J Korean Med Sci.
2020 Dec;35(48):e423. 10.3346/jkms.2020.35.e423.
Changing Patterns of Medical Visits and Factors Associated with No-show in Patients with Rheumatoid Arthritis during COVID-19 Pandemic
- Affiliations
-
- 1Department of Nursing, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea
- 3Division of Rheumatology, Department of Internal Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 4Division of Rheumatology, Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 5Division of Rheumatology, Department of Internal Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- KMID: 2509528
- DOI: http://doi.org/10.3346/jkms.2020.35.e423
Abstract
- Background
The main barrier to the effective rheumatoid arthritis (RA) therapy is poor adherence. Coronavirus disease 2019 (COVID-19) pandemic have led to a significant change in the pattern and the number of medical visits. We assessed changing patterns of medical visits and no-show, and identified factors associated with no-show in patients with RA during COVID-19 pandemic.
Methods
RA patients treated with disease-modifying antirheumatic drugs at least 6 months who had been in remission or those with mild disease activity were observed for 6 months from February to July 2020. No-show was defined as a missed appointment that was not previously cancelled by the patient and several variables that might affect no-show were examined.
Results
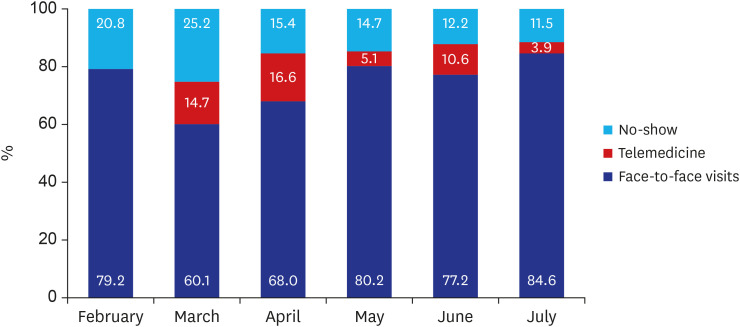
A total of 376 patients and 1,189 appointments were evaluated. Among 376 patients, 164 patients (43.6%) missed appointment more than one time and no-show rate was 17.2% during COVID-19 pandemic. During the observation, face-to-face visits gradually increased and no-show gradually decreased. The logistic regression analysis identified previous history of no-show (adjusted odds ratio [OR], 2.225; 95% confidence interval [CI], 1.422–3.479; P < 0.001) and fewer numbers of comorbidities (adjusted OR, 0.749; 95% CI, 0.584–0.961; P = 0.023) as the independent factors associated with no-show.
Conclusion
Monthly analysis showed that the no-show rate and the pattern of medical visits gradually changed in patients with RA during COVID-19 pandemic. Moreover, we found that previous history of no-show and fewer numbers of comorbidities as the independent factors associated with no-show.
Keyword
Figure
Cited by 1 articles
-
Impact of the COVID-19 Outbreak on Emergency Care Utilization in Patients with Acute Myocardial Infarction: a Nationwide Population-based Study
Ho Kyung Sung, Jin Hui Paik, Yu Jin Lee, Soo Kang
J Korean Med Sci. 2021;36(16):e111. doi: 10.3346/jkms.2021.36.e111.
Reference
-
1. World Health Organization. Coronavirus disease (COVID-2019) situation report-143. Updated 2020. Accessed November 5, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.2. Korea Centers for Disease control and Prevention. Coronavirus disease-19 main website. Updated 2020. Accessed November 6, 2020. http://ncov.mohw.go.kr/en.3. Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020; 38(9):1732–1736. PMID: 32738468.
Article4. Ham CH, Moon HJ, Kim JH, Park YK, Lee TH, Kwon WK. Coronavirus disease (COVID-19) outbreak and its impact on spinal daily practice: preliminary report from a single (regional) university hospital in Republic of Korea. J Korean Neurosurg Soc. 2020; 63(4):407–414. PMID: 32455517.5. Smolen JS, Landewé RB, Bijlsma JW, Burmester GR, Dougados M, Kerschbaumer A, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020; 79(6):685–699. PMID: 31969328.6. Lindqvist E, Jonsson K, Saxne T, Eberhardt K. Course of radiographic damage over 10 years in a cohort with early rheumatoid arthritis. Ann Rheum Dis. 2003; 62(7):611–616. PMID: 12810421.
Article7. Weinblatt ME, Kremer JM, Bankhurst AD, Bulpitt KJ, Fleischmann RM, Fox RI, et al. A trial of etanercept, a recombinant tumor necrosis factor receptor:Fc fusion protein, in patients with rheumatoid arthritis receiving methotrexate. N Engl J Med. 1999; 340(4):253–259. PMID: 9920948.
Article8. Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, et al. Infliximab and methotrexate in the treatment of rheumatoid arthritis. N Engl J Med. 2000; 343(22):1594–1602. PMID: 11096166.
Article9. Keystone EC, Kavanaugh AF, Sharp JT, Tannenbaum H, Hua Y, Teoh LS, et al. Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo-controlled, 52-week trial. Arthritis Rheum. 2004; 50(5):1400–1411. PMID: 15146409.
Article10. Waimann CA, Marengo MF, de Achaval S, Cox VL, Garcia-Gonzalez A, Reveille JD, et al. Electronic monitoring of oral therapies in ethnically diverse and economically disadvantaged patients with rheumatoid arthritis: consequences of low adherence. Arthritis Rheum. 2013; 65(6):1421–1429. PMID: 23728826.
Article11. Alaeddini A, Yang K, Reddy C, Yu S. A probabilistic model for predicting the probability of no-show in hospital appointments. Health Care Manage Sci. 2011; 14(2):146–157.
Article12. Hallsworth M, Berry D, Sanders M, Sallis A, King D, Vlaev I, et al. Stating appointment costs in SMS reminders reduces missed hospital appointments: findings from two randomised controlled trials. PLoS One. 2015; 10(9):e0137306. PMID: 26366885.
Article13. Peng Y, Erdem E, Shi J, Masek C, Woodbridge P. Large-scale assessment of missed opportunity risks in a complex hospital setting. Inform Health Soc Care. 2016; 41(2):112–127. PMID: 25325215.
Article14. Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. Am J Med. 2010; 123(6):542–548. PMID: 20569761.
Article15. Bech M. The economics of non-attendance and the expected effect of charging a fine on non-attendees. Health Policy. 2005; 74(2):181–191. PMID: 16153478.
Article16. Odonkor CA, Christiansen S, Chen Y, Sathiyakumar A, Chaudhry H, Cinquegrana D, et al. Factors associated with missed appointments at an academic pain treatment center: a prospective year-long longitudinal study. Anesth Analg. 2017; 125(2):562–570. PMID: 28277318.17. Dantas LF, Fleck JL, Cyrino Oliveira FL, Hamacher S. No-shows in appointment scheduling - a systematic literature review. Health Policy. 2018; 122(4):412–421. PMID: 29482948.
Article18. Kang CR, Bang JH, Cho SI. Factors contributing to missed visits for medical care among human immunodeficiency virus-infected adults in Seoul, Korea. J Korean Med Sci. 2018; 33(42):e261. PMID: 30310363.
Article19. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010; 62(9):2569–2581. PMID: 20872595.20. Torres O, Rothberg MB, Garb J, Ogunneye O, Onyema J, Higgins T. Risk factor model to predict a missed clinic appointment in an urban, academic, and underserved setting. Popul Health Manag. 2015; 18(2):131–136. PMID: 25299396.
Article21. Kempny A, Diller GP, Dimopoulos K, Alonso-Gonzalez R, Uebing A, Li W, et al. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int J Cardiol. 2016; 203:245–250. PMID: 26519677.
Article22. Lee VJ, Earnest A, Chen MI, Krishnan B. Predictors of failed attendances in a multi-specialty outpatient centre using electronic databases. BMC Health Serv Res. 2005; 5(1):51. PMID: 16083504.
Article23. Cronin PR, DeCoste L, Kimball AB. A multivariate analysis of dermatology missed appointment predictors. JAMA Dermatol. 2013; 149(12):1435–1437. PMID: 24080767.
Article24. Giunta D, Briatore A, Baum A, Luna D, Waisman G, de Quiros FG. Factors associated with nonattendance at clinical medicine scheduled outpatient appointments in a university general hospital. Patient Prefer Adherence. 2013; 7:1163–1170. PMID: 24235820.25. Lee S, So MW, Ahn E. Long-term adherence and persistence with febuxostat among male patients with gout in a routine clinical setting. Mod Rheumatol. 2019; 29(4):662–668. PMID: 29856667.
Article26. Ade S, Trébucq A, Harries AD, Ade G, Agodokpessi G, Wachinou P, et al. Follow-up and tracing of tuberculosis patients who fail to attend their scheduled appointments in Cotonou, Benin: a retrospective cohort study. BMC Health Serv Res. 2016; 16(1):5. PMID: 26754808.
Article27. Traeger L, O'Cleirigh C, Skeer MR, Mayer KH, Safren SA. Risk factors for missed HIV primary care visits among men who have sex with men. J Behav Med. 2012; 35(5):548–556. PMID: 22068878.
Article28. Baggarly SA, Kemp RJ, Wang X, Magoun AD. Factors associated with medication adherence and persistence of treatment for hypertension in a Medicaid population. Res Social Adm Pharm. 2014; 10(6):e99–112. PMID: 24731547.
Article29. Rodriguez F, Cannon CP, Steg PG, Kumbhani DJ, Goto S, Smith SC, et al. Predictors of long-term adherence to evidence-based cardiovascular disease medications in outpatients with stable atherothrombotic disease: findings from the REACH Registry. Clin Cardiol. 2013; 36(12):721–727. PMID: 24166484.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Correction of Author’s Affiliation in the Article “Changing Patterns of Medical Visits and Factors Associated With No-show in Patients With Rheumatoid Arthritis During COVID-19 Pandemic”
- Psychiatric Inpatient Care During the COVID-19 Pandemic: A Review
- The Management of Thyroid Disease in COVID-19 Pandemic
- Tracheostomy in the Era of COVID-19 Pandemic
- The COVID-19 pandemic's impact on prostate cancer screening and diagnosis in Korea