to 2016. Health Rep. 2020; 31:15–25.12. Opsahl EM, Akslen LA, Schlichting E, Aas T, Brauckhoff K, Hagen AI, et al. Trends in diagnostics, surgical treatment, and prognostic factors for outcomes in medullary thyroid carcinoma in Norway: a nationwide population-based study. Eur Thyroid J. 2019; 8:31–40.
Article13. Du L, Wang Y, Sun X, Li H, Geng X, Ge M, et al. Thyroid cancer: trends in incidence, mortality and clinical-pathological patterns in Zhejiang Province, Southeast China. BMC Cancer. 2018; 18:291.
Article14. National Cancer Registration and Analysis Service. Thyroid cancer: trends by sex, age and histological type [Internet]. London: National Cancer Intelligence Network;c2010. [cited 2020 Oct 19]. Available from: http://www.ncin.org.uk/publications/data_briefings/thyroid_cancer_trends_by_sex_age_and_histological_type.15. Rendl G, Manzl M, Hitzl W, Sungler P, Pirich C. Long-term prognosis of medullary thyroid carcinoma. Clin Endocrinol (Oxf). 2008; 69:497–505.
Article16. Roman S, Lin R, Sosa JA. Prognosis of medullary thyroid carcinoma: demographic, clinical, and pathologic predictors of survival in 1252 cases. Cancer. 2006; 107:2134–42.17. Choi YM, Kim TY, Jang EK, Kwon H, Jeon MJ, Kim WG, et al. Standardized thyroid cancer mortality in Korea between 1985 and 2010. Endocrinol Metab (Seoul). 2014; 29:530–5.
Article18. La Vecchia C, Malvezzi M, Bosetti C, Garavello W, Bertuccio P, Levi F, et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer. 2015; 136:2187–95.
Article19. Jung KY, Kim SM, Yoo WS, Kim BW, Lee YS, Kim KW, et al. Postoperative biochemical remission of serum calcitonin is the best predictive factor for recurrence-free survival of medullary thyroid cancer: a large-scale retrospective analysis over 30 years. Clin Endocrinol (Oxf). 2016; 84:587–97.
Article20. Kazaure HS, Roman SA, Sosa JA. Medullary thyroid microcarcinoma: a population-level analysis of 310 patients. Cancer. 2012; 118:620–7.21. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int J Epidemiol. 2017; 46:799–800.
Article22. World Health Organization. ICD-10 international statistical classification of diseases and related health problems: tenth revision. Gevena: World Health Organization;2004.23. Jung KY, Kim SM, Kim MJ, Cho SW, Kim BW, Lee YS, et al. Genotypic characteristics and their association with phenotypic characteristics of hereditary medullary thyroid carcinoma in Korea. Surgery. 2018; 164:312–8.
Article24. Kim BH. Registry for medullary thyroid carcinoma in Korea. In : 2015 Annual Symposium on Science, Technology, and Education & Autumn Symposium of KES; 2015 Oct 29–31; Busan, KR.25. Jameson JL. Harrison’s principles of internal medicine. 20th ed. New York: McGraw Hill;2018.26. KOrean Statistical Information Service. Population statistics based on resident registration [Internet]. Daejeon: KOSIS;2020. [cited 2020 Oct 19]. Available from: http://kosis.kr/index/index.do .27. Korea Central Cancer Registry, National Cancer Center. Annual report of cancer statistics in Korea in 2016 [Internet]. Sejong: Ministry of Health and Welfare;2018. [cited 2020 Oct 19]. Available from: https://ncc.re.kr/main.ncc?uri=english/sub04_statistics.28. Mathiesen JS, Kroustrup JP, Vestergaard P, Stochholm K, Poulsen PL, Rasmussen AK, et al. Incidence and prevalence of sporadic and hereditary MTC in Denmark 1960–2014: a nationwide study. Endocr Connect. 2018; 7:829–39.
Article29. Modigliani E, Cohen R, Campos JM, Conte-Devolx B, Maes B, Boneu A, et al. Prognostic factors for survival and for biochemical cure in medullary thyroid carcinoma: results in 899 patients. The GETC Study Group. Groupe d’étude des tumeurs à calcitonine. Clin Endocrinol (Oxf). 1998; 48:265–73.30. Kim JH, Pyo JS, Cho WJ. Clinicopathological significance and prognosis of medullary thyroid microcarcinoma: a meta-analysis. World J Surg. 2017; 41:2551–8.
Article31. Hirsch D, Twito O, Levy S, Bachar G, Robenshtok E, Gross DJ, et al. Temporal trends in the presentation, treatment, and outcome of medullary thyroid carcinoma: an Israeli multicenter study. Thyroid. 2018; 28:369–76.
Article32. Cho BY, Choi HS, Park YJ, Lim JA, Ahn HY, Lee EK, et al. Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid. 2013; 23:797–804.
Article33. Choi JB, Lee SG, Kim MJ, Kim TH, Ban EJ, Lee CR, et al. Dynamic risk stratification in medullary thyroid carcinoma: single institution experiences. Medicine (Baltimore). 2018; 97:e9686.34. Meijer JA, Bakker LE, Valk GD, de Herder WW, de Wilt JH, Netea-Maier RT, et al. Radioactive iodine in the treatment of medullary thyroid carcinoma: a controlled multicenter study. Eur J Endocrinol. 2013; 168:779–86.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- Medullary and Papillary Thyroid Carcinoma as a Collision Tumor: Report of Five Cases
- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma
- A Case of Familial Medullary Thyroid Carcinoma