Neonatal Med.
2020 Nov;27(4):181-186. 10.5385/nm.2020.27.4.181.
Early Onset Type 2 Diabetes Mellitus in Non-Obese Adolescents Born Small for Gestational Age
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2510823
- DOI: http://doi.org/10.5385/nm.2020.27.4.181
Abstract
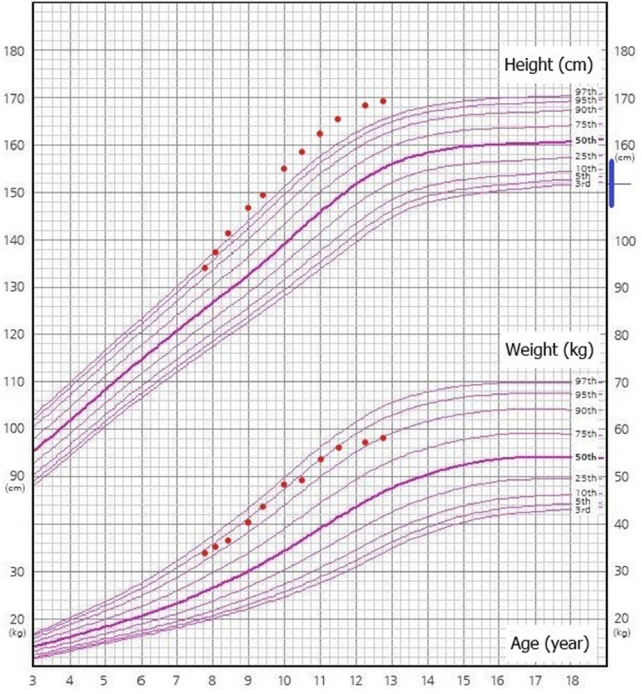
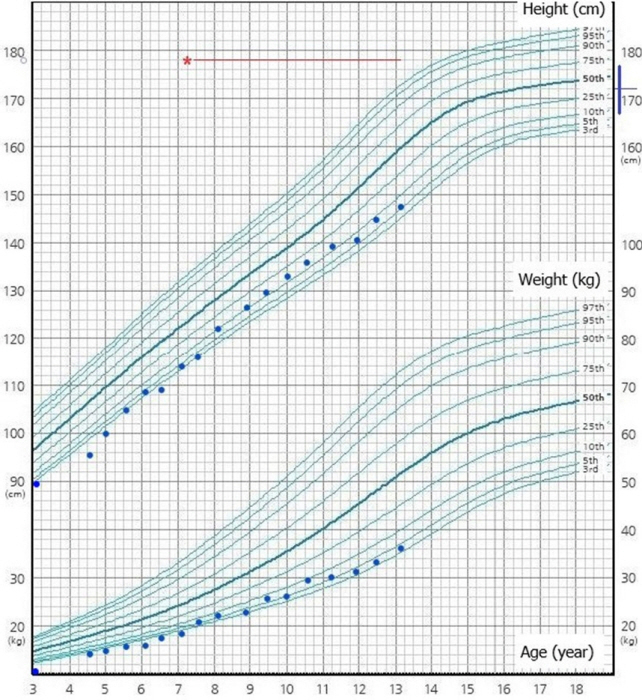
- Being born small for gestational age (SGA) has been strongly associated with mortality during the perinatal period and long-term risk of metabolic syndrome, including type 2 diabetes mellitus, hypertension, hyperlipidemia, and coronary heart disease. Insulin resistance is an important factor in the development of metabolic syndrome in SGA, with several proposed hypotheses. Here, we report two cases of non-obese adolescent patients with early onset type 2 diabetes who were born SGA. Of these, one experienced catch-up growth, while the other did not. Both had a high body fat percentage at the time of diagnosis of type 2 diabetes and were diagnosed with fatty liver and hyperlipidemia before adolescence, at the age of 7 years. Early interventions for SGA are needed for healthy catch-up growth to prevent metabolic diseases in the future.
Keyword
Figure
Reference
-
1. Health Insurance Review and Assessment Service. Insurance Accreditation Standards [Internet]. Wonju: Health Insurance Review and Assessment Service;2019. [cited 2020 Oct 31]. Available from: https://www.hira.or.kr/main.do.2. Hediger ML, Overpeck MD, Kuczmarski RJ, McGlynn A, Maurer KR, Davis WW. Muscularity and fatness of infants and young children born small- or large-for-gestational-age. Pediatrics. 1998; 102:E60.3. Cho WK, Jung IA, Suh BK. Current growth status and metabolic parameters of Korean adolescents born small for gestational age: results from the Korea National Health and Nutrition Examination Surveys (KNHANES) 2010-2011. Pediatr Int. 2014; 56:344–8.4. Kim HE, Song IG, Chung SH, Choi YS, Bae CW. Trends in birth weight and the incidence of low birth weight and advanced maternal age in Korea between 1993 and 2016. J Korean Med Sci. 2019; 34:e34.5. Jaquet D, Deghmoun S, Chevenne D, Collin D, Czernichow P, Levy-Marchal C. Dynamic change in adiposity from fetal to postnatal life is involved in the metabolic syndrome associated with reduced fetal growth. Diabetologia. 2005; 48:849–55.6. Hales CN, Barker DJ. Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia. 1992; 35:595–601.7. Neel JV. Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet. 1962; 14:353–62.8. Hwang IT. Long-term care, from neonatal period to adulthood, of children born small for gestational age. Clin Pediatr Endocrinol. 2019; 28:97–103.9. Jensen ET, Dabelea D. Type 2 diabetes in youth: new lessons from the SEARCH study. Curr Diab Rep. 2018; 18:36.10. Barker DJ, Winter PD, Osmond C, Margetts B, Simmonds SJ. Weight in infancy and death from ischaemic heart disease. Lancet. 1989; 2:577–80.11. Soto N, Bazaes RA, Pena V, Salazar T, Avila A, Iniguez G, et al. Insulin sensitivity and secretion are related to catch-up growth in small-for-gestational-age infants at age 1 year: results from a prospective cohort. J Clin Endocrinol Metab. 2003; 88:3645–50.12. Giapros V, Vavva E, Siomou E, Kolios G, Tsabouri S, Cholevas V, et al. Low-birth-weight, but not catch-up growth, correlates with insulin resistance and resistin level in SGA infants at 12 months. J Matern Fetal Neonatal Med. 2017; 30:1771–6.13. Huang YT, Lin HY, Wang CH, Su BH, Lin CC. Association of preterm birth and small for gestational age with metabolic outcomes in children and adolescents: a population-based cohort study from Taiwan. Pediatr Neonatol. 2018; 59:147–53.14. Urakami T, Kuwabara R, Habu M, Okuno M, Suzuki J, Takahashi S, et al. Clinical characteristics of non-obese children with type 2 diabetes mellitus without involvement of β-cell autoimmunity. Diabetes Res Clin Pract. 2013; 99:105–11.15. Liu C, Wu B, Lin N, Fang X. Insulin resistance and its association with catch-up growth in Chinese children born small for gestational age. Obesity (Silver Spring). 2017; 25:172–7.16. Xu T, Liu J, Liu J, Zhu G, Han S. Relation between metabolic syndrome and body compositions among Chinese adolescents and adults from a large-scale population survey. BMC Public Health. 2017; 17:337.17. Sas T, Mulder P, Hokken-Koelega A. Body composition, blood pressure, and lipid metabolism before and during long-term growth hormone (GH) treatment in children with short stature born small for gestational age either with or without GH deficiency. J Clin Endocrinol Metab. 2000; 85:3786–92.18. De Zegher F, Sebastiani G, Diaz M, Gomez-Roig MD, Lopez-Bermejo A, Ibanez L. Breast-feeding vs formula-feeding for infants born small-for-gestational-age: divergent effects on fat mass and on circulating IGF-I and high-molecular-weight adiponectin in late infancy. J Clin Endocrinol Metab. 2013; 98:1242–7.19. Lei X, Chen Y, Ye J, Ouyang F, Jiang F, Zhang J. The optimal postnatal growth trajectory for term small for gestational age babies: a prospective cohort study. J Pediatr. 2015; 166:54–8.20. Kesavan K, Devaskar SU. Intrauterine growth restriction: postnatal monitoring and outcomes. Pediatr Clin North Am. 2019; 66:403–23.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Type 2 Diabetes Mellitus in Adolescents and Young Adults
- Clinical Course of Childhood and Adolescence Onset Type 2 Diabetes Mellitus
- Recent advances in gestational diabetes mellitus
- Clinical Predictive Factors for Metabolic Syndrome in Obese Children and Adolescents
- Pharmacothearpy of Adolescents with Diabetes