J Korean Acad Oral Health.
2020 Dec;44(4):240-245. 10.11149/jkaoh.2020.44.4.240.
Analysis of the distribution and association of periodontal disease-causing bacteria in saliva according to the severity of periodontitis in the elderly in some communities
- Affiliations
-
- 1Department of Preventive Dentistry, School of Dentistry, Daegu, Korea
- 2Department of Dental Hygiene, College of Science and Technology, Kyungpook National University, Daegu, Korea
- KMID: 2510260
- DOI: http://doi.org/10.11149/jkaoh.2020.44.4.240
Abstract
Objectives
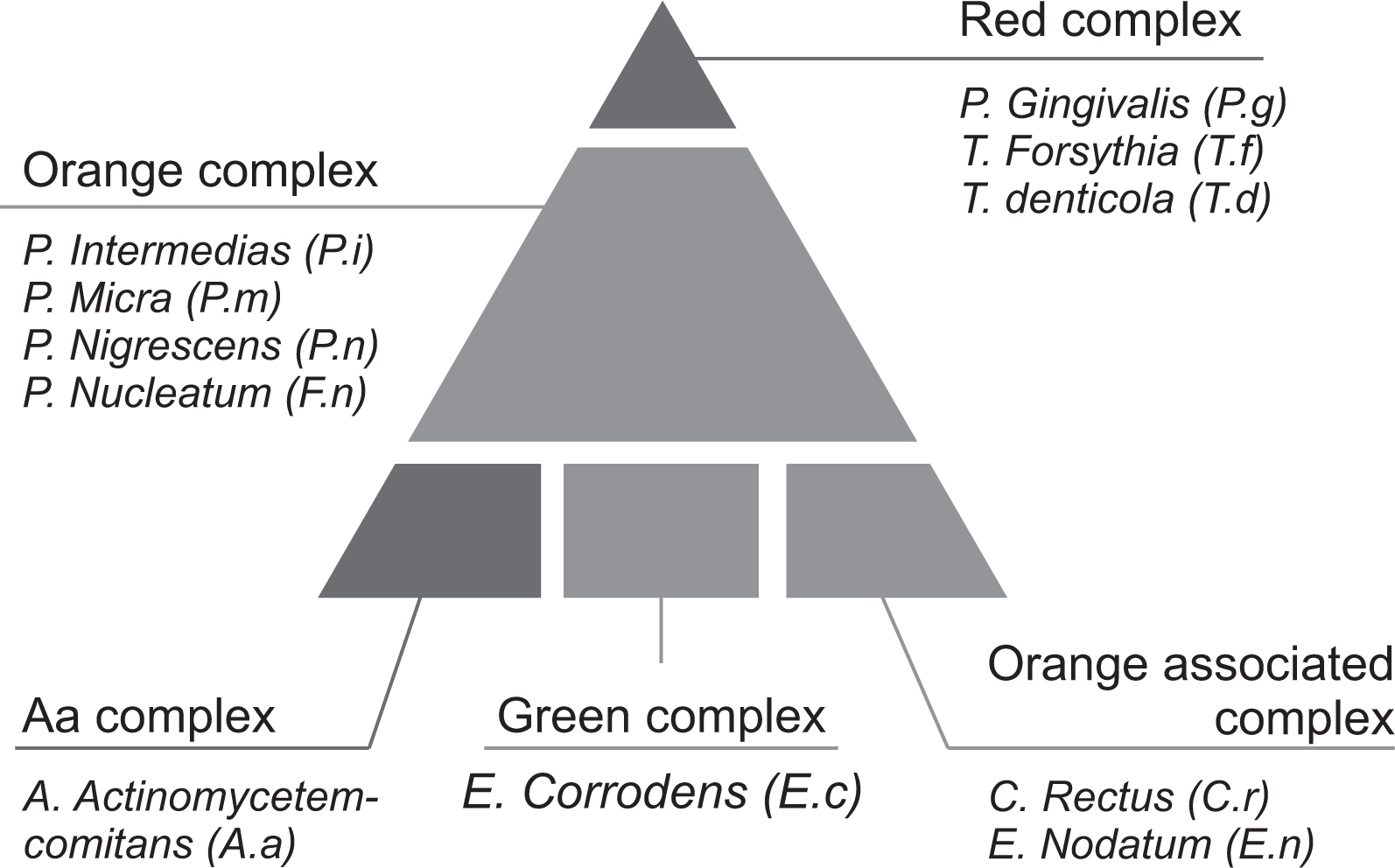
Periodontitis-causing microorganisms and their virulence factors can provoke periodontal destruction in the host. This study was aimed at evaluating the distribution of periodontal disease and its relationship with 11 periodontal disease-causing bacteria in the elderly.
Methods
Individuals aged 60 years or above were recruited after obtaining informed consent. The clinical attachment loss was measured at studied sites to determine the severity of periodontitis. Further, the stimulated salivary samples were collected and analyzed with real-time polymerase chain reaction to detect 11 strains of periodontitis-causing bacteria.
Results
The severity of periodontal disease was proportional to the amount of periodontal diseasecausing bacteria. Porphyromonas gingivalis in the red complex increased from 6.60±5.50 in stage 1 to 5.36±5.39 in stage 2 and 7.19±5.56 in stage 3 (P=0.003). Tannerella forsythia increased from 6.54±4.60 in stage 1 to 7.44±4.56 in stage 2 and 8.49±4.70 in stage 3 (P=0.007).
Conclusions
The presence of complex bacterial groups and their number of strains were high in participants with severe periodontitis. Controlling periodontitis-related bacteria is important for periodontal health in the elderly.
Keyword
Figure
Reference
-
References
1. Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent JRL. 1998; Microbial complexes in subgingival plaque. J Clin Periodontol. 25:134–144. DOI: 10.1111/j.1600-051X.1998.tb02419.x. PMID: 9495612.
Article2. Kim KK. 2003; The role of immune response in periodontal disease. Immune Netw. 3:261–267. DOI: 10.4110/in.2003.3.4.261.
Article3. Statistics. 2008. Korea National Health and Nutrition Examination Survey (KNHANES). Korean MOHW.4. Statistics. 2019. Future population estimates: 2017~2067. Korean MOHW.5. Kassebaum NJ, Smith AG, Bernabé E, Fleming TD, Reynolds AE, Vos T, et al. 2017; GBD 2015 Oral Health Collaborators. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 96:380–387. DOI: 10.1177/0022034517693566. PMID: 28792274. PMCID: PMC5912207.6. Chapple I, Wilson N. 2014; Chronic non-communicable diseases. BDJ. 216:487–487. DOI: 10.1038/sj.bdj.2014.357. PMID: 24809545.
Article7. Kim YT, Lee JH, Kweon HHI, Lee JS, Choi JK, Kim DW, et al. 2015; Evaluation of national health insurance coverage of periodontal scaling: a nationwide cohort study in Korea. J Korean Dent Assoc. 54:604–612.8. Nonnenmacher C, Dalpke A, Rochon J, Flores JL, Mutters R, Heeg K. 2005; Real time polymerase chain reaction for detection and quantification of bacteria in periodontal patients. J Periodontol. 76:1542–1549. DOI: 10.1902/jop.2005.76.9.1542. PMID: 16171445.9. Hong MH. 2014; Study on detection of oral bacteria in the saliva and risk factors of adults. J Korean Acad Industr Coop Soc. 15:5675–5682. DOI: 10.5762/KAIS.2014.15.9.5675.
Article10. Eick S, Straube A, Guentsch A, Pfister W, Jentsch H. 2011; Comparison of real-time polymerase chain reaction and DNA-strip technology in microbiological evaluation of periodontitis treatment. Diagn Micr Infec Dis. 69:12–20. DOI: 10.1016/j.diagmicrobio.2010.08.017. PMID: 21146709.
Article11. Caton JG, Armitage G, Berglundh T, Chapple IL, Jepsen S, Kornman KS, et al. 2018; A new classification scheme for periodontal and peri implant diseases and conditions-Introduction and key changes from the 1999 classification. J Periodontol. 89:S1–8. DOI: 10.1002/JPER.18-0157. PMID: 29926946.12. Peters IR, Helps CR, Hall EJ, Day MJ. 2004; Real-time RT-PCR: considerations for efficient and sensitive assay design. J Immunol Methods. 286:203–217. DOI: 10.1016/j.jim.2004.01.003. PMID: 15087233.
Article13. Jung JH, Kim KY, Jeong SH, Kim KS, Lee YM. 2014; The effect of oral health behaviors on the periodontal status of teenager. J Korean Soc Dent Hyg. 14:163–171. DOI: 10.13065/jksdh.2014.14.02.163.14. Socransky SS, Haffajee AD. 1992; The bacterial etiology of destructive periodontal disease: current concepts. J Periodontol. 63:322–331. DOI: 10.1902/jop.1992.63.4s.322. PMID: 1573546.
Article15. Choi HS. 2017; Influencing factors of dental caries across the life cycle of Koreans. J Korean Soc Dent Hyg. 10:889–898.16. Yun JH, Park JE, Kim DI, Lee SI, Choi SH, Cho KS, et al. 2008; Identification of putative periodontal pathogens in Korean chronic periodontitis patients. J Korean Acad Periodontol. 38:143–152. DOI: 10.5051/jkape.2008.38.2.143.
Article17. Bodet C, Chandad F, Grenier D. 2007; Pathogenic potential of Porphyromonas gingivalis, Treponema denticola and Tannerella forsythia, the red bacterial complex associated with periodontitis. Pathol Biol. 55:154–162. DOI: 10.1016/j.patbio.2006.07.045. PMID: 17049750.18. Mandell RL. 1984; A longitudinal microbiological investigation of Actinobacillus actinomycetemcomitans and Eikenella corrodens in juvenile periodontitis. Infect Immun. 45:778–780. DOI: 10.1128/IAI.45.3.778-780.1984. PMID: 6381313. PMCID: PMC263366.19. Haffajee AD, Bogren A, Hasturk H, Feres M, Lopez NJ, Socransky SS. 2004; Subgingival microbiota of chronic periodontitis subjects from different geographic locations. J Clin Periodontol. 31:996–1002. DOI: 10.1111/j.1600-051X.2004.00597.x. PMID: 15491316.
Article20. Schenkein HA, Burmeister JA, Koertge TE, Brooks CN, Best AM, Moore LVH, et al. 1993; The influence of race and gender on periodontal microflora. J Periodontol. 64:292–296. DOI: 10.1902/jop.1993.64.4.292. PMID: 8387107.
Article21. Petersen PE, Baehni PC. 2012; Periodontal health and global public health. Periodontol. 60:7–14. DOI: 10.1111/j.1600-0757.2012.00452.x. PMID: 22909103.
Article22. Kandelman D, Arpin S, Baez RJ, Baehni PC, Petersen PE. 2012; Oral health care systems in developing and developed countries. Periodontol. 60:98–109. DOI: 10.1111/j.1600-0757.2011.00427.x. PMID: 22909109.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microbiological links between periodontitis and systemic diseases: a brief review
- Quantitative analysis of periodontal pathogens present in the saliva of geriatric subjects
- Oral health condition according to distribution of periodontopathic bacterial complex
- A quantitative comparison of oral microbiota using various sample collection methods: a pilot study
- The Mode of Detection of Helicobacter pylori in Saliva and Subgingival Plaques of Adult Periodontitis Patients