Korean J Gastroenterol.
2020 Dec;76(6):331-336. 10.4166/kjg.2020.123.
Percutaneous Trans-splenic Obliteration for Duodenal Variceal bleeding: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Department of Radiology, Pusan National University Hospital, Busan, Korea
- KMID: 2509711
- DOI: http://doi.org/10.4166/kjg.2020.123
Abstract
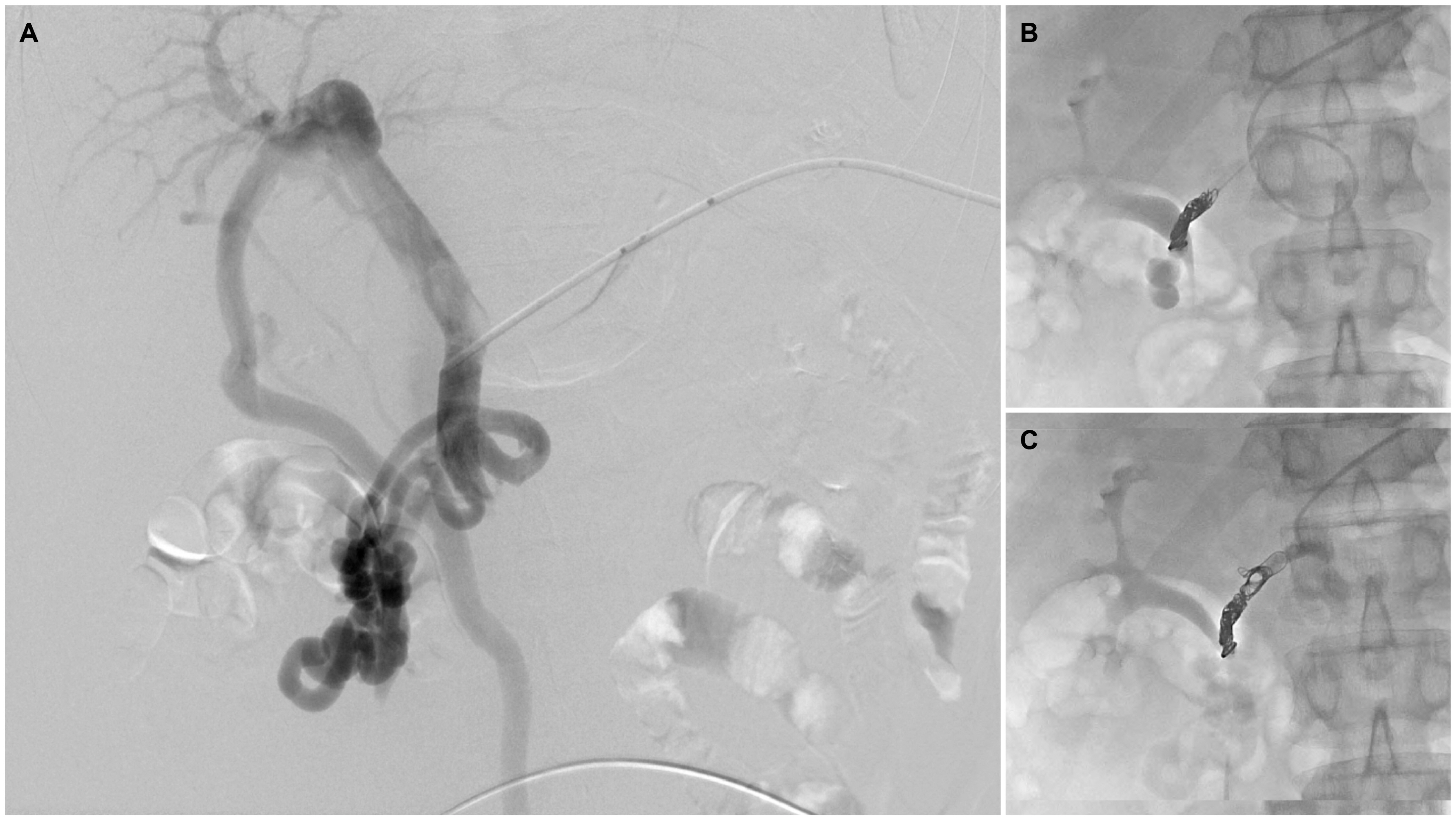
- Duodenal varices are a serious complication of portal hypertension. Bleeding from duodenal varices is rare, but when bleeding does occur, it is massive and can be fatal. Unfortunately, the optimal therapeutic modality for duodenal variceal bleeding is unclear. This paper presents a patient with duodenal variceal bleeding that was managed successfully using percutaneous trans-splenic variceal obliteration (PTVO). A 56-year-old man with a history of alcoholic cirrhosis presented with a 6-day history of melena. Emergency esophagogastroduodenoscopy revealed a large, bluish mass with a nipple sign in the second portion of the duodenum. Coil embolization of the duodenal varix was performed via a trans-splenic approach (i.e., PTVO). The patient no longer complained of melena after treatment. The duodenal varix was no longer visible at the follow-up esophagogastroduodenoscopy performed three months after PTVO. The use of PTVO might be a viable option for the treatment of duodenal variceal bleeding.
Figure
Reference
-
1. García-Pagán JC, Gracia-Sancho J, Bosch J. 2012; Functional aspects on the pathophysiology of portal hypertension in cirrhosis. J Hepatol. 57:458–461. DOI: 10.1016/j.jhep.2012.03.007. PMID: 22504334.
Article2. Kinkhabwala M, Mousavi A, Iyer S, Adamsons R. 1977; Bleeding ileal varicosity demonstrated by transhepatic portography. AJR Am J Roentgenol. 129:514–516. DOI: 10.2214/ajr.129.3.514. PMID: 409211.
Article3. Norton ID, Andrews JC, Kamath PS. 1998; Management of ectopic varices. Hepatology. 28:1154–1158. DOI: 10.1002/hep.510280434. PMID: 9755256.
Article4. Henry Z, Uppal D, Saad W, Caldwell S. 2014; Gastric and ectopic varices. Clin Liver Dis. 18:371–388. DOI: 10.1016/j.cld.2014.01.002. PMID: 24679501.
Article5. Hashimoto R, Sofue K, Takeuchi Y, Shibamoto K, Arai Y. 2013; Successful balloon-occluded retrograde transvenous obliteration for bleeding duodenal varices using cyanoacrylate. World J Gastroenterol. 19:951–954. DOI: 10.3748/wjg.v19.i6.951. PMID: 23429766. PMCID: PMC3574895.
Article6. Park SB, Lee SH, Kim JH, et al. 2013; Successful treatment of duodenal variceal bleeding by endoscopic clipping. Clin Endosc. 46:403–406. DOI: 10.5946/ce.2013.46.4.403. PMID: 23964340. PMCID: PMC3746148.
Article7. Narendra SC, Rahul R, Rajesh P, Randhir S. 2015; Endoscopic ultrasound guided emergency coil and glue for actively bleeding duodenal varix after failed endoscopy. J Dig Endosc. 6:139–141. DOI: 10.4103/0976-5042.165726.8. Kinzel J, Pichetshote N, Dredar S, Aslanian H, Nagar A. 2014; Bleeding from a duodenal varix: a unique case of variceal hemostasis achieved using EUS-guided placement of an embolization coil and cyanoacrylate. J Clin Gastroenterol. 48:362–364. DOI: 10.1097/MCG.0000000000000004. PMID: 24518801.9. Wong F. 2006; The use of TIPS in chronic liver disease. Ann Hepatol. 5:5–15. DOI: 10.1016/S1665-2681(19)32033-2.
Article10. Boyer TD, Haskal ZJ. American Association for the Study of Liver Diseases. 2005; The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology. 41:386–400. DOI: 10.1002/hep.20559. PMID: 15660434.
Article11. Kim MJ, Jang BK, Chung WJ, Hwang JS, Kim YH. 2012; Duodenal variceal bleeding after balloon-occluded retrograde transverse obliteration: treatment with transjugular intrahepatic portosystemic shunt. World J Gastroenterol. 18:2877–2880. DOI: 10.3748/wjg.v18.i22.2877. PMID: 22719200. PMCID: PMC3374995.
Article12. Ishikawa T, Imai M, Ko M, et al. 2017; Percutaneous transhepatic obliteration and percutaneous transhepatic sclerotherapy for intractable hepatic encephalopathy and gastric varices improves the hepatic function reserve. Biomed Rep. 6:99–102. DOI: 10.3892/br.2016.811. PMID: 28123716. PMCID: PMC5244787.
Article13. L'Hermin? C, Chastanet P, Delemazure O, Bonni?re PL, Durieu JP, Paris JC. 1989; Percutaneous transhepatic embolization of gastroesophageal varices: results in 400 patients. AJR Am J Roentgenol. 152:755–760. DOI: 10.2214/ajr.152.4.755. PMID: 2784259.14. Smith-Laing G, Scott J, Long RG, Dick R, Sherlock S. 1981; Role of percutaneous transhepatic obliteration of varices in the management of hemorrhage from gastroesophageal varices. Gastroenterology. 80:1031–1036. DOI: 10.1016/0016-5085(81)90077-9.
Article15. Lee JH, Kim TH, Choi JW, et al. 2019; A case report of bleeding from duodenal varices treated with percutaneous transhepatic obliteration. Int J Gastrointest Interv. 8:174–177. DOI: 10.18528/ijgii190002.
Article16. Tominaga K, Montani A, Kuga T, et al. 2001; Combined balloon-occluded embolization for treatment of concurrent duodenal, gastric, and esophageal varices: a case report. Gastrointest Endosc. 53:665–668. DOI: 10.1067/mge.2001.113279. PMID: 11323602.
Article17. Kang DH, Park JW, Jeon EY, et al. 2015; Successful treatment of bleeding duodenal varix by percutaneous transsplenic embolization. Korean J Gastroenterol. 66:286–290. DOI: 10.4166/kjg.2015.66.5.286. PMID: 26586353.
Article18. Lee JY, Song SY, Kim J, et al. 2013; Percutaneous transsplenic embolization of jejunal varices in a patient with liver cirrhosis: a case report. Abdom Imaging. 38:52–55. DOI: 10.1007/s00261-012-9894-2. PMID: 22527157.
Article19. Chu HH, Kim HC, Jae HJ, et al. 2012; Percutaneous transsplenic access to the portal vein for management of vascular complication in patients with chronic liver disease. Cardiovasc Intervent Radiol. 35:1388–1395. DOI: 10.1007/s00270-011-0311-y. PMID: 22159907.
Article20. Gong GQ, Wang XL, Wang JH, et al. 2001; Percutaneous transsplenic embolization of esophageal and gastrio-fundal varices in 18 patients. World J Gastroenterol. 7:880–883. DOI: 10.3748/wjg.v7.i6.880. PMID: 11854922. PMCID: PMC4695615.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous transvenous obliteration for duodenal variceal bleeding using micro-balloon catheter and n-butyl cyanoacrylate: A case report
- Plug-Assisted Retrograde Transvenous Obliteration for the Treatment of Duodenal Variceal Bleeding - A Case Report and Literature Review
- Successful Bridging Hemostasis Using a Sengstaken-Blakemore Tube in Massive Rectal Variceal Bleeding
- Successful Treatment of Duodenal Variceal Bleeding with Coil-Assisted Retrograde Transvenous Obliteration: A Case Report
- A case report of bleeding from duodenal varices treated with percutaneous transhepatic obliteration