Ann Hepatobiliary Pancreat Surg.
2020 Nov;24(4):477-483. 10.14701/ahbps.2020.24.4.477.
National survey of Korean hepatobiliary-pancreatic surgeons on attitudes about the enhanced recovery after surgery protocol
- Affiliations
-
- 1Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Liver Transplantation and Hepatobiliary Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea
- 4Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 5Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- 6Department of Surgery, Inje University College of Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea
- KMID: 2508857
- DOI: http://doi.org/10.14701/ahbps.2020.24.4.477
Abstract
- Backgrounds/Aims
The purpose of this study was to investigate attitudes regarding the Enhanced Recovery After Surgery (ERAS) protocol of hepato-biliary-pancreatic (HBP) surgeons in Korea and the extent to which they use the protocol for perioperative management.
Methods
An online survey was conducted among members of the Korean Association of Hepato-Biliary-Pancreatic Surgery (KAHBPS) for eight weeks beginning on August 2019. The questionnaire, which was written in Korean, was based on the latest ERAS guidelines. Total responses were collected from 127 surgeons.
Results
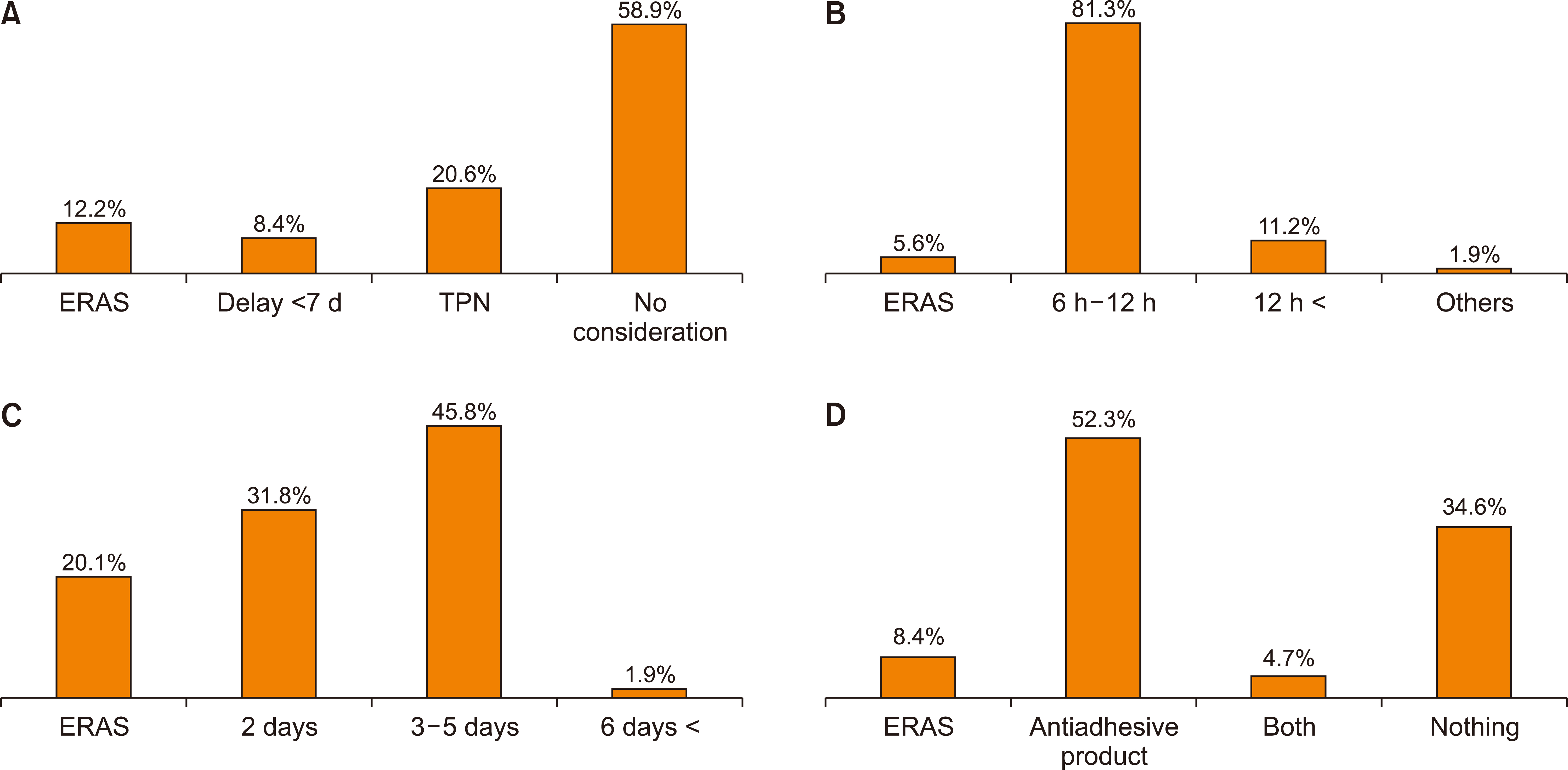
Of the 127 total respondents, the largest proportion (44.9%) were working in Seoul. In terms of established in-hospital clinical pathways (CP), 19.7% of the participating surgeons had and followed a CP in pancreaticoduodenectomy (PD) and 21.3% in hepatectomy. Regarding the ERAS protocol for each surgery, four items (18.2%) regarding PD and seven items (35.0%) related to hepatectomy were followed by more than 50% of respondents.
Conclusions
ERAS guidelines are one of the consensuses for better recovery in perioperative management of patients undergoing major surgeries and encompass the overall process of patient recovery including patient education, pain control, physiologic balance, and perioperative nutrition. A novel project is needed to successfully implement an evidence-based enhanced recovery strategy.
Keyword
Figure
Cited by 2 articles
-
Effect of early oral nutrition supplement using Encover in patients undergoing hepato-biliary-pancreatic surgery
Byeong Jun Lee, Joon Seong Park, Hyung Sun Kim, Dong Sup Yoon, Jin Hong Lim
Int J Stem Cells. 2022;26(3):244-250. doi: 10.14701/ahbps.21-152.Challenging issues of implementing enhanced recovery after surgery programs in South Korea
Soo-Hyuk Yoon, Ho-Jin Lee
Anesth Pain Med. 2024;19(1):24-34. doi: 10.17085/apm.23096.
Reference
-
1. Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. 1995; Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet. 345:763–764. DOI: 10.1016/S0140-6736(95)90643-6. PMID: 7891489.
Article2. Kehlet H, Mogensen T. 1999; Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 86:227–230. DOI: 10.1046/j.1365-2168.1999.01023.x. PMID: 10100792.
Article3. Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. 2012; Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERASⓇ) Society recommendations. Clin Nutr. 31:817–830. DOI: 10.1016/j.clnu.2012.08.011. PMID: 23079762.4. Melloul E, Hübner M, Scott M, Snowden C, Prentis J, Dejong CH, et al. 2016; Guidelines for perioperative care for liver surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg. 40:2425–2440. DOI: 10.1007/s00268-016-3700-1. PMID: 27549599.
Article5. Ljungqvist O, Scott M, Fearon KC. 2017; Enhanced recovery after surgery: a review. JAMA Surg. 152:292–298. DOI: 10.1001/jamasurg.2016.4952. PMID: 28097305.6. Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J. 2011; Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 146:571–577. DOI: 10.1001/archsurg.2010.309. PMID: 21242424.7. Savikko J, Ilmakunnas M, Mäkisalo H, Nordin A, Isoniemi H. 2015; Enhanced recovery protocol after liver resection. Br J Surg. 102:1526–1532. DOI: 10.1002/bjs.9912. PMID: 26331595.
Article8. Rouxel P, Beloeil H. 2019; Enhanced recovery after hepatectomy: a systematic review. Anaesth Crit Care Pain Med. 38:29–34. DOI: 10.1016/j.accpm.2018.05.003. PMID: 29807132.
Article9. Hwang DW, Kim HJ, Lee JH, Song KB, Kim MH, Lee SK, et al. 2019; Effect of Enhanced Recovery After Surgery program on pancreaticoduodenectomy: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 26:360–369. DOI: 10.1002/jhbp.641. PMID: 31152686.
Article10. Buhrman WC, Lyman WB, Kirks RC, Passeri M, Vrochides D. 2018; Current state of Enhanced Recovery After Surgery in hepatopancreatobiliary surgery. J Laparoendosc Adv Surg Tech A. 28:1471–1475. DOI: 10.1089/lap.2018.0314. PMID: 29924662.
Article11. Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, et al. 2013; Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERASⓇ) Society recommendations. World J Surg. 37:240–258. DOI: 10.1007/s00268-012-1771-1. PMID: 22956014.12. Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. 2000; Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 232:786–795. DOI: 10.1097/00000658-200012000-00007. PMID: 11088073. PMCID: PMC1421271.
Article13. Sohn TA, Yeo CJ, Cameron JL, Koniaris L, Kaushal S, Abrams RA, et al. 2000; Resected adenocarcinoma of the pancreas-616 patients: results, outcomes, and prognostic indicators. J Gastrointest Surg. 4:567–579. DOI: 10.1016/S1091-255X(00)80105-5. PMID: 11307091.
Article14. Shin SH, Kim SC, Song KB, Hwang DW, Lee JH, Park KM, et al. 2018; Chronologic changes in clinical and survival features of pancreatic ductal adenocarcinoma since 2000: a single-center experience with 2,029 patients. Surgery. 164:432–442. DOI: 10.1016/j.surg.2018.04.017. PMID: 29884479.
Article15. Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. 2002; Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 236:397–406. discussion 406-407. DOI: 10.1097/00000658-200210000-00001. PMID: 12368667. PMCID: PMC1422593.16. Aloia TA, Fahy BN, Fischer CP, Jones SL, Duchini A, Galati J, et al. 2009; Predicting poor outcome following hepatectomy: analysis of 2313 hepatectomies in the NSQIP database. HPB (Oxford). 11:510–515. DOI: 10.1111/j.1477-2574.2009.00095.x. PMID: 19816616. PMCID: PMC2756639.
Article17. Zimmitti G, Roses RE, Andreou A, Shindoh J, Curley SA, Aloia TA, et al. 2013; Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg. 17:57–64. discussion 64-65. DOI: 10.1007/s11605-012-2000-9. PMID: 22956403. PMCID: PMC3855461.
Article18. Jones C, Kelliher L, Dickinson M, Riga A, Worthington T, Scott MJ, et al. 2013; Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg. 100:1015–1024. DOI: 10.1002/bjs.9165. PMID: 23696477.
Article19. Schultz NA, Larsen PN, Klarskov B, Plum LM, Frederiksen HJ, Christensen BM, et al. 2013; Evaluation of a fast-track programme for patients undergoing liver resection. Br J Surg. 100:138–143. DOI: 10.1002/bjs.8996. PMID: 23165484.
Article20. Braga M, Pecorelli N, Ariotti R, Capretti G, Greco M, Balzano G, et al. 2014; Enhanced recovery after surgery pathway in patients undergoing pancreaticoduodenectomy. World J Surg. 38:2960–2966. DOI: 10.1007/s00268-014-2653-5. PMID: 24870390.
Article21. Coolsen MM, van Dam RM, Chigharoe A, Olde Damink SW, Dejong CH. 2014; Improving outcome after pancreaticoduodenectomy: experiences with implementing an enhanced recovery after surgery (ERAS) program. Dig Surg. 31:177–184. DOI: 10.1159/000363583. PMID: 25097014.
Article22. Williamsson C, Karlsson N, Sturesson C, Lindell G, Andersson R, Tingstedt B. 2015; Impact of a fast-track surgery programme for pancreaticoduodenectomy. Br J Surg. 102:1133–1141. DOI: 10.1002/bjs.9856. PMID: 26042725.
Article23. Lavu H, Kennedy EP, Mazo R, Stewart RJ, Greenleaf C, Grenda DR, et al. 2010; Preoperative mechanical bowel preparation does not offer a benefit for patients who undergo pancreaticoduodenectomy. Surgery. 148:278–284. DOI: 10.1016/j.surg.2010.03.012. PMID: 20447669.
Article24. Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. 2013; A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg. 216:1–14. DOI: 10.1016/j.jamcollsurg.2012.09.002. PMID: 23122535.
Article25. McMillan MT, Malleo G, Bassi C, Butturini G, Salvia R, Roses RE, et al. 2015; Drain management after pancreatoduodenectomy: reappraisal of a prospective randomized trial using risk stratification. J Am Coll Surg. 221:798–809. DOI: 10.1016/j.jamcollsurg.2015.07.005. PMID: 26278037.
Article26. Ljungqvist O, Søreide E. 2003; Preoperative fasting. Br J Surg. 90:400–406. DOI: 10.1002/bjs.4066. PMID: 12673740.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perception and implementation status of enhanced recovery after surgery
- Which patients with gastric cancer should be candidates for Enhanced Recovery After Surgery protocols?
- ERAS in minimally invasive hepatectomy
- Enhanced recovery after surgery: operation-related factors
- Predictive value of post-operative drain amylase levels for post-operative pancreatic fistula