Ann Surg Treat Res.
2020 Dec;99(6):362-369. 10.4174/astr.2020.99.6.362.
A course on endovascular training for resuscitative endovascular balloon occlusion of the aorta: a pilot study for residents and specialists
- Affiliations
-
- 1Department of Trauma Surgery, Trauma Center, Dankook University Hospital, Cheonan, Korea
- 2Department of Trauma Surgery, Wonkwang University Hospital, Iksan, Korea
- 3Department of Thoracic and Cardiovascular Surgery, Trauma Center, Dankook University Hospital, Cheonan, Korea
- KMID: 2508936
- DOI: http://doi.org/10.4174/astr.2020.99.6.362
Abstract
- Purpose
Resuscitative endovascular balloon occlusion of the aorta (REBOA) has emerged as a salvage technique changing the paradigm in the management of noncompressible torso hemorrhage. However, training for the REBOA procedure is rarely performed. The endovascular training for REBOA (ET-REBOA) course was conducted to develop the endovascular skills of participants.
Methods
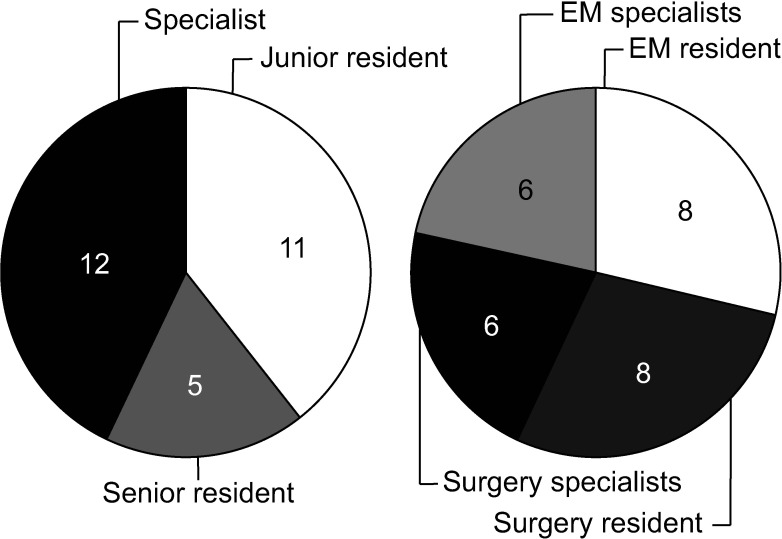
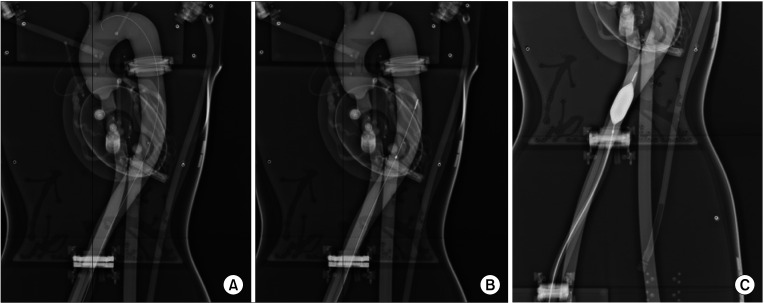
Sixteen residents and 12 specialists participated in this educational course. All participants were provided with precourse learning materials. The ET-REBOA course consisted of 2 sections; an ultrasound-guided sheath insertion on the puncture model, and a balloon manipulation on the vascular circuit model. A 13-item procedure checklist and the time required to perform the procedure were examined. Pre/post self-reported confidence score and course satisfaction questionnaire were obtained.
Results
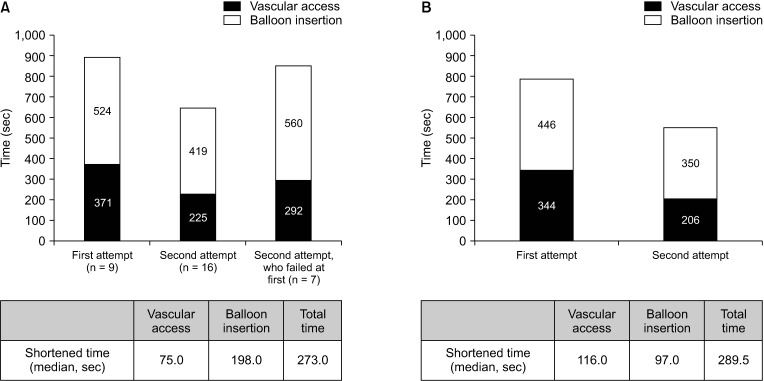
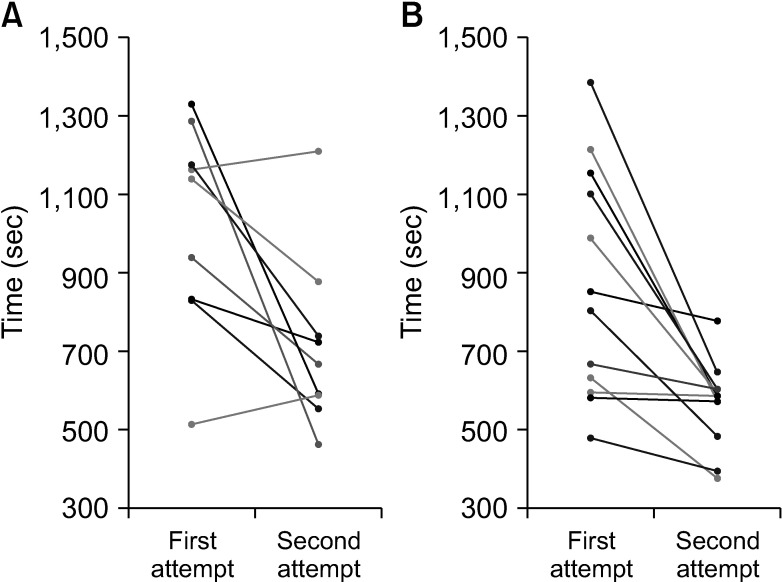
Twenty-eight participants performed the 56 REBOA procedures. On the first attempt, the median total time for REBOA from ultrasound-guided vascular access to balloon inflation was 1,139 ± 250 seconds in the resident group and 828 ± 280 seconds in the specialist group. The median shortened time for completion was 273 seconds and 290 seconds respectively. A significant decrease in procedure task time was observed between first and second attempts in the resident group (P = 0.016), specialist group (P = 0.004), and in total among all participants (P < 0.001).
Conclusion
The ET-REBOA course significantly decreased the time taken to perform the REBOA procedure with high satisfaction of the participants. The course could be an effective curriculum for the development of endovascular skills for performing REBOA.
Keyword
Figure
Cited by 1 articles
-
Comments on “A course on endovascular training for resuscitative endovascular balloon occlusion of the aorta: a pilot study for residents and specialists”
Morten Engberg, Mikkel Taudorf, Lene Russell, Lars Konge, Lars Lönn
Ann Surg Treat Res. 2021;101(2):129-130. doi: 10.4174/astr.2021.101.2.129.
Reference
-
1. Sim J, Lee J, Lee JC, Heo Y, Wang H, Jung K. Risk factors for mortality of severe trauma based on 3 years' data at a single Korean institution. Ann Surg Treat Res. 2015; 89:215–219. PMID: 26448920.2. Andres J, Scott J, Giannoudis PV. Resuscitative endovascular balloon occlusion of the aorta (REBOA): what have we learned? Injury. 2016; 47:2603–2605. PMID: 27817883.3. Belenkiy SM, Batchinsky AI, Rasmussen TE, Cancio LC. Resuscitative endovascular balloon occlusion of the aorta for hemorrhage control: past, present, and future. J Trauma Acute Care Surg. 2015; 79(4 Suppl 2):S236–S242. PMID: 26406436.4. Seamon MJ, Haut ER, Van Arendonk K, Barbosa RR, Chiu WC, Dente CJ, et al. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015; 79:159–173. PMID: 26091330.5. Kim DH, Chang SW, Matsumoto J. The utilization of resuscitative endovascular balloon occlusion of the aorta: preparation, technique, and the implementation of a novel approach to stabilizing hemorrhage. J Thorac Dis. 2018; 10:5550–5559. PMID: 30416806.6. Sadeghi M, Nilsson KF, Larzon T, Pirouzram A, Toivola A, Skoog P, et al. The use of aortic balloon occlusion in traumatic shock: first report from the ABO trauma registry. Eur J Trauma Emerg Surg. 2018; 44:491–501. PMID: 28801841.7. Saito N, Matsumoto H, Yagi T, Hara Y, Hayashida K, Motomura T, et al. Evaluation of the safety and feasibility of resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2015; 78:897–903. PMID: 25909407.8. Moore LJ, Brenner M, Kozar RA, Pasley J, Wade CE, Baraniuk MS, et al. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg. 2015; 79:523–530. discussion 530-2. PMID: 26402524.9. Villamaria CY, Eliason JL, Napolitano LM, Stansfield RB, Spencer JR, Rasmussen TE. Endovascular Skills for Trauma and Resuscitative Surgery (ESTARS) course: curriculum development, content validation, and program assessment. J Trauma Acute Care Surg. 2014; 76:929–935. discussion 935-6. PMID: 24662854.10. Brenner M, Hoehn M, Pasley J, Dubose J, Stein D, Scalea T. Basic endovascular skills for trauma course: bridging the gap between endovascular techniques and the acute care surgeon. J Trauma Acute Care Surg. 2014; 77:286–291. PMID: 25058255.11. Qasim Z, Brenner M, Menaker J, Scalea T. Resuscitative endovascular balloon occlusion of the aorta. Resuscitation. 2015; 96:275–279. PMID: 26386370.12. Gamberini E, Coccolini F, Tamagnini B, Martino C, Albarello V, Benni M, et al. Resuscitative endovascular balloon occlusion of the aorta in trauma: a systematic review of the literature. World J Emerg Surg. 2017; 12:42. PMID: 28855960.13. Morrison JJ, Galgon RE, Jansen JO, Cannon JW, Rasmussen TE, Eliason JL. A systematic review of the use of resuscitative endovascular balloon occlusion of the aorta in the management of hemorrhagic shock. J Trauma Acute Care Surg. 2016; 80:324–334. PMID: 26816219.14. King DR. Initial care of the severely injured patient. N Engl J Med. 2019; 380:763–770. PMID: 30786189.15. Ihm J, Choi H, Roh S. Flipped-learning course design and evaluation through student self-assessment in a predental science class. Korean J Med Educ. 2017; 29:93–100. PMID: 28597872.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comments on “A course on endovascular training for resuscitative endovascular balloon occlusion of the aorta: a pilot study for residents and specialists”
- Educational Simulation Videos for Performing Resuscitative Endovascular Balloon Occlusion of the Aorta
- Analysis of procedural performance after a pilot course on endovascular training for resuscitative endovascular balloon occlusion of the aorta
- Positioning of Resuscitative Endovascular Balloon Occlusion of the Aorta Catheter: A Case of an Elderly Patient with Concomitant Chest and Pelvic Injury after Blunt Trauma
- Transsplenic Ultrasound-Guided Balloon Positioning During a Zone 1 Resuscitative Endovascular Balloon Occlusion of the Aorta: A Case Report