J Korean Med Sci.
2021 Jan;36(2):e6. 10.3346/jkms.2021.36.e6.
Process of Obtaining Social Consensus and 3-Year Functional Outcomes of the First Hand Allotransplantation in Korea
- Affiliations
-
- 1W Institute for Hand & Reconstructive Microsurgery, W General Hospital, Daegu, Korea
- 2Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, Daegu, Korea
- 3Division of Nephrology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 4Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2510593
- DOI: http://doi.org/10.3346/jkms.2021.36.e6
Abstract
- Background
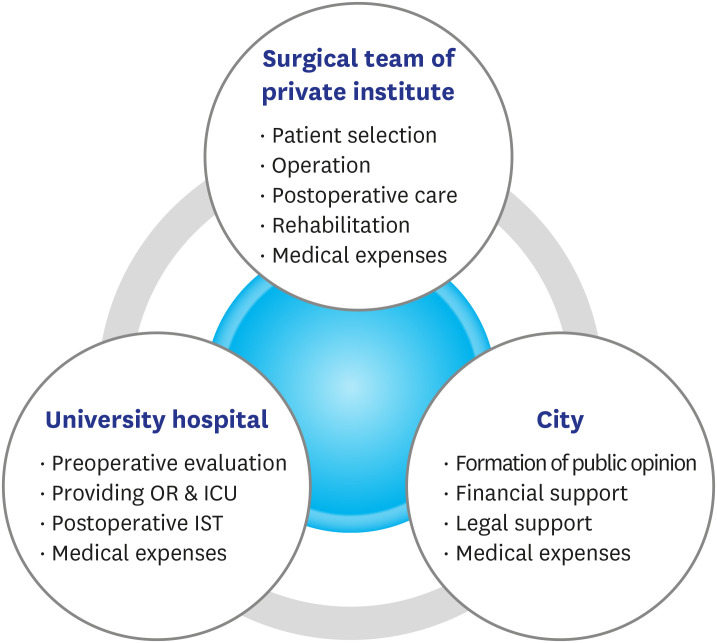
On February 2, 2017, the surgical team of ten board-certified hand specialists of W Hospital in Korea successfully performed the nation's first hand transplantation at Yeungnam University Medical Center (YUMC). This paper reports on the legal, financial, and cultural hurdles that were overcome to open the way for hand transplantation and its functional outcomes at 36 months after the operation.
Methods
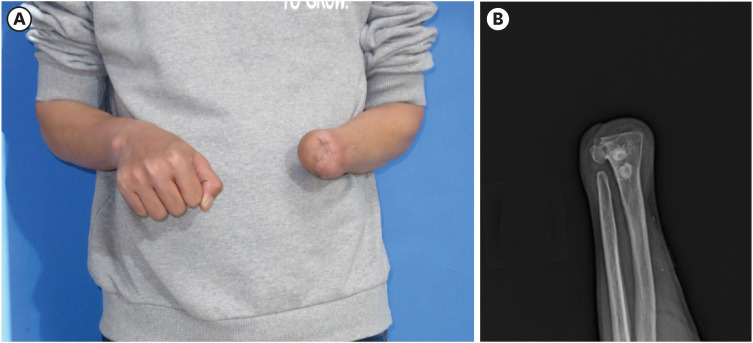
W Hospital formed a memorandum of understanding with Daegu city and YUMC to comply with government regulations regarding hand transplantation. Campaigns were initiated in the media to increase public awareness and understanding. With the city's financial and legal support and the university's medical cooperation, a surgical team performed a left distal forearm hand transplantation from a brain-dead 48-year-old man to a 35-year-old left-handed man.
Results
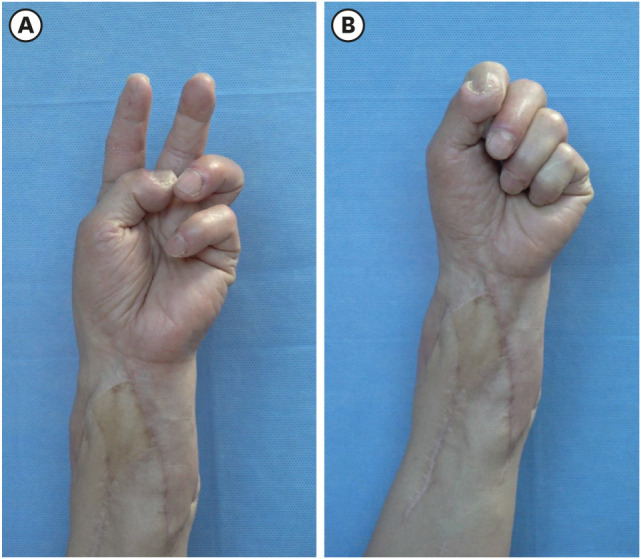
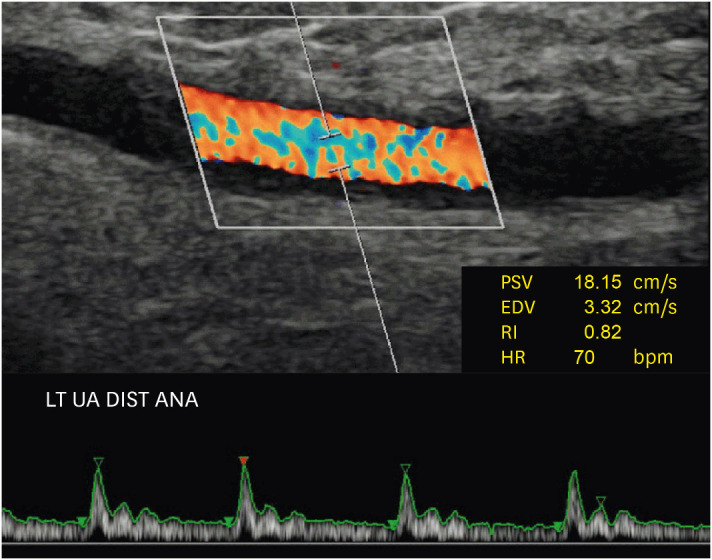
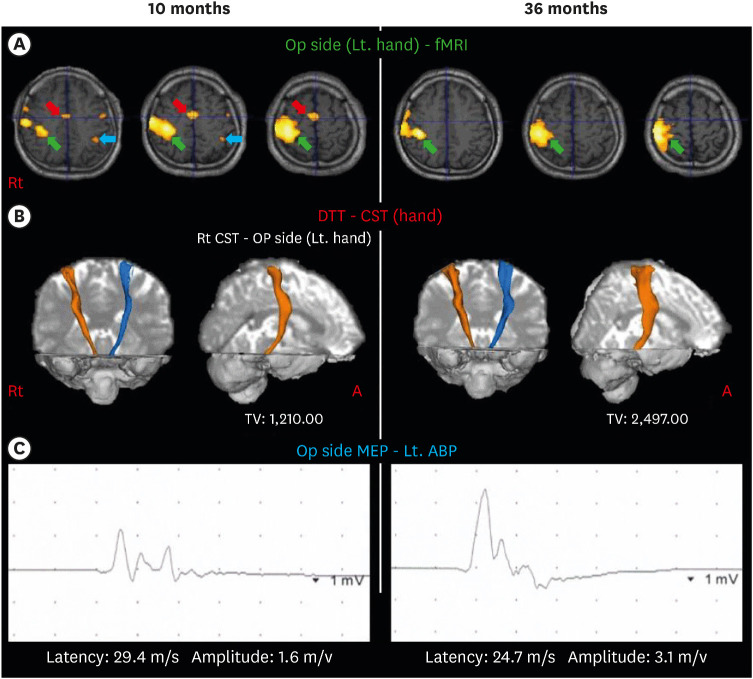
With this successful allotransplantation, the Korean Act on Organ Transplantation has now been amended to include hand transplantation. Korean national health insurance has also begun covering hand transplantation. Functional outcome at 36 months after the operation showed satisfactory progress in both motor and sensory functions. The disabilities of the arm, shoulder, and hand score were 23. The final Hand Transplantation Score was 90 points. Functional brain magnetic resonance imaging shows significant cortical reorganization of the corticospinal tract, and reinnervation of intrinsic muscle is observed.
Conclusions
Hand transplantation at the distal forearm shows very satisfactory outcomes in functional, aesthetical, and psychological aspects. Legal and financial barriers against hand transplantation have long been the most burdensome issues. Despite this momentous success, there have been no other clinical applications of vascularized composite allotransplantation due to the limited acceptance by Korean doctors and people. Further public education campaigns for vascularized composite allotransplantation are needed to increase awareness and acceptance.
Figure
Cited by 1 articles
-
History and Recent Advances in Microsurgery
Hyokyung Yoo, Byung Jun Kim
Arch Hand Microsurg. 2021;26(3):174-183. doi: 10.12790/ahm.21.0097.
Reference
-
1. Jones JW, Gruber SA, Barker JH, Breidenbach WC. Successful hand transplantation. One-year follow-up. Louisville Hand Transplant Team. N Engl J Med. 2000; 343(7):468–473. PMID: 10950668.2. Shores JT, Brandacher G, Lee WP. Hand and upper extremity transplantation: an update of outcomes in the worldwide experience. Plast Reconstr Surg. 2015; 135(2):351e–360e.3. Breidenbach WC, Meister EA, Becker GW, Turker T, Gorantla VS, Hassan K, et al. A statistical comparative assessment of face and hand transplantation outcomes to determine whether either meets the standard of care threshold. Plast Reconstr Surg. 2016; 137(1):214e–222e. PMID: 26710025.
Article4. Organ Procurement and Transplantation Network. A proposed rule by the Health and Human Services Department on 12/16/2011. Updated 2011. Accessed June 15, 2017. https://www.federalregister.gov/documents/2011/12/16/2011-2204/organ-procurement-and-transplantation-network.5. Thuong M, Petruzzo P, Landin L, Mahillo B, Kay S, Testelin S, et al. Vascularized composite allotransplantation - a Council of Europe position paper. Transpl Int. 2019; 32(3):233–240. PMID: 30387910.
Article6. Schuind F, Van Holder C, Mouraux D, Robert C, Meyer A, Salvia P, et al. The first Belgian hand transplantation--37 month term results. J Hand Surg Br. 2006; 31(4):371–376. PMID: 16527381.
Article7. Jablecki J, Kaczmarzyk L, Patrzałek D, Domanasiewicz A, Boratyńska Z. First Polish forearm transplantation: report after 17 months. Transplant Proc. 2009; 41(2):549–553. PMID: 19328923.
Article8. Pei G, Xiang D, Gu L, Wang G, Zhu L, Yu L, et al. A report of 15 hand allotransplantations in 12 patients and their outcomes in China. Transplantation. 2012; 94(10):1052–1059. PMID: 23169225.
Article9. Dwyer KM, Webb AR, Furniss HS, Anjou KE, Gibbs-Dwyer JM, McCombe DB, et al. First hand transplant procedure in Australia: outcome at 2 years. Med J Aust. 2013; 199(4):285–287. PMID: 23984788.
Article10. Singh M, Sisk G, Carty M, Sampson C, Blazar P, Dyer G, et al. Functional outcomes after bilateral hand transplantation: a 3.5-year comprehensive follow-up. Plast Reconstr Surg. 2016; 137(1):185–189. PMID: 26710022.11. Kuo YR, Chen CC, Chen YC, Yeh MC, Lin PY, Lee CH, et al. The first hand allotransplantation in Taiwan: a report at 9 months. Ann Plast Surg. 2016; 77(Suppl 1):S12–S15. PMID: 26914350.12. Amaral S, Kessler SK, Levy TJ, Gaetz W, McAndrew C, Chang B, et al. 18-month outcomes of heterologous bilateral hand transplantation in a child: a case report. Lancet Child Adolesc Health. 2017; 1(1):35–44. PMID: 30169225.
Article13. Kim JR, Elliott D, Hyde C. The influence of sociocultural factors on organ donation and transplantation in Korea: findings from key informant interviews. J Transcult Nurs. 2004; 15(2):147–154. PMID: 15070497.
Article14. National Library of Korea. A new health technology. Updated 2012. Accessed November 3, 2020. https://www.nl.go.kr/NL/contents/search.do?pageNum=1&pageSize=30&srchTarget=total&kwd=%EC%8B%A0%EC%9D%98%EB%A3%8C%EA%B8%B0%EC%88%A0+%ED%8C%94%EC%9D%B4%EC%8B%9D.15. Woo SH. The concept and current trends of composite tissue allotransplantation. J Korean Soc Reconstr Hand Surg. 2001; 1(2):84–95.16. Korea Ministry of Government Legislation. Enforcement decree of the internal organs, etc. Transplant act. Updated 2018. Accessed November 3, 2020. https://www.law.go.kr/engLsSc.do?menuId=1&subMenuId=21&tabMenuId=117&query=%EC%9E%A5%EA%B8%B0%EB%93%B1%20%EC%9D%B4%EC%8B%9D%EC%97%90%20%EA%B4%80%ED%95%9C%20%EB%B2%95%EB%A5%A0#.17. Buchanan RD. The development of the Minnesota multiphasic personality inventory. J Hist Behav Sci. 1994; 30(2):148–161. PMID: 8034964.
Article18. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988; 56(6):893–897. PMID: 3204199.
Article19. Petruzzo P, Lanzetta M, Dubernard JM, Landin L, Cavadas P, Margreiter R, et al. The international registry on hand and composite tissue transplantation. Transplantation. 2010; 90(12):1590–1594. PMID: 21052038.20. Cooney WP, Hentz VR. American Society for Surgery of the Hand. Hand transplantation--primum non nocere. J Hand Surg Am. 2002; 27(1):165–168. PMID: 11810633.
Article21. Shores JT, Malek V, Lee WPA, Brandacher G. Outcomes after hand and upper extremity transplantation. J Mater Sci Mater Med. 2017; 28(5):72. PMID: 28361279.
Article22. Schuind F, Abramowicz D, Schneeberger S. Hand transplantation: the state-of-the-art. J Hand Surg Eur Vol. 2007; 32(1):2–17. PMID: 17084950.
Article23. Burloux G. Hand transplant and body image. In : Lanzettta M, Dubernard JM, editors. Hand Transplantation. Milano: Springer;2007. p. 375–380.24. Meyer TM. Psychological aspects of mutilating hand injuries. Hand Clin. 2003; 19(1):41–49. PMID: 12683445.
Article25. Chosun Media. Seven organs simultaneous transplantation. Updated 2012. Accessed November 4, 2020. https://www.chosun.com/site/data/html_dir/2012/11/28/2012112800206.html.26. Bertrand AA, Sen S, Otake LR, Lee GK. Changing attitudes toward hand allotransplantation among North American hand surgeons. Ann Plast Surg. 2014; 72(Suppl 1):S56–60. PMID: 24740026.
Article27. Cooney CM, Siotos C, Aston JW, Bello RJ, Seal SM, Cooney DS, et al. The ethics of hand transplantation: a systematic review. J Hand Surg Am. 2018; 43(1):84.e1–84.e15. PMID: 28985978.28. Germann G. Bilateral hand transplantation--indication and rationale. J Hand Surg Br. 2001; 26(6):521. PMID: 11884102.29. Lanzetta M, Nolli R, Borgonovo A, Owen ER, Dubernard JM, Kapila H, et al. Hand transplantation: ethics, immunosuppression and indications. J Hand Surg Br. 2001; 26(6):511–516. PMID: 11884098.
Article30. Kaufman CL, Bhutiani N, Ramirez A, Tien HY, Palazzo MD, Galvis E, et al. Current status of vascularized composite allotransplantation. Am Surg. 2019; 85(6):631–637. PMID: 31267905.
Article31. Kim DH, Paik HC, Cho SH, Cho KS, Lee DY. Trachea replacement with cryopreserved tracheal allograft: experiment in dogs. J Korean Soc Transplant. 2002; 16(2):162–166.32. Park SR, Kim JH, Hwang JH, Kim KS, Lee SY. Investigation of risk acceptance and expectations in facial allotransplantation. J Korean Soc Plast Reconstr Surg. 2010; 37(5):555–560.33. Hong JW, Kim YS, Yun IS, Lee DW, Lee WJ, Roh TS, et al. Current status of face transplantation: where do we stand in Korea? Arch Craniofac Surg. 2012; 13(2):85–94.
Article34. Lim JW, Eun SC. Hemifacial transplantation model in rats. Arch Craniofac Surg. 2014; 15(2):89–93. PMID: 28913197.
Article35. Jo HK, Park JW, Hwang JH, Kim KS, Lee SY, Shin JH. Risk acceptance and expectations of laryngeal allotransplantation. Arch Plast Surg. 2014; 41(5):505–512. PMID: 25276642.
Article36. Eun SC. Facial transplantation surgery introduction. J Korean Med Sci. 2015; 30(6):669–672. PMID: 26028914.
Article37. Gómez MP, Pérez B, Manyalich M. International registry in organ donation and transplantation--2013. Transplant Proc. 2014; 46(4):1044–1048. PMID: 24815123.
Article38. Glazier AK. Regulatory oversight in the United States of vascularized composite allografts. Transpl Int. 2016; 29(6):682–685. PMID: 26284312.
Article39. Rodrigue JR, Tomich D, Fleishman A, Glazier AK. Vascularized composite allograft donation and transplantation: a survey of public attitudes in the United States. Am J Transplant. 2017; 17(10):2687–2695. PMID: 28390109.
Article40. Korean Network for Organ Sharing. Statistics of annual number of hoping organ donation. Updated 2020. Accessed November 4, 2020. https://www.konos.go.kr/konosis/common/bizlogic.jsp.41. Margreiter R, Brandacher G, Ninkovic M, Steurer W, Kreczy A, Schneeberger S. A double-hand transplant can be worth the effort! Transplantation. 2002; 74(1):85–90. PMID: 12134104.
Article42. Banegas RN, Moreno R, Duggal A, Breidenbach WC 3rd. Surgical aspects of donor hand recovery for transplantation. J Reconstr Microsurg. 2012; 28(1):21–26. PMID: 21861253.
Article43. Korea Institute for Health and Social Affairs. A survey on the disabled in 2017. Updated 2017. Accessed November 4, 2020. http://www.prism.go.kr/homepage/theme/retrieveThemeDetail.do?leftMenuLevel=110&cond_brm_super_id=NB000120061201100031424&research_id=1351000-201800347.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Limb Transplantation: Indications and Recent Results
- Second hand allotransplantation experience after the revised transplantation law: 5-month follow-up
- Reaching New Heights: A Comprehensive Study of Hand Transplantations in Korea after Institutionalization of Hand Transplantation Law
- Consensus Making Process in the Korean Academy of Medical Sciences Guideline for Physical Impairment: Evaluation as a Social Process
- Review of Current Facial Allotransplantation and Future Aspects