Korean J Transplant.
2020 Dec;34(4):244-248. 10.4285/kjt.20.0053.
Serum creatinine level at 1-month posttransplant can independently predict long-term graft survival and functional status
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2510262
- DOI: http://doi.org/10.4285/kjt.20.0053
Abstract
- Background
After the year 2000, kidney transplants with high immunologic risk and deceased donors increased rapidly in Korea. At the same time, the medical community developed special pretransplant and early posttransplantation management protocols. Our team evaluated the effect of early graft stabilization on long-term graft survival and functional status using databases from a high-volume kidney transplantation center.
Methods
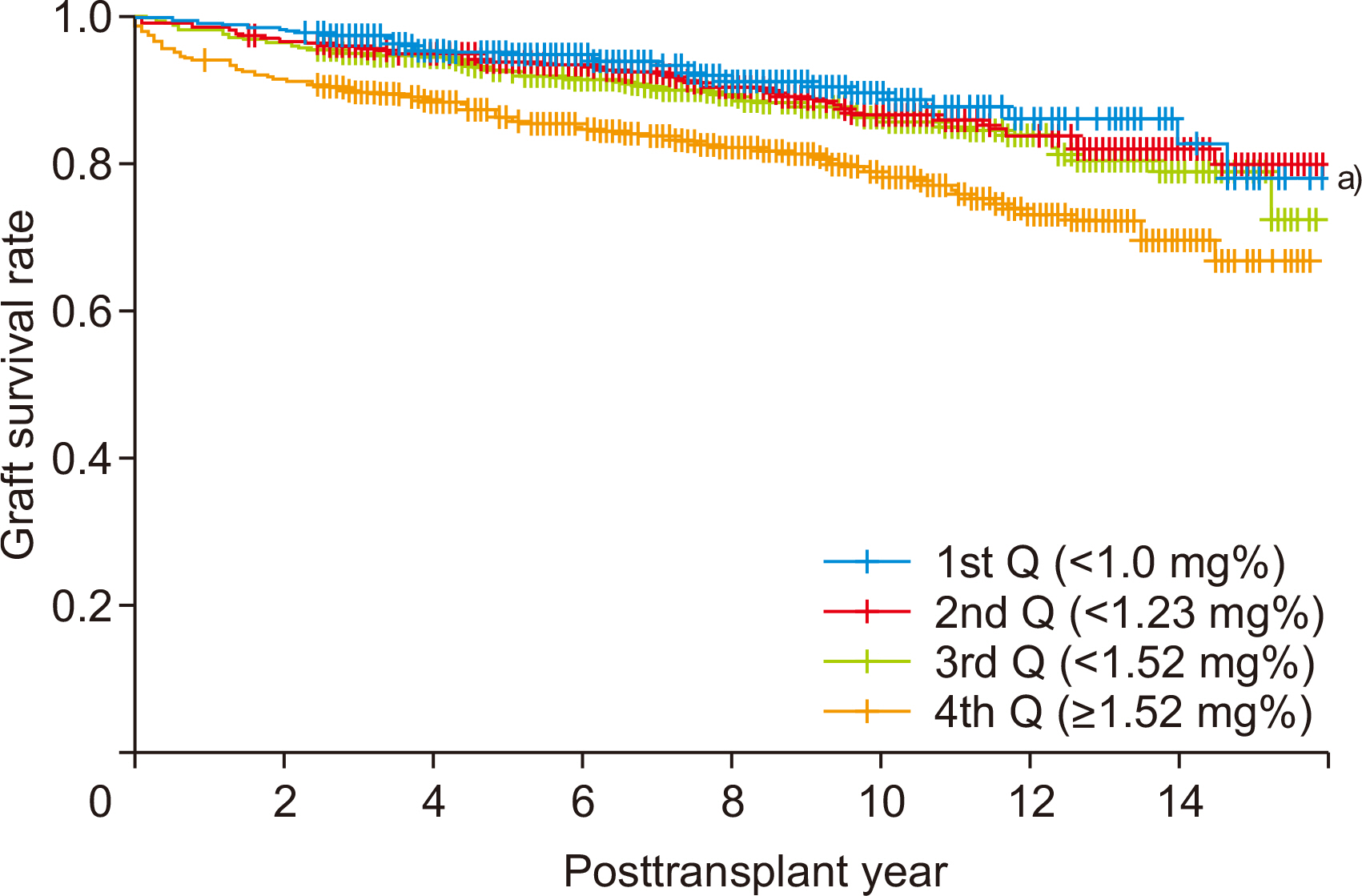
We included 1,895 kidney transplant patients from a total of 1,976 performed between 2005 and 2018. Early graft failure within 1 month (n=9), loss to follow-up (n=2), pediatric recipient or donor (n=37), and combined organ transplantation (n=33) cases were excluded. We grouped the cases at 1-month posttransplantation by serum creati-nine quantiles (1.0 mg%, 1.23 mg%, and 1.52 mg%).
Results
After an average of 95 months of follow-up (maximum 189 months), the high-se- rum creatinine group (4th quantile) showed significantly poorer graft survival than other groups (1st to 3rd quantile) (P<0.05). In multiple Cox regression analysis, a high serum creatinine level (4th quantile) at 1-month posttransplant is an independent risk factor for graft failure with a hazard ratio of 1.799 (P=0.013). The quantile group by serum cre-atinine shows a persistent, significant difference of functional graft status (glomerular filtration rate by Modification of Diet in Renal Disease method) among quantile groups beyond ten years posttransplant.
Conclusions
Serum creatinine level at 1-month posttransplant is a strong independent predictor of graft survival and functional graft status beyond ten years posttransplant.
Keyword
Figure
Reference
-
1. Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. 1999; Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 341:1725–30. DOI: 10.1056/NEJM199912023412303. PMID: 10580071.
Article2. Marcén R, Morales JM, Fernández-Rodriguez A, Capdevila L, Pallardó L, Plaza JJ, et al. 2010; Long-term graft function changes in kidney transplant recipients. NDT Plus. 3(Suppl_2):ii2–8. DOI: 10.1093/ndtplus/sfq063. PMID: 20508857. PMCID: PMC2875040.3. Salahudeen AK, May W. 2006; Cold ischemia time: Its reduction and influence on renal allograft and recipient survival in the US over the last decade. Transplantation. 82:89. DOI: 10.1097/00007890-200607152-00067.
Article4. Cecka JM. 2004; The OPTN/UNOS renal transplant registry. Clin Transpl. 1–16. PMID: 16704134.5. Held PJ, Kahan BD, Hunsicker LG, Liska D, Wolfe RA, Port FK, et al. 1994; The impact of HLA mismatches on the survival of first cadaveric kidney transplants. N Engl J Med. 331:765–70. DOI: 10.1056/NEJM199409223311203. PMID: 8065404.
Article6. Naesens M, Kuypers DR, Sarwal M. 2009; Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol. 4:481–508. DOI: 10.2215/CJN.04800908. PMID: 19218475.
Article7. Pascual M, Theruvath T, Kawai T, Tolkoff-Rubin N, Cosimi AB. 2002; Strategies to improve long-term outcomes after renal transplantation. N Engl J Med. 346:580–90. DOI: 10.1056/NEJMra011295. PMID: 11856798.
Article8. Mayer AD, Dmitrewski J, Squifflet JP, Besse T, Grabensee B, Klein B, et al. 1997; Multicenter randomized trial comparing tacrolimus (FK506) and cyclosporine in the prevention of renal allograft rejection: a report of the European Tacrolimus Multicenter Renal Study Group. Transplantation. 64:436–43. DOI: 10.1097/00007890-199708150-00012. PMID: 9275110.9. Margreiter R. European Tacrolimus vs Ciclosporin Microemulsion Renal Transplantation Study Group. 2002; Efficacy and safety of tacrolimus compared with ciclosporin microemulsion in renal transplantation: a randomised multicentre study. Lancet. 359:741–6. DOI: 10.1016/S0140-6736(02)07875-3. PMID: 11888584.
Article10. Okada D, Okumi M, Kakuta Y, Unagami K, Iizuka J, Takagi T, et al. 2018; Outcome of the risk-stratified desensitization protocol in donor-specific antibody-positive living kidney transplant recipients: a retrospective study. Transpl Int. 31:1008–17. DOI: 10.1111/tri.13269. PMID: 29676803.
Article11. Chapman JR. 2010; Clinical renal transplantation: where are we now, what are our key challenges? Transplant Proc. 42(9 Suppl):S3–6. DOI: 10.1016/j.transproceed.2010.09.017. PMID: 21095448.
Article12. Geissler EK, Schlitt HJ. 2010; The potential benefits of rapamycin on renal function, tolerance, fibrosis, and malignancy following transplantation. Kidney Int. 78:1075–9. DOI: 10.1038/ki.2010.324. PMID: 20861822.
Article13. Chapman JR. 2017; Progress in transplantation: will it be achieved in big steps or by marginal gains? Am J Kidney Dis. 69:287–95. DOI: 10.1053/j.ajkd.2016.08.024. PMID: 27823818.
Article14. Cecka JM. 1999; The UNOS Scientific Renal Transplant Registry. Clin Transpl. 1–21. PMID: 1820108.15. De La Vega LS, Torres A, Bohorquez HE, Heimbach JK, Gloor JM, Schwab TR, et al. 2004; Patient and graft outcomes from older living kidney donors are similar to those from younger donors despite lower GFR. Kidney Int. 66:1654–61. DOI: 10.1111/j.1523-1755.2004.00932.x. PMID: 15458463.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- One-month Serum Creatinine Level is the IndePendent Predictor of Long Term Graft Function Following Renal Transplant
- A report on the longest graft survival of a porcine kidney transplanted into a non-human-primate in Korea
- The Prognostic Factors for Long-term Maintenance of CAPD: Importance of Early %lean Body Mass and Peritonitis
- Early posttransplant vitamin D improvement is associated with better long-term kidney graft survival
- Graft Functions and Survivals according to the Serum Creatinine Level at 3 Days after Renal Transplantation in Living-donor Renal Transplantation