J Korean Med Sci.
2020 Dec;35(46):e397. 10.3346/jkms.2020.35.e397.
Implantable Cardioverter-defibrillator Utilization and Its Outcomes in Korea: Data from Korean Acute Heart Failure Registry
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Internal Medicine, Heart Research Center, Chonnam National University, Gwangju, Korea
- 4Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 5Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 6Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea
- 7Department of Internal Medicine, School of Medicine, Sungkyunkwan University, Seoul, Korea
- 8Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea
- 9Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea
- 10Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2509038
- DOI: http://doi.org/10.3346/jkms.2020.35.e397
Abstract
- Background
There are sparse data on the utilization rate of implantable cardioverterdefibrillator (ICD) and its beneficial effects in Korean patients with heart failure with reduced left ventricular ejection fraction (LVEF).
Methods
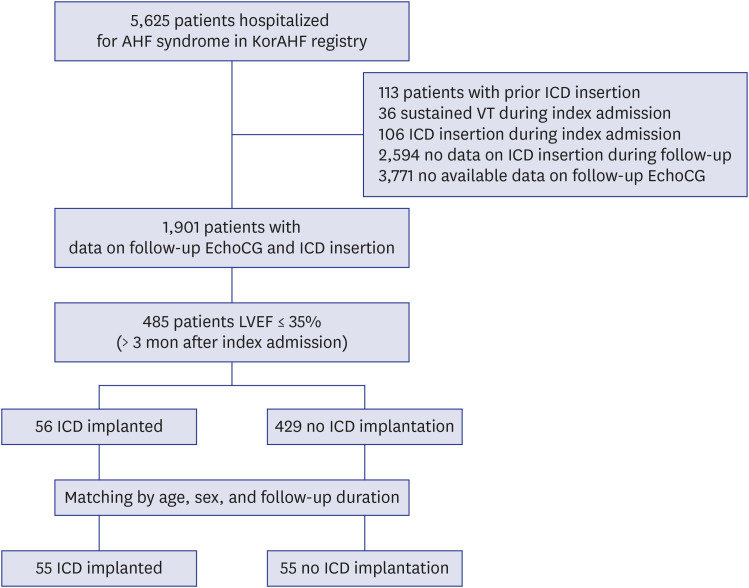
Among 5,625 acute heart failure (AHF) patients from 10 tertiary university hospitals across Korea, 485 patients with reassessed LVEF ≤ 35% at least 3 months after the index admission were enrolled in this study. The ICD implantation during the follow-up was evaluated. Mortality was compared between patients with ICDs and age-, sex-, and follow-up duration matched control patients.
Results
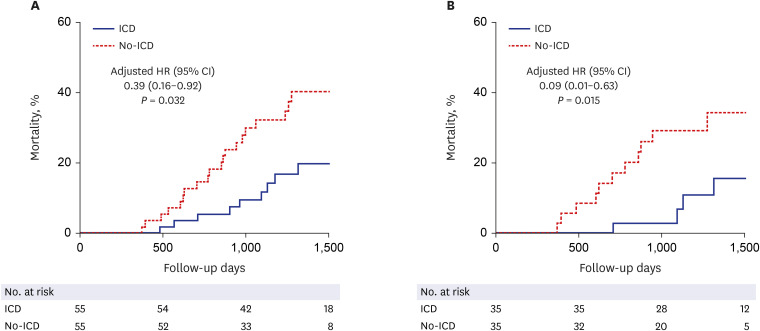
Among 485 patients potentially indicated for an ICD for primary prevention, only 56 patients (11.5%) underwent ICD implantation during the follow-up. Patients with ICD showed a significantly lower all-cause mortality compared with their matched control population: adjusted hazard ratio (HR) (95% confidence interval [CI]) = 0.39 (0.16–0.92), P = 0.032. The mortality rate was still lower in the ICD group after excluding patients with cardiac resynchronization therapy (adjusted HR [95% CI] = 0.09 [0.01–0.63], P = 0.015). According to the subgroup analysis for ischemic heart failure, there was a significantly lower all-cause mortality in the ICD group than in the no-ICD group (HR [95% CI] = 0.20 [0.06– 0.72], P = 0.013), with a borderline statistical significance (interaction P = 0.069).
Conclusion
Follow-up data of this large, multicenter registry suggests a significant underutilization of ICD in Korean heart failure patients with reduced LVEF. Survival analysis implies that previously proven survival benefit of ICD in clinical trials could be extrapolated to Korean patients.
Figure
Reference
-
1. Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS Guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018; 72(14):e91–220. PMID: 29097296.2. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37(27):2129–2200. PMID: 27206819.3. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017; 70(6):776–803. PMID: 28461007.4. Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002; 346(12):877–883. PMID: 11907286.
Article5. Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005; 352(3):225–237. PMID: 15659722.
Article6. Garg R, Yusuf S. Collaborative Group on ACE Inhibitor Trials. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. JAMA. 1995; 273(18):1450–1456. PMID: 7654275.
Article7. Hjalmarson A, Goldstein S, Fagerberg B, Wedel H, Waagstein F, Kjekshus J, et al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). JAMA. 2000; 283(10):1295–1302. PMID: 10714728.
Article8. Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001; 357(9266):1385–1390. PMID: 11356434.9. Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN. SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991; 325(5):293–302. PMID: 2057034.
Article10. Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001; 344(22):1651–1658. PMID: 11386263.
Article11. Choi KH, Lee GY, Choi JO, Jeon ES, Lee HY, Cho HJ, et al. Effects of angiotensin receptor blocker at discharge in patients with heart failure with reduced ejection fraction: Korean Acute Heart Failure (KorAHF) registry. Int J Cardiol . 2018; 257:168–176. PMID: 29506690.
Article12. Youn JC, Kim JJ, Kwon A, Lee HY, Kang SM, Baek SH. Dose response relationship of RAS blocker and beta-blocker in patients with acute heart failure syndrome: data from the Korean Acute Hart Failure (KorAHF) registry. J Card Fail. 2019; 25(8):S142.
Article13. Lee SE, Cho HJ, Lee HY, Yang HM, Choi JO, Jeon ES, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014; 16(6):700–708. PMID: 24797348.
Article14. Kang J, Park JJ, Cho YJ, Oh IY, Park HA, Lee SE, et al. Predictors and prognostic value of worsening renal function during admission in HFpEF versus HFrEF: data from the KorAHF (Korean Acute Heart Failure) registry. J Am Heart Assoc. 2018; 7(6):e007910. PMID: 29535141.
Article15. Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure registry (KorAHF). Korean Circ J. 2017; 47(3):341–353. PMID: 28567084.
Article16. Hohnloser SH, Kuck KH, Dorian P, Roberts RS, Hampton JR, Hatala R, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med. 2004; 351(24):2481–2488. PMID: 15590950.
Article17. Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004; 350(21):2151–2158. PMID: 15152060.
Article18. Kolodziejczak M, Andreotti F, Kowalewski M, Buffon A, Ciccone MM, Parati G, et al. Implantable cardioverter-defibrillators for primary prevention in patients with ischemic or nonischemic cardiomyopathy: a systematic review and meta-analysis. Ann Intern Med. 2017; 167(2):103–111. PMID: 28632280.19. Miller AL, Gosch K, Daugherty SL, Rathore S, Peterson PN, Peterson ED, et al. Failure to reassess ejection fraction after acute myocardial infarction in potential implantable cardioverter/defibrillator candidates: insights from the Translational Research Investigating Underlying disparities in acute myocardial infarction patients' health status (TRIUMPH) registry. Am Heart J. 2013; 166(4):737–743. PMID: 24093855.
Article20. Pokorney SD, Miller AL, Chen AY, Thomas L, Fonarow GC, de Lemos JA, et al. Reassessment of cardiac function and implantable cardioverter-defibrillator use among medicare patients with low ejection fraction after myocardial infarction. Circulation. 2017; 135(1):38–47. PMID: 27881561.
Article21. Schrage B, Uijl A, Benson L, Westermann D, Ståhlberg M, Stolfo D, et al. Association between use of primary-prevention implantable cardioverter-defibrillators and mortality in patients with heart failure: a prospective propensity score-matched analysis from the Swedish heart failure registry. Circulation. 2019; 140(19):1530–1539. PMID: 31476893.22. Roh SY, Choi JI, Kim MS, Cho EY, Kim YG, Lee KN, et al. Trends in the use of implantable cardioverter-defibrillators for prevention of sudden cardiac arrest: A South Korean nationwide population-based study. Pacing Clin Electrophysiol. 2019; 42(8):1086–1094. PMID: 31197835.
Article23. Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003; 138(4):288–298. PMID: 12585826.
Article24. Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003; 138(4):273–287. PMID: 12585825.
Article25. Matlock DD, Peterson PN, Heidenreich PA, Lucas FL, Malenka DJ, Wang Y, et al. Regional variation in the use of implantable cardioverter-defibrillators for primary prevention: results from the national cardiovascular data registry. Circ Cardiovasc Qual Outcomes. 2011; 4(1):114–121. PMID: 21139094.26. Gupta A, Gholami P, Turakhia MP, Friday K, Heidenreich PA. Clinical reminders to providers of patients with reduced left ventricular ejection fraction increase defibrillator referral: a randomized trial. Circ Heart Fail. 2014; 7(1):140–145. PMID: 24319096.27. Kim YH, Kim JS. Clinical characteristics in patients with implantable cardioverter-defibrillator (ICD). Korean Circ J. 2004; 34(4):395–404.28. Park KH, Lee CH, Jung BC, Cho Y, Bae MH, Kim YN, et al. Effectiveness of implantable cardioverter-defibrillator therapy for heart failure patients according to ischemic or non-ischemic etiology in Korea. Korean Circ J. 2017; 47(1):72–81. PMID: 28154594.
Article29. Uhm JS, Kim TH, Kim IC, Park YA, Shin DG, Lim YM, et al. Long-term prognosis of patients with an implantable cardioverter-defibrillator in Korea. Yonsei Med J. 2017; 58(3):514–520. PMID: 28332355.
Article30. Yang JH, Byeon K, Yim HR, Park JW, Park SJ, Huh J, et al. Predictors and clinical impact of inappropriate implantable cardioverter-defibrillator shocks in Korean patients. J Korean Med Sci. 2012; 27(6):619–624. PMID: 22690092.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transvenous Implantation of an Implantable Cardioverter Defibrillator in a Patient Who Had Undergone Tricuspid Valve Replacement
- Implantable cardioverter defibrillator as a treatment for massive left ventricular fibroma-induced ventricular arrhythmia in a child
- A Case Report of the Patient Implanted with Automatic Implantable Cardioverter Defibrillator (AICD) Subject to 3rd Molar Extraction using Target Controlled Infusion of Propofol and Remifentanil: A Case Report
- Implantable Cardioverter-Defibrillator and Cardiac Resynchronization Therapy
- Implantable Cardioverter-Defibrillator of Korean Patients in a Single Center Registry