Ann Rehabil Med.
2020 Dec;44(6):415-427. 10.5535/arm.20071.
Novel Method of Classification in Knee Osteoarthritis: Machine Learning Application Versus Logistic Regression Model
- Affiliations
-
- 1Department of Rehabilitation Medicine, Hanyang University College of Medicine, Seoul, Korea
- 2Department of Rehabilitation Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 3Korea Orthopedics & Rehabilitation Engineering Center, Incheon, Korea
- KMID: 2510809
- DOI: http://doi.org/10.5535/arm.20071
Abstract
Objective
To present new classification methods of knee osteoarthritis (KOA) using machine learning and compare its performance with conventional statistical methods as classification techniques using machine learning have recently been developed.
Methods
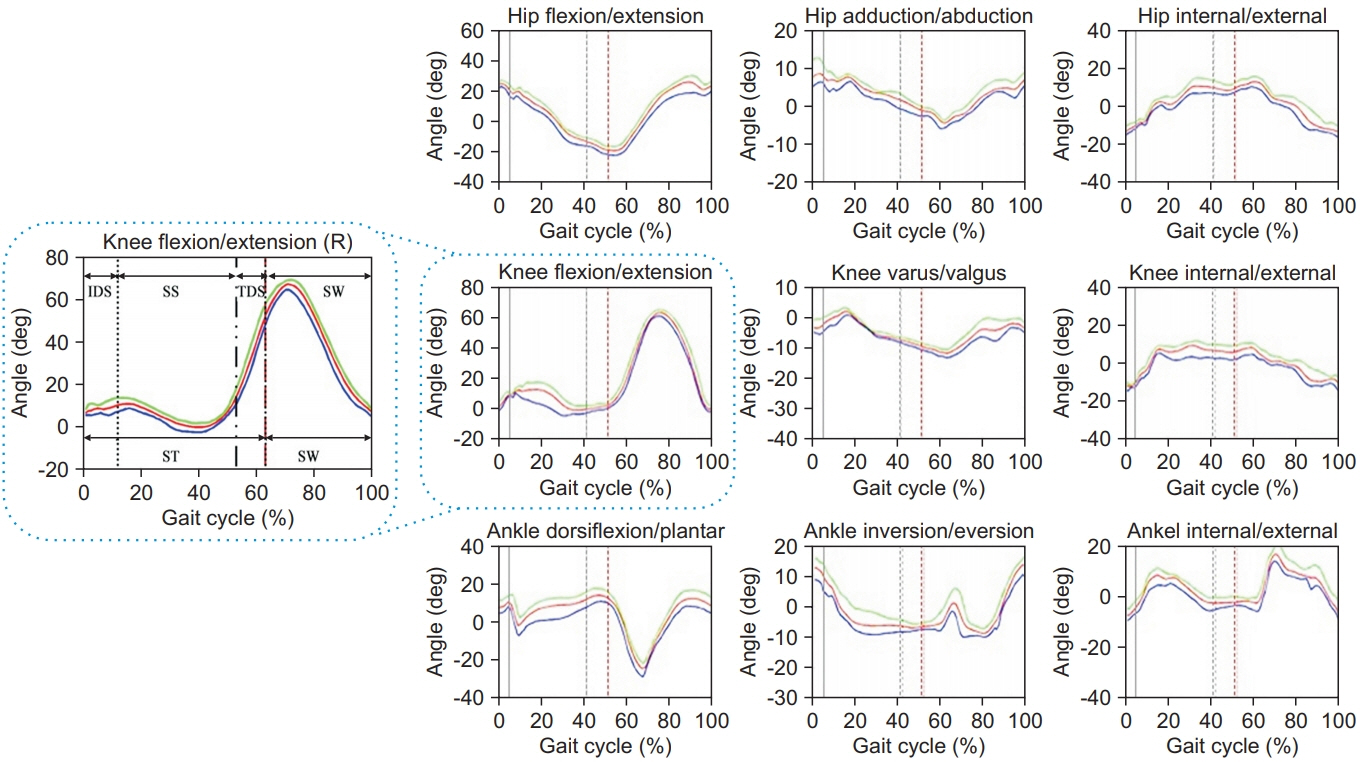
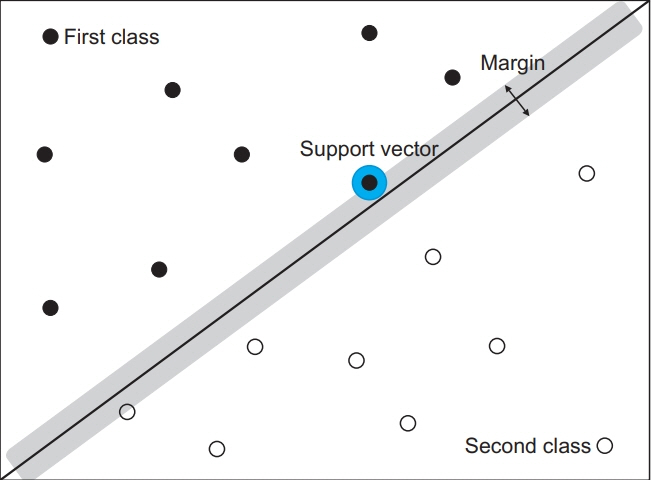
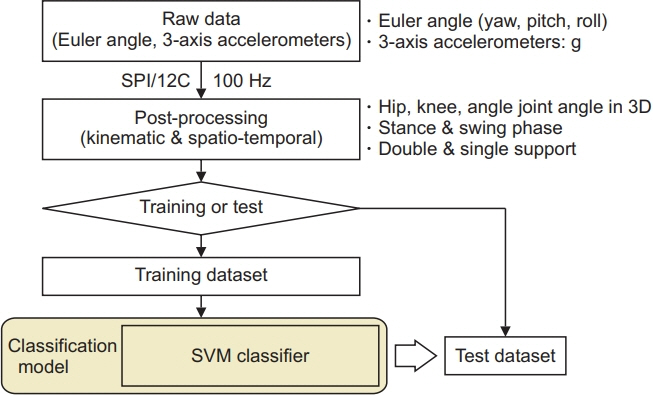
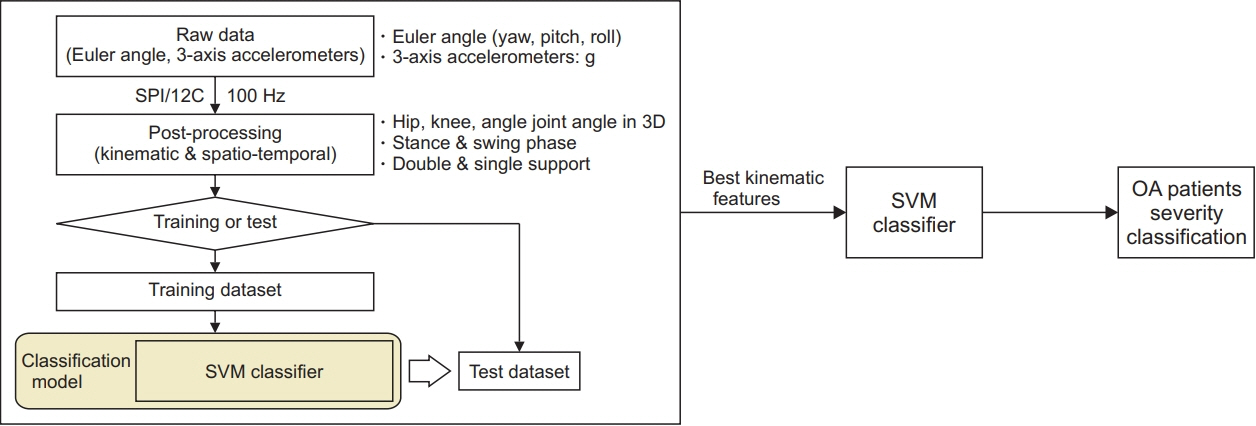
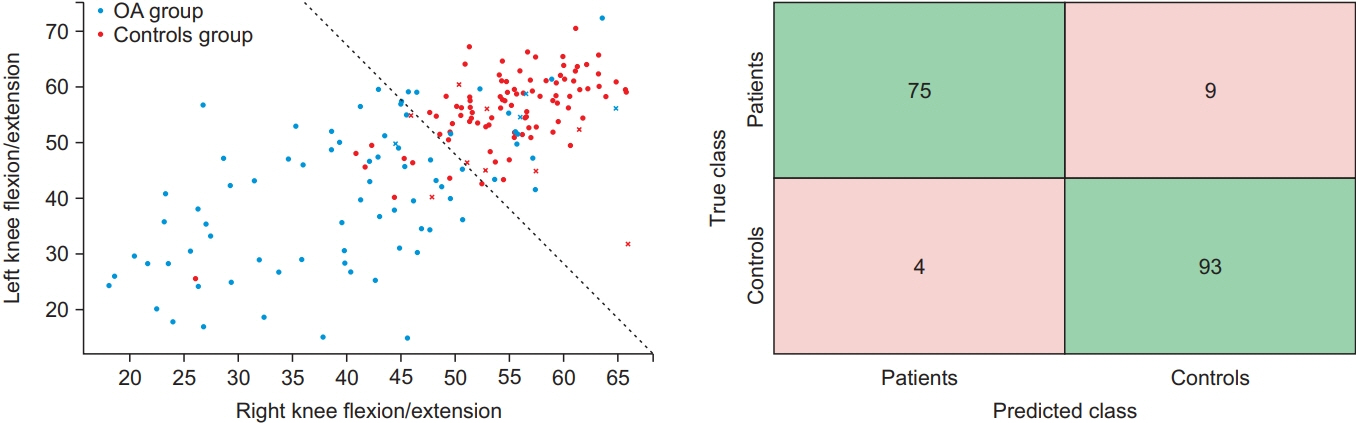
A total of 84 KOA patients and 97 normal participants were recruited. KOA patients were clustered into three groups according to the Kellgren-Lawrence (K-L) grading system. All subjects completed gait trials under the same experimental conditions. Machine learning-based classification using the support vector machine (SVM) classifier was performed to classify KOA patients and the severity of KOA. Logistic regression analysis was also performed to compare the results in classifying KOA patients with machine learning method.
Results
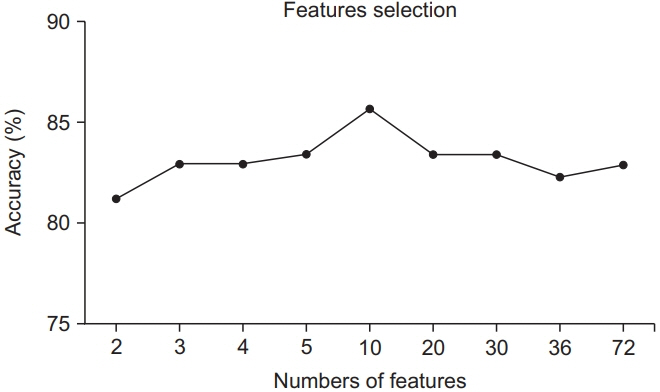
In the classification between KOA patients and normal subjects, the accuracy of classification was higher in machine learning method than in logistic regression analysis. In the classification of KOA severity, accuracy was enhanced through the feature selection process in the machine learning method. The most significant gait feature for classification was flexion and extension of the knee in the swing phase in the machine learning method.
Conclusion
The machine learning method is thought to be a new approach to complement conventional logistic regression analysis in the classification of KOA patients. It can be clinically used for diagnosis and gait correction of KOA patients.
Figure
Reference
-
1. Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006; 20:3–25.
Article2. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019; 393:1745–59.
Article3. Wallace IJ, Worthington S, Felson DT, Jurmain RD, Wren KT, Maijanen H, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A. 2017; 114:9332–6.
Article4. Samuel AJ, Kanimozhi D. Outcome measures used in patient with knee osteoarthritis: with special importance on functional outcome measures. Int J Health Sci (Qassim). 2019; 13:52–60.5. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016; 474:1886–93.
Article6. Deluzio KJ, Astephen JL. Biomechanical features of gait waveform data associated with knee osteoarthritis: an application of principal component analysis. Gait Posture. 2007; 25:86–93.7. Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res. 2008; 26:332–41.
Article8. Zeni JA Jr, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clin Biomech (Bristol, Avon). 2009; 24:372–8.9. Favre J, Jolles BM. Gait analysis of patients with knee osteoarthritis highlights a pathological mechanical pathway and provides a basis for therapeutic interventions. EFORT Open Rev. 2017; 1:368–74.
Article10. Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005; 52:2835–44.
Article11. Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001; 34:907–15.
Article12. Al-Zahrani KS, Bakheit AM. A study of the gait characteristics of patients with chronic osteoarthritis of the knee. Disabil Rehabil. 2002; 24:275–80.
Article13. Lewek MD, Scholz J, Rudolph KS, Snyder-Mackler L. Stride-to-stride variability of knee motion in patients with knee osteoarthritis. Gait Posture. 2006; 23:505–11.
Article14. Astephen Wilson JL, Deluzio KJ, Dunbar MJ, Caldwell GE, Hubley-Kozey CL. The association between knee joint biomechanics and neuromuscular control and moderate knee osteoarthritis radiographic and pain severity. Osteoarthritis Cartilage. 2011; 19:186–93.
Article15. Elbaz A, Mor A, Segal G, Debi R, Shazar N, Herman A. Novel classification of knee osteoarthritis severity based on spatiotemporal gait analysis. Osteoarthritis Cartilage. 2014; 22:457–63.
Article16. Cho JS, Cho YS, Moon SB, Kim MJ, Lee HD, Lee SY, et al. Scoliosis screening through a machine learning based gait analysis test. Int J Precis Eng Manuf. 2018; 19:1861–72.
Article17. Shetty S, Rao YS. SVM based machine learning approach to identify Parkinson’s disease using gait analysis. In : Proceedings of 2016 International Conference on Inventive Computation Technologies (ICICT); 2016 Aug 26-27; Coimbatore, India.
Article18. Mezghani N, Husse S, Boivin K, Turcot K, Aissaoui R, Hagemeister N, et al. Automatic classification of asymptomatic and osteoarthritis knee gait patterns using kinematic data features and the nearest neighbor classifier. IEEE Trans Biomed Eng. 2008; 55:1230–2.
Article19. Burges CJ. A tutorial on support vector machines for pattern recognition. Data Min Knowl Discov. 1998; 2:121–67.20. Aminian K, Najafi B, Bula C, Leyvraz PF, Robert P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J Biomech. 2002; 35:689–99.
Article21. Cho YS, Jang SH, Cho JS, Kim MJ, Lee HD, Lee SY, et al. Evaluation of validity and reliability of inertial measurement unit-based gait analysis systems. Ann Rehabil Med. 2018; 42:872–83.
Article22. Allseits E, Lucarevic J, Gailey R, Agrawal V, Gaunaurd I, Bennett C. The development and concurrent validity of a real-time algorithm for temporal gait analysis using inertial measurement units. J Biomech. 2017; 55:27–33.
Article23. Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee osteoarthritis: a primer. Perm J. 2017; 21:16–183.
Article24. Pritzker KP, Gay S, Jimenez SA, Ostergaard K, Pelletier JP, Revell PA, et al. Osteoarthritis cartilage histopathology: grading and staging. Osteoarthritis Cartilage. 2006; 14:13–29.
Article25. Spector TD, Cooper C. Radiographic assessment of osteoarthritis in population studies: whither Kellgren and Lawrence? Osteoarthritis Cartilage. 1993; 1:203–6.
Article26. Schiphof D, Boers M, Bierma-Zeinstra SM. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis. 2008; 67:1034–6.
Article27. Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002; 10:573–9.
Article28. McKean KA, Landry SC, Hubley-Kozey CL, Dunbar MJ, Stanish WD, Deluzio KJ. Gender differences exist in osteoarthritic gait. Clin Biomech (Bristol, Avon). 2007; 22:400–9.
Article29. Kiss RM. Effect of severity of knee osteoarthritis on the variability of gait parameters. J Electromyogr Kinesiol. 2011; 21:695–703.
Article30. Mills K, Hunt MA, Ferber R. Biomechanical deviations during level walking associated with knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2013; 65:1643–65.
Article31. Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ, Hubley-Kozey CL. Gait and neuromuscular pattern changes are associated with differences in knee osteoarthritis severity levels. J Biomech. 2008; 41:868–76.
Article32. Chang A, Hayes K, Dunlop D, Song J, Hurwitz D, Cahue S, et al. Hip abduction moment and protection against medial tibiofemoral osteoarthritis progression. Arthritis Rheum. 2005; 52:3515–9.
Article33. Messier SP, Loeser RF, Hoover JL, Semble EL, Wise CM. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992; 73:29–36.34. McCarthy I, Hodgins D, Mor A, Elbaz A, Segal G. Analysis of knee flexion characteristics and how they alter with the onset of knee osteoarthritis: a case control study. BMC Musculoskelet Disord. 2013; 14:169.
Article35. Simon SR. Quantification of human motion: gait analysis-benefits and limitations to its application to clinical problems. J Biomech. 2004; 37:1869–80.
Article36. Ahmed H, Tahir M. Improving the accuracy of human body orientation estimation with wearable IMU sensors. IEEE Trans Instrum Meas. 2017; 66:535–42.
Article37. Beange KH, Chan AD, Graham RB. Evaluation of wearable IMU performance for orientation estimation and motion tracking. In : Proceedings of 2018 IEEE International Symposium on Medical Measurements and Applications (MeMeA); 2018 Jun 11-13; Rome, Italy.
Article38. Obermeyer Z, Emanuel EJ. Predicting the future: big data, machine learning, and clinical medicine. N Engl J Med. 2016; 375:1216–9.39. Chan K, Lee TW, Sample PA, Goldbaum MH, Weinreb RN, Sejnowski TJ. Comparison of machine learning and traditional classifiers in glaucoma diagnosis. IEEE Trans Biomed Eng. 2002; 49:963–74.40. Marriott KA, Birmingham TB, Leitch KM, Pinto R, Giffin JR. Strong independent associations between gait biomechanics and pain in patients with knee osteoarthritis. J Biomech. 2019; 94:123–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Machine Learning vs. Statistical Model for Prediction Modelling: Application in Medical Imaging Research
- Identification of Mesiodens Using Machine Learning Application in Panoramic Images
- Application of Text-Classification Based Machine Learningin Predicting Psychiatric Diagnosis
- The application of machine learning for predicting recurrence in patients with early-stage endometrial cancer: a pilot study
- Use of Machine Learning in Stroke Rehabilitation: A Narrative Review