Int J Thyroidol.
2020 Nov;13(2):111-117. 10.11106/ijt.2020.13.2.111.
Predictive Risk Factors for Recurrence or Metastasis in Papillary Thyroid Cancer
- Affiliations
-
- 1Department of Surgery, Kyungpook National University, School of Medicine, Daegu, Korea
- 2Department of Pathology, Kyungpook National University, School of Medicine, Daegu, Korea
- 3Department of Otolaryngology-Head and Neck Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA
- KMID: 2509189
- DOI: http://doi.org/10.11106/ijt.2020.13.2.111
Abstract
- Background and Objectives
This study investigated predictive risk factors for cervical nodal recurrence or metastasis in papillary thyroid carcinoma (PTC).
Materials and Methods
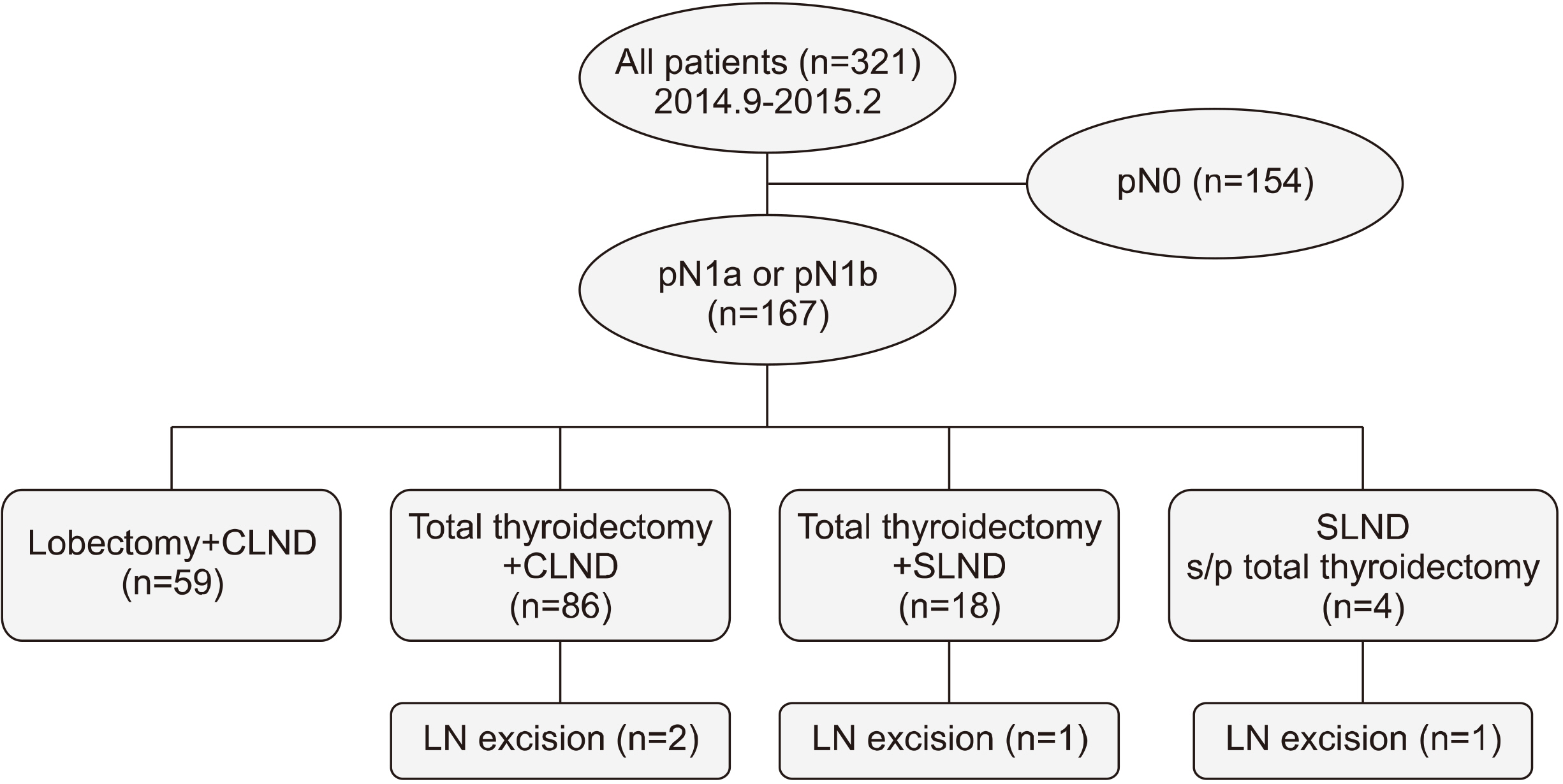
From September 2014 to February 2015, a total of 321 PTC patients were enrolled retrospectively. Except for 154 N0 patients, the remaining 167 patients were divided into two groups as follows: Group I (n=140), central lymph node (LN) metastasis (pN1a); Group II (n=27), lateral LN metastasis (pN1b, n=23) or LN recurrence (n=4). The patients who had LN metastasis or recurrence underwent selective LN dissection or recurrent LN excision.
Results
Central LN metastases were found in 44.0% (142/321) of patients. Two hundred thirty patients (71.7%) were classified as being at low-risk for LN disease, as evidenced by N0 or fewer than five micrometastases. The mean size of central metastatic LNs was 0.37±0.34 cm. A total of 76 patients (46.6%) presented with micrometastasis, and ten (3.1%) presented with extranodal extension (ENE). The multiple/bilateral cancer, Extrathyroidal extension, size of metastatic LN, ENE, high risk LN disease (>5, macrometastasis, >3.0 cm) and high thyroglobulin were significant risk factors in predicting LN recurrence or lateral LN metastasis (p<0.05) in univariate analysis. Patients with ENE were 10.3 times more at risk for recurrence or metastasis than patients without ENE.
Conclusion
We consider the ENE was the most potent risk factors for LN recurrence or lateral LN metastasis in PTC.
Keyword
Figure
Reference
-
References
1. Seo GH, Chung JH. 2014; Analysis of therapeutic modalities of thyroid cancer in Korea between 2008 and 2012. J Korean Thyroid Assoc. 7(02):167–71. DOI: 10.11106/cet.2014.7.2.167.
Article2. Cho BY, Choi HS, Park YJ, Lim JA, Ahn HY, Lee EK, et al. 2013; Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid. 23(7):797–804. DOI: 10.1089/thy.2012.0329. PMID: 23427907. PMCID: PMC3704118.
Article3. Ortiz S, Rodriguez JM, Soria T, Perez-Flores D, Pinero A, Moreno J, et al. 2001; Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic study. Otolaryngol Head Neck Surg. 124(3):261–5. DOI: 10.1067/mhn.2001.113141. PMID: 11240987.
Article4. Shah JP, Loree TR, Dharker D, Strong EW, Begg C, Vlamis V. 1992; Prognostic factors in differentiated carcinoma of the thyroid gland. Am J Surg. 164(6):658–61. DOI: 10.1016/S0002-9610(05)80729-9. PMID: 1463119.
Article5. Teixeira G, Teixeira T, Gubert F, Chikota H, Tufano R. 2011; The incidence of central neck micrometastatic disease in patients with papillary thyroid cancer staged preoperatively and intraoperatively as N0. Surgery. 150(6):1161–7. DOI: 10.1016/j.surg.2011.09.019. PMID: 22136836.
Article6. Park CH, Song CM, Ji YB, Pyo JY, Yi KJ, Song YS, et al. 2015; Significance of the extracapsular spread of metastatic lymph nodes in papillary thyroid carcinoma. Clin Exp Otorhinolaryngol. 8(3):289–94. DOI: 10.3342/ceo.2015.8.3.289. PMID: 26330926. PMCID: PMC4553362.
Article7. Liu FH, Kuo SF, Hsueh C, Chao TC, Lin JD. 2015; Postoperative recurrence of papillary thyroid carcinoma with lymph node metastasis. J Surg Oncol. 112(2):149–54. DOI: 10.1002/jso.23967. PMID: 26175314. PMCID: PMC5034820.
Article8. Grogan RH, Kaplan SP, Cao H, Weiss RE, Degroot LJ, Simon CA, et al. 2013; A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery. 154(6):1436–46. discussion 46–7. DOI: 10.1016/j.surg.2013.07.008. PMID: 24075674.
Article9. Wada N, Suganuma N, Nakayama H, Masudo K, Rino Y, Masuda M, et al. 2007; Microscopic regional lymph node status in papillary thyroid carcinoma with and without lymphadenopathy and its relation to outcomes. Langenbecks Arch Surg. 392(4):417–22. DOI: 10.1007/s00423-007-0159-4. PMID: 17562092.
Article10. Lundgren CI, Hall P, Dickman PW, Zedenius J. 2006; Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 106(3):524–31. DOI: 10.1002/cncr.21653. PMID: 16369995.11. Jeon MJ, Yoon JH, Han JM, Yim JH, Hong SJ, Song DE, et al. 2013; The prognostic value of the metastatic lymph node ratio and maximal metastatic tumor size in pathological N1a papillary thyroid carcinoma. Eur J Endocrinol. 168(2):219–25. DOI: 10.1530/EJE-12-0744. PMID: 23161752.
Article12. Clain JB, Scherl S, Dos Reis L, Turk A, Wenig BM, Mehra S, et al. 2014; Extrathyroidal extension predicts extranodal extension in patients with positive lymph nodes: an important association that may affect clinical management. Thyroid. 24(6):951–7. DOI: 10.1089/thy.2013.0557. PMID: 24443878.
Article13. Cho SY, Lee TH, Ku YH, Kim HI, Lee GH, Kim MJ. 2015; Central lymph node metastasis in papillary thyroid microcarcinoma can be stratified according to the number, the size of metastatic foci, and the presence of desmoplasia. Surgery. 157(1):111–8. DOI: 10.1016/j.surg.2014.05.023. PMID: 25444224.
Article14. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. 2012; The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 22(11):1144–52. DOI: 10.1089/thy.2012.0043. PMID: 23083442.
Article15. Lango M, Flieder D, Arrangoiz R, Veloski C, Yu JQ, Li T, et al. 2013; Extranodal extension of metastatic papillary thyroid carcinoma: correlation with biochemical endpoints, nodal persis-tence, and systemic disease progression. Thyroid. 23(9):1099–105. DOI: 10.1089/thy.2013.0027. PMID: 23421588. PMCID: PMC3770240.
Article16. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2016; 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133. DOI: 10.1089/thy.2015.0020. PMID: 26462967. PMCID: PMC4739132.17. Lee J, Song Y, Soh EY. 2014; Prognostic significance of the number of metastatic lymph nodes to stratify the risk of recurrence. World J Surg. 38(4):858–62. DOI: 10.1007/s00268-013-2345-6. PMID: 24305921.
Article18. Lang BH, Tang AH, Wong KP, Shek TW, Wan KY, Lo CY. 2012; Significance of size of lymph node metastasis on postsurgical stimulated thyroglobulin levels after prophylactic unilateral central neck dissection in papillary thyroid carcinoma. Ann Surg Oncol. 19(11):3472–8. DOI: 10.1245/s10434-012-2385-4. PMID: 22565664. PMCID: PMC3442170.
Article19. Cranshaw IM, Carnaille B. 2008; Micrometastases in thyroid cancer. An important finding? Surg Oncol. 17(3):253–8. DOI: 10.1016/j.suronc.2008.04.005. PMID: 18504121.
Article20. Kim SY, Kim BW, Pyo JY, Hong SW, Chang HS, Park CS. 2018; Macrometastasis in papillary thyroid cancer patients is associated with higher recurrence in lateral neck nodes. World J Surg. 42(1):123–9. DOI: 10.1007/s00268-017-4158-5. PMID: 28779384.
Article21. Wu MH, Shen WT, Gosnell J, Duh QY. 2015; Prognostic significance of extranodal extension of regional lymph node metastasis in papillary thyroid cancer. Head Neck. 37(9):1336–43. DOI: 10.1002/hed.23747. PMID: 24821456.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Lobectomy as an Initial Treatment Option on 1-4 cm Papillary Cancer
- Comparison of Neck CT and ¹â¸F-FDG PET-CT for Making the Preoperative Diagnosis of Lymph Node Metastasis in Papillary Thyroid Cancer
- A Study on the Risk Factors for Recurrence of Recurrent Papillary Thyroid Cancer after Surgery
- The Clinical Significance of Preoperative Serum Neutrophil-Lymphocyte Ratio (NLR) in Papillary Thyroid Cancer Patients
- Clinico-pathologic Characteristics of the Primary Thyroid Cancer in Patients with Breast Cancer