Cancer Res Treat.
2021 Jan;53(1):283-288. 10.4143/crt.2020.575.
Hyperammonemic Encephalopathy Mimicking Ornithine Transcarbamylase Deficiency in Fibrolamellar Hepatocellular Carcinoma: Successful Treatment with Continuous Venovenous Hemofiltration and Ammonia Scavengers
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Center for Pediatric Cancer, National Cancer Center, Goyang, Korea
- 3Department of Surgery, National Cancer Center, Goyang, Korea
- 4Department of Pathology, National Cancer Center, Goyang, Korea
- KMID: 2510671
- DOI: http://doi.org/10.4143/crt.2020.575
Abstract
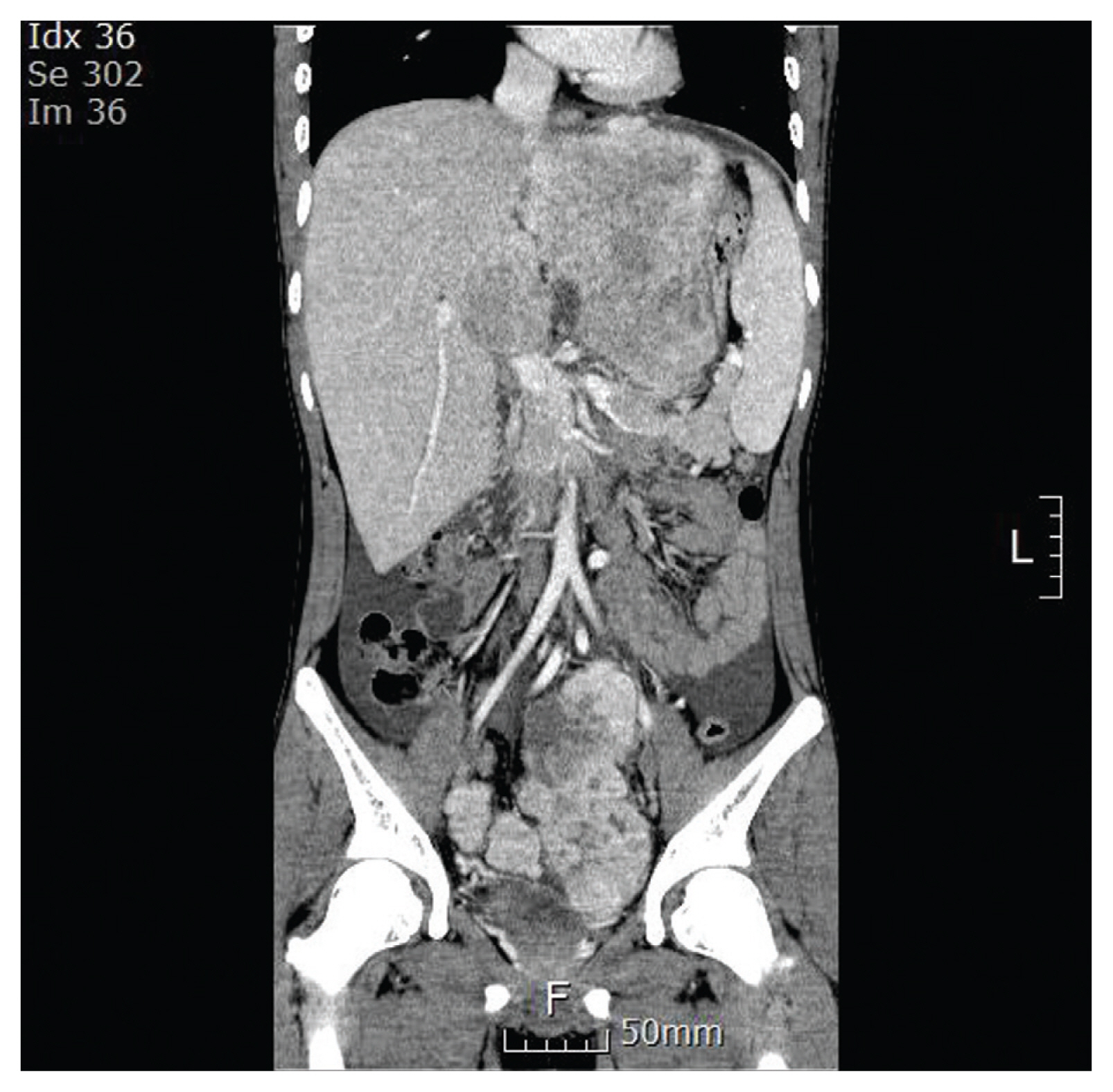
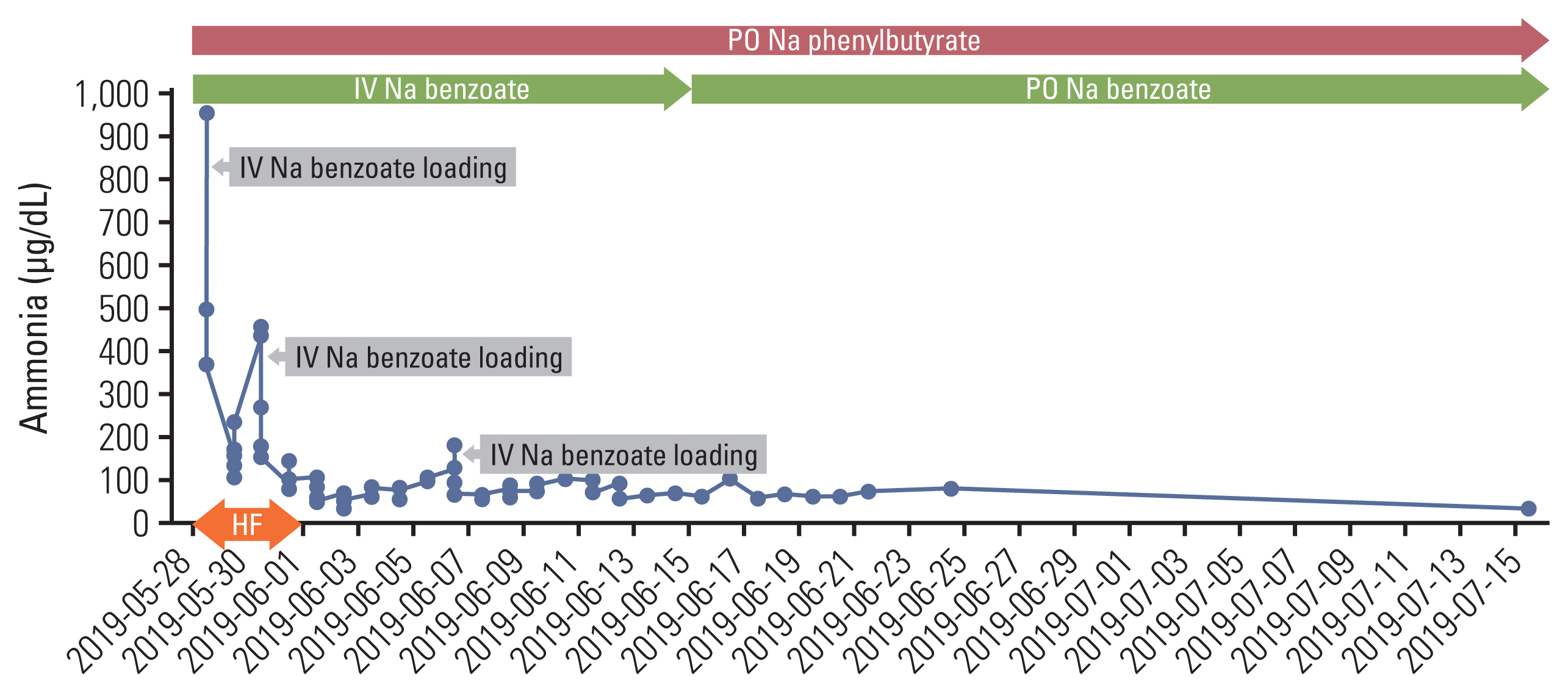
- Fibrolamellar hepatocellular carcinoma (FLHCC) is a rare liver cancer affecting adolescents and young adults without any pre existing liver disease. Hyperammonemic encephalopathy (HAE) is a serious paraneoplastic syndrome, and several cases of HAE have been reported in patients with FLHCC. This condition is rare; hence, there are currently no management guidelines for cancer-related HAE. Herein, we report a case of an 18-year-old man with advanced FLHCC who developed HAE during the first course of chemotherapy consisting of cisplatin, doxorubicin, 5-fluorouracil, and interferon-α. He was successfully treated with continuous venovenous hemofiltration, sodium benzoate, sodium phenylbutyrate, and amino acid supplementation for HAE. After the second course of chemotherapy, he underwent surgery, and thereafter, his ammonia levels were normal without any ammonia scavenger therapy. Treatments for HAE described here will be helpful for this rare, but serious metabolic complication of FLHCC and could partially applied to HAE related to any malignancies.
Figure
Reference
-
References
1. Chakrabarti S, Tella SH, Kommalapati A, Huffman BM, Yadav S, Riaz IB, et al. Clinicopathological features and outcomes of fibrolamellar hepatocellular carcinoma. J Gastrointest Oncol. 2019; 10:554–61.
Article2. Riggle KM, Turnham R, Scott JD, Yeung RS, Riehle KJ. Fibrolamellar hepatocellular carcinoma: mechanistic distinction from adult hepatocellular carcinoma. Pediatr Blood Cancer. 2016; 63:1163–7.
Article3. Sethi S, Tageja N, Singh J, Arabi H, Dave M, Badheka A, et al. Hyperammonemic encephalopathy: a rare presentation of fibrolamellar hepatocellular carcinoma. Am J Med Sci. 2009; 338:522–4.
Article4. Alsina AE, Franco E, Nakshabandi A, Albers C, Kemmer N, Berry AC, et al. Successful liver transplantation for hyperammonemic fibrolamellar hepatocellular carcinoma. ACG Case Rep J. 2016; 3:e106.
Article5. Cho J, Chen JCY, Paludo J, Conboy EE, Lanpher BC, Alberts SR, et al. Hyperammonemic encephalopathy in a patient with fibrolamellar hepatocellular carcinoma: case report and literature review. J Gastrointest Oncol. 2019; 10:582–8.
Article6. Surjan RC, Dos Santos ES, Basseres T, Makdissi FF, Machado MA. A proposed physiopathological pathway to hyperammonemic encephalopathy in a non-cirrhotic patient with fibrolamellar hepatocellular carcinoma without ornithine transcarbamylase (OTC) Mutation. Am J Case Rep. 2017; 18:234–41.
Article7. Muramori K, Taguchi S, Taguchi T, Kohashi K, Furuya K, Tokuda K, et al. High aromatase activity and overexpression of epidermal growth factor receptor in fibrolamellar hepatocellular carcinoma in a child. J Pediatr Hematol Oncol. 2011; 33:e195–7.
Article8. Bhagat M, Kembhavi S, Qureshi SS. Fibrolamellar hepatocellular carcinoma with extensive vascular thrombosis. J Cancer Res Ther. 2015; 11:493–4.9. Weber G, Queener SF, Morris HP. Imbalance in ornithine metabolism in hepatomas of different growth rates as expressed in behavior of L-ornithine carbamyl transferase activity. Cancer Res. 1972; 32:1933–40.10. __Honeyman JN, Simon EP, Robine N, Chiaroni-Clarke R, Darcy DG, Lim II, et al. Detection of a recurrent DNAJB1-PRKACA chimeric transcript in fibrolamellar hepatocellular carcinoma. Science. 2014; 343:1010–4.11. Hawley RJ. Hyperammonia possibly due to corticosteroids. Arch Neurol. 2000; 57:1085–6.
Article12. Nussbaum V, Lubcke N, Findlay R. Hyperammonemia secondary to asparaginase: a case series. J Oncol Pharm Pract. 2016; 22:161–4.
Article13. Fultz KE, Gerner EW. APC-dependent regulation of ornithine decarboxylase in human colon tumor cells. Mol Carcinog. 2002; 34:10–8.
Article14. Matoori S, Leroux JC. Recent advances in the treatment of hyperammonemia. Adv Drug Deliv Rev. 2015; 90:55–68.
Article15. Patt YZ, Hassan MM, Lozano RD, Brown TD, Vauthey JN, Curley SA, et al. Phase II trial of systemic continuous fluorouracil and subcutaneous recombinant interferon Alfa-2b for treatment of hepatocellular carcinoma. J Clin Oncol. 2003; 21:421–7.
Article16. Portolani N, Baiocchi GL, Gheza F, Molfino S, Lomiento D, Giulini SM. Parietal and peritoneal localizations of hepatocellular carcinoma: is there a place for a curative surgery? World J Surg Oncol. 2014; 12:298.
Article17. Yeh CN, Chen MF. Resection of peritoneal implantation of hepatocellular carcinoma after hepatic resection: risk factors and prognostic analysis. World J Surg. 2004; 28:382–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Molecular Diagnosis of Ornithine Transcarbamylase Deficiency
- Acute treatment of hyperammonemia by continuous renal replacement therapy in a newborn patient with ornithine transcarbamylase deficiency
- Hyperammonemic Encephalopathy Caused by the c.386+5G>A Mutation in OTC Gene in a Young Adult Woman
- A Case of Ornithine Transcarbamylase Deficiency Successfully Treated with Protein Restriction and Living Related Liver Transplantation
- Hyperammonemic encephalopathy: An unusual presentation of fibrolamellar hepatocellular carcinoma