Cancer Res Treat.
2021 Jan;53(1):243-251. 10.4143/crt.2020.063.
Impact of the Learning Curve on the Survival of Abdominal or Minimally Invasive Radical Hysterectomy for Early-Stage Cervical Cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Institute of Women’s Life Medical Science, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Yanbian University Hospital, Yanji, China
- KMID: 2510666
- DOI: http://doi.org/10.4143/crt.2020.063
Abstract
- Purpose
The objective of this study was to define the learning curve required to attain satisfactory oncologic outcomes of cervical cancer patients who were undergoing open or minimally invasive surgery for radical hysterectomy, and to analyze the correlation between the learning curve and tumor size.
Materials and Methods
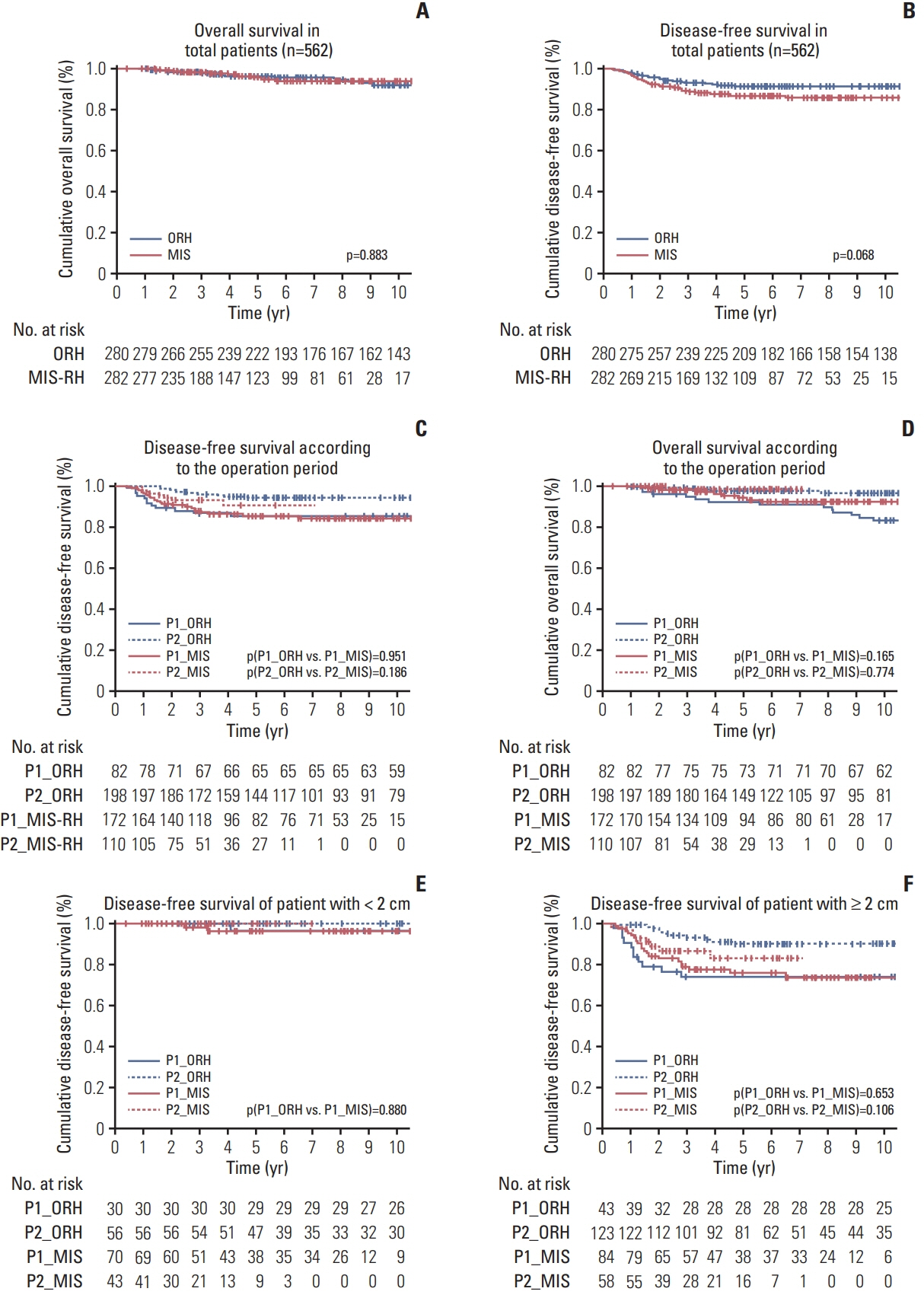
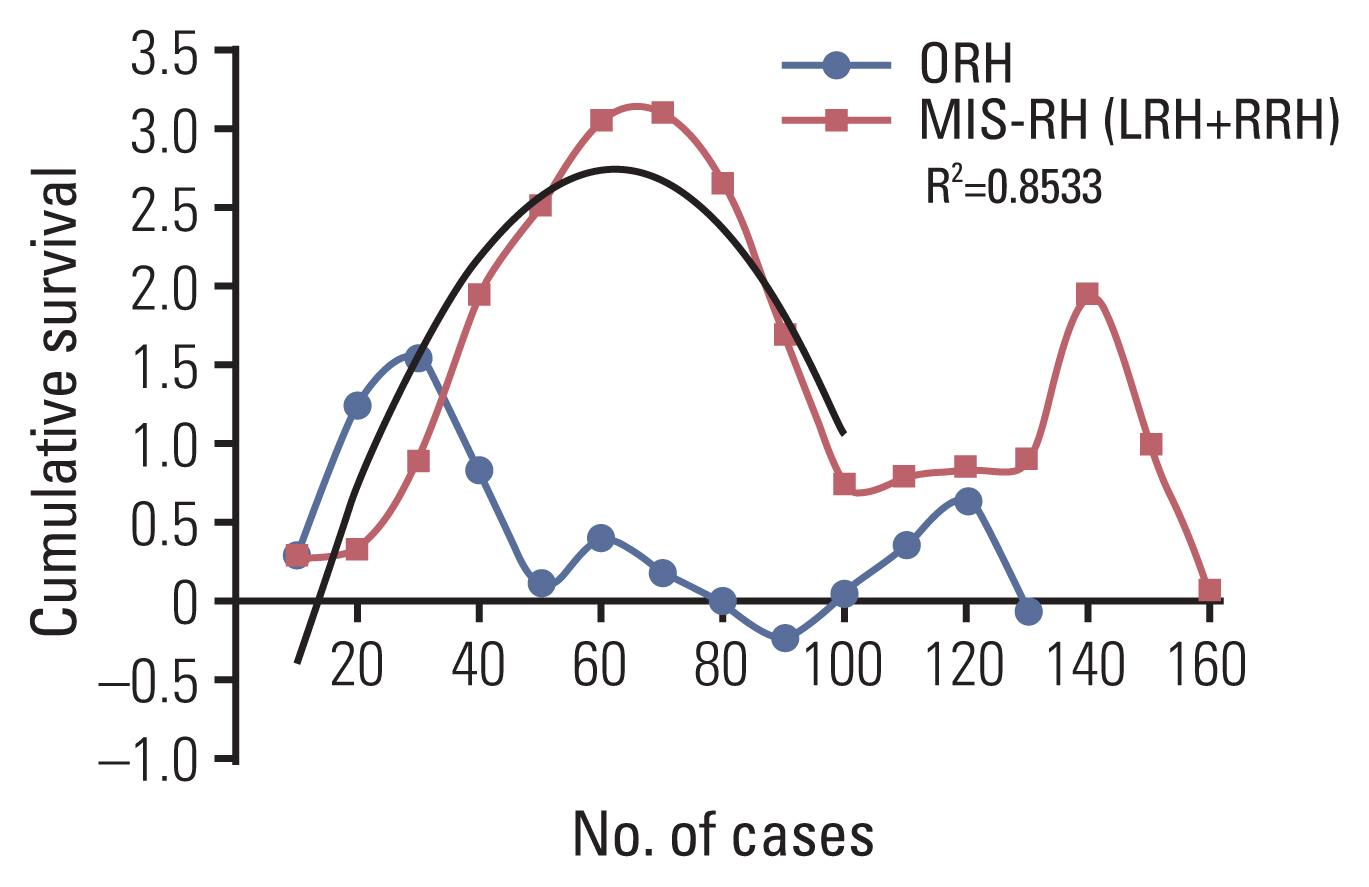
Cervical cancer patients (stage IA-IIA) who underwent open radical hysterectomy (n=280) or minimal invasive radical hysterectomy (n=282) were retrospectively reviewed. The learning curve was evaluated using cumulative sum of 5-year recurrence rates. Survival outcomes were analyzed based on the operation period (“learning period,” P1 vs. “skilled period,” P2), operation mode, and tumor size.
Results
The 5-year disease-free and overall survival rates between open and minimally invasive groups were 91.8% and 89.0% (p=0.098) and 96.1% and 97.2% (p=0.944), respectively. The number of surgeries for learning period was 30 and 60 in open and minimally invasive group, respectively. P2 had better 5-year disease-free survival than P1 after adjusting for risk factors (hazard ratio, 0.392; 95% confidence interval, 0.210 to 0.734; p=0.003). All patients with tumors < 2 cm had similar 5-year disease-free survival regardless of operation mode or learning curve. Minimally invasive group presented lower survival rates than open group when tumors ≥ 2 cm in P2. Preoperative conization improved disease-free survival in patients with tumors ≥ 2 cm, especially in minimally invasive group.
Conclusion
Minimally invasive radical hysterectomy required more cases than open group to achieve acceptable 5-year disease-free survival. When tumors ≥ 2 cm, the surgeon’s proficiency affected survival outcomes in both groups.
Figure
Reference
-
References
1. Lelle RJ, Heidenreich W, Schneider J, Morley GW. 100 years radical abdominal operation of cervix carcinoma: in memory of Wertheim’s predecessors. Zentralbl Gynakol. 1995; 117:169–74.2. Shafer A, Boggess JF. Robotic-assisted endometrial cancer staging and radical hysterectomy with the da Vinci surgical system. Gynecol Oncol. 2008; 111(2 Suppl):S18–23.
Article3. Paley PJ, Veljovich DS, Shah CA, Everett EN, Bondurant AE, Drescher CW, et al. Surgical outcomes in gynecologic oncology in the era of robotics: analysis of first 1000 cases. Am J Obstet Gynecol. 2011; 204:551.
Article4. Brudie LA, Backes FJ, Ahmad S, Zhu X, Finkler NJ, Bigsby GEt, et al. Analysis of disease recurrence and survival for women with uterine malignancies undergoing robotic surgery. Gynecol Oncol. 2013; 128:309–15.
Article5. Steed H, Rosen B, Murphy J, Laframboise S, De Petrillo D, Covens A. A comparison of laparascopic-assisted radical vaginal hysterectomy and radical abdominal hysterectomy in the treatment of cervical cancer. Gynecol Oncol. 2004; 93:588–93.
Article6. Magrina JF, Kho RM, Weaver AL, Montero RP, Magtibay PM. Robotic radical hysterectomy: comparison with laparoscopy and laparotomy. Gynecol Oncol. 2008; 109:86–91.
Article7. Chen CH, Chiu LH, Chang CW, Yen YK, Huang YH, Liu WM. Comparing robotic surgery with conventional laparoscopy and laparotomy for cervical cancer management. Int J Gynecol Cancer. 2014; 24:1105–11.
Article8. Mendivil AA, Rettenmaier MA, Abaid LN, Brown JV 3rd, Micha JP, Lopez KL, et al. Survival rate comparisons amongst cervical cancer patients treated with an open, robotic-assisted or laparoscopic radical hysterectomy: a five year experience. Surg Oncol. 2016; 25:66–71.9. Tinelli R, Malzoni M, Cosentino F, Perone C, Fusco A, Cicinelli E, et al. Robotics versus laparoscopic radical hysterectomy with lymphadenectomy in patients with early cervical cancer: a multicenter study. Ann Surg Oncol. 2011; 18:2622–8.
Article10. Estape R, Lambrou N, Diaz R, Estape E, Dunkin N, Rivera A. A case matched analysis of robotic radical hysterectomy with lymphadenectomy compared with laparoscopy and laparotomy. Gynecol Oncol. 2009; 113:357–61.
Article11. Shah CA, Beck T, Liao JB, Giannakopoulos NV, Veljovich D, Paley P. Surgical and oncologic outcomes after robotic radical hysterectomy as compared to open radical hysterectomy in the treatment of early cervical cancer. J Gynecol Oncol. 2017; 28:e82.
Article12. Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018; 379:1895–904.
Article13. Cao L, Xu H, Chen Y, Pan K, Liang Z. A detailed analysis of the learning curve: Da Vinci robot-assisted radical hysterectomy in cervical cancer. J Minim Invasive Gynecol. 2015; 22(6S):S228–9.
Article14. Yim GW, Kim SW, Nam EJ, Kim S, Kim YT. Learning curve analysis of robot-assisted radical hysterectomy for cervical cancer: initial experience at a single institution. J Gynecol Oncol. 2013; 24:303–12.
Article15. Heo YJ, Kim S, Min KJ, Lee S, Hong JH, Lee JK, et al. The comparison of surgical outcomes and learning curves of radical hysterectomy by laparoscopy and robotic system for cervical cancer: an experience of a single surgeon. Obstet Gynecol Sci. 2018; 61:468–76.
Article16. Hawkins DM, Olwell DH. Cumulative sum charts and charting for quality improvement. New York: Springer;1998.17. Lin JF, Frey M, Huang JQ. Learning curve analysis of the first 100 robotic-assisted laparoscopic hysterectomies performed by a single surgeon. Int J Gynaecol Obstet. 2014; 124:88–91.
Article18. Oyama K, Kanno K, Kojima R, Shirane A, Yanai S, Ota Y, et al. Short-term outcomes of robotic-assisted versus conventional laparoscopic radical hysterectomy for early-stage cervical cancer: a single-center study. J Obstet Gynaecol Res. 2019; 45:405–11.
Article19. Shazly SA, Murad MH, Dowdy SC, Gostout BS, Famuyide AO. Robotic radical hysterectomy in early stage cervical cancer: a systematic review and meta-analysis. Gynecol Oncol. 2015; 138:457–71.
Article20. Wallin E, Floter Radestad A, Falconer H. Introduction of robot-assisted radical hysterectomy for early stage cervical cancer: impact on complications, costs and oncologic outcome. Acta Obstet Gynecol Scand. 2017; 96:536–42.
Article21. Wang YZ, Deng L, Xu HC, Zhang Y, Liang ZQ. Laparoscopy versus laparotomy for the management of early stage cervical cancer. BMC Cancer. 2015; 15:928.
Article22. Cao T, Feng Y, Huang Q, Wan T, Liu J. Prognostic and safety roles in laparoscopic versus abdominal radical hysterectomy in cervical cancer: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2015; 25:990–8.
Article23. Roh HF, Nam SH, Kim JM. Robot-assisted laparoscopic surgery versus conventional laparoscopic surgery in randomized controlled trials: a systematic review and meta-analysis. PLoS One. 2018; 13:e0191628.
Article24. Zhou J, Xiong BH, Ma L, Cheng Y, Huang W, Zhao L. Robotic vs laparoscopic radical hysterectomy for cervical cancer: a meta-analysis. Int J Med Robot. 2016; 12:145–54.
Article25. Chong GO, Lee YH, Lee HJ, Hong DG, Lee YS. Comparison of the long-term oncological outcomes between the initial learning period of robotic and the experienced period of laparoscopic radical hysterectomy for early-stage cervical cancer. Int J Gynecol Cancer. 2018; 28:226–32.
Article26. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018; 68:7–30.
Article27. Leetanaporn K, Hanprasertpong J. Impact of obesity on clinical outcomes in patients with early-stage cervical cancer after radical hysterectomy with pelvic node dissection. Oncol Res Treat. 2019; 42:553–63.
Article28. Choi E, Lee YY, Suh M, Lee EY, Mai TTX, Ki M, et al. Socio-economic inequalities in cervical and breast cancer screening among women in Korea, 2005–2015. Yonsei Med J. 2018; 59:1026–33.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- Transvaginal cervical tumor-concealing no-look no-touch technique in minimally invasive radical hysterectomy for early-stage cervical cancer: a novel operation technique
- A comparison of robot assisted and abdominal radical hysterectomy (RH) for early stage cervical and endometrial cancer
- The twenty-first century role of Piver-Rutledge type III radical hysterectomy and FIGO stage IA, IB1, and IB2 cervical cancer in the era of robotic surgery: a personal perspective
- Feasibility and outcome of total laparoscopic radical hysterectomy with no-look no-touch technique for FIGO IB1 cervical cancer