Ann Surg Treat Res.
2020 Dec;99(6):352-361. 10.4174/astr.2020.99.6.352.
The efficacy of the “no zone” approach for the assessment of traumatic neck injury: a case-control study
- Affiliations
-
- 1Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Regional Trauma Center, Wonju Severance Christian Hospital, Wonju, Korea
- 3Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2508935
- DOI: http://doi.org/10.4174/astr.2020.99.6.352
Abstract
- Purpose
Recently, several studies have demonstrated symptom-based, non-zonal algorithms for approaching penetrating neck injuries. The purpose of this study was to confirm the effectiveness of the “no zone” approach in traumatic neck injuries.
Methods
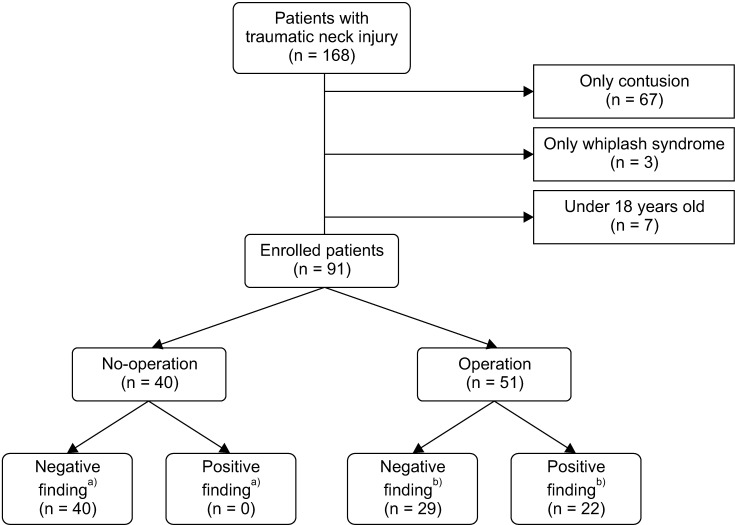
Medical charts of patients with traumatic neck injuries who presented at the Regional Trauma Center in South Korea between January 2014 and December 2018 were retrospectively reviewed. Negative final neck findings (FNFs) were compared with positive FNFs (which include major vascular, aerodigestive, nerve, endocrine gland, cartilage, or hyoid bone injuries) using multivariate logistic regression analysis including values of the “zone” and/or no zone approach.
Results
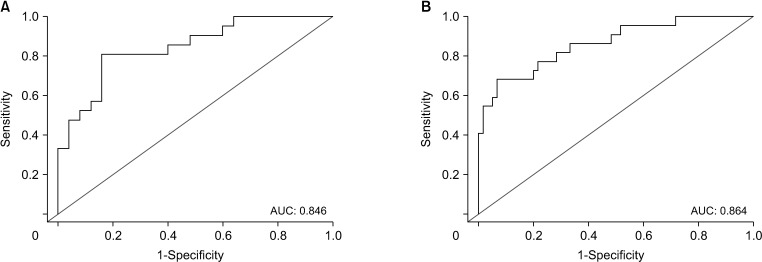
Out of 168 trauma patients, 70 patients with a minor injury and 7 patients under the age of 18 years were excluded. Of the remaining 91 patients, 74 (81.3%) had penetrating neck injuries and 17 (18.7%) had blunt neck injuries. Initial diagnosis most frequently revealed external wounds in zone II (84.6%). Twenty (22.0%) and 36 (39.5%) patients had hard and soft signs, respectively, using the no zone approach. Further, there was a significant difference between the negative and positive FNFs in patients with hard signs (11.6% vs. 54.5%; P < 0.01, respectively). According to the multivariate logistic regression analysis, the hard signs were associated with an odds ratio (OR) for FNFs (OR, 18.92; 95% confidence interval, 3.55–157.60).
Conclusion
Traumatic neck injuries classified as having hard signs based on the no zone approach may be correlated with internal organ injuries of the neck.
Keyword
Figure
Reference
-
1. Vishwanatha B, Sagayaraj A, Huddar SG, Kumar P, Datta RK. Penetrating neck injuries. Indian J Otolaryngol Head Neck Surg. 2007; 59:221–224. PMID: 23120437.2. Saito N, Hito R, Burke PA, Sakai O. Imaging of penetrating injuries of the head and neck:current practice at a level I trauma center in the United States. Keio J Med. 2014; 63:23–33. PMID: 24965876.3. Verdonck P, de Schoutheete JC, Monsieurs KG, Van Laer C, Vander Poorten V, Vanderveken O. Penetrating and blunt trauma to the neck: clinical presentation, assessment and emergency management. B-ENT. 2016; Suppl 26:69–85.4. Tessler RA, Nguyen H, Newton C, Betts J. Pediatric penetrating neck trauma: hard signs of injury and selective neck exploration. J Trauma Acute Care Surg. 2017; 82:989–994. PMID: 28521330.5. Demetriades D, Theodorou D, Cornwell E, Berne TV, Asensio J, Belzberg H, et al. Evaluation of penetrating injuries of the neck: prospective study of 223 patients. World J Surg. 1997; 21:41–48. PMID: 8943176.6. Bell RB, Osborn T, Dierks EJ, Potter BE, Long WB. Management of penetrating neck injuries: a new paradigm for civilian trauma. J Oral Maxillofac Surg. 2007; 65:691–705. PMID: 17368366.7. Sim J, Lee J, Lee JC, Heo Y, Wang H, Jung K. Risk factors for mortality of severe trauma based on 3 years' data at a single Korean institution. Ann Surg Treat Res. 2015; 89:215–219. PMID: 26448920.8. Mahmoodie M, Sanei B, Moazeni-Bistgani M, Namgar M. Penetrating neck trauma: review of 192 cases. Arch Trauma Res. 2012; 1:14–18. PMID: 24719835.9. Monson DO, Saletta JD, Freeark RJ. Carotid vertebral trauma. J Trauma. 1969; 9:987–999. PMID: 4902214.10. Shiroff AM, Gale SC, Martin ND, Marchalik D, Petrov D, Ahmed HM, et al. Penetrating neck trauma: a review of management strategies and discussion of the ‘No Zone’ approach. Am Surg. 2013; 79:23–29. PMID: 23317595.11. Ibraheem K, Khan M, Rhee P, Azim A, O'Keeffe T, Tang A, et al. “No zone” approach in penetrating neck trauma reduces unnecessary computed tomography angiography and negative explorations. J Surg Res. 2018; 221:113–120. PMID: 29229116.12. Schroll R, Fontenot T, Lipcsey M, Heaney JB, Marr A, Meade P, et al. Role of computed tomography angiography in the management of Zone II penetrating neck trauma in patients with clinical hard signs. J Trauma Acute Care Surg. 2015; 79:943–950. PMID: 26317813.13. Sperry JL, Moore EE, Coimbra R, Croce M, Davis JW, Karmy-Jones R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg. 2013; 75:936–940. PMID: 24256663.14. Low GM, Inaba K, Chouliaras K, Branco B, Lam L, Benjamin E, et al. The use of the anatomic ‘zones’ of the neck in the assessment of penetrating neck injury. Am Surg. 2014; 80:970–974. PMID: 25264641.15. Inaba K, Branco BC, Menaker J, Scalea TM, Crane S, DuBose JJ, et al. Evaluation of multidetector computed tomography for penetrating neck injury: a prospective multicenter study. J Trauma Acute Care Surg. 2012; 72:576–584. PMID: 22491539.16. Prichayudh S, Choadrachata-anun J, Sriussadaporn S, Pak-art R, Sriussadaporn S, Kritayakirana K, et al. Selective management of penetrating neck injuries using “no zone” approach. Injury. 2015; 46:1720–1725. PMID: 26117413.17. Hundersmarck D, Reinders Folmer E, de Borst GJ, Leenen LP, Vriens PW, Hietbrink F. Penetrating neck injury in two Dutch level 1 trauma centres: the non-existent problem. Eur J Vasc Endovasc Surg. 2019; 58:455–462. PMID: 31307866.18. Nowicki JL, Stew B, Ooi E. Penetrating neck injuries: a guide to evaluation and management. Ann R Coll Surg Engl. 2018; 100:6–11. PMID: 29046084.19. Babu A, Garg H, Sagar S, Gupta A, Kumar S. Penetrating neck injury: collaterals for another life after ligation of common carotid artery and subclavian artery. Chin J Traumatol. 2017; 20:56–58. PMID: 28233726.20. Burgess CA, Dale OT, Almeyda R, Corbridge RJ. An evidence based review of the assessment and management of penetrating neck trauma. Clin Otolaryngol. 2012; 37:44–52. PMID: 22152036.21. Siau RT, Moore A, Ahmed T, Lee MS, Tostevin P. Management of penetrating neck injuries at a London trauma centre. Eur Arch Otorhinolaryngol. 2013; 270:2123–2128. PMID: 23263269.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of the Zone III Neck Injury by Impalement of a Metal Stick
- One Case of Traumatic Pericallosal Artery Aneurysm: A Case Report
- The Diagnostic Value of MRI in Traumatic Brachial Plexus Injury
- Computerized Assessment of Neurocognitive function for Traumatic Brain Injury Patients
- Central Pain Due to Traumatic Axonal Injury of the Spinothalamic Tract in Patients with Mild Traumatic Brain Injury