J Korean Med Sci.
2020 Nov;35(45):e369. 10.3346/jkms.2020.35.e369.
The Prevalence of Sjögren's Syndrome in Rheumatoid Arthritis Patients and Their Clinical Features
- Affiliations
-
- 1Department of Rheumatology, Hanyang University Hospital for Rheumatic Diseases, Seoul, Korea
- 2Department of Ophthalmology, Hanyang University Hospital, Hanyang University College of Medicine, Seoul, Korea
- 3Division of Oral & Maxillofacial Surgery, Department of Dentistry, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2508800
- DOI: http://doi.org/10.3346/jkms.2020.35.e369
Abstract
- Background
To estimate the prevalence of Sjögren's syndrome (SS) in patients with rheumatoid arthritis (RA) and to compare the clinical features of RA patients with and without SS.
Methods
We conducted a retrospective study of RA patients who visited a rheumatology clinic in a tertiary referral hospital in Korea between May 20 and July 22, 2016. All patients fulfilled the classification criteria for RA, and the diagnosis of SS was made clinically by rheumatologists and according to the 2002 American-European Consensus Group (AECG), 2012 American College of Rheumatology (ACR), and 2016 ACR/European League Against Rheumatism (EULAR) classification criteria. The prevalence was estimated as the number of SS patients within the total number of RA patients. The disease activity and treatment pattern of RA were compared between patients with and without SS.
Results
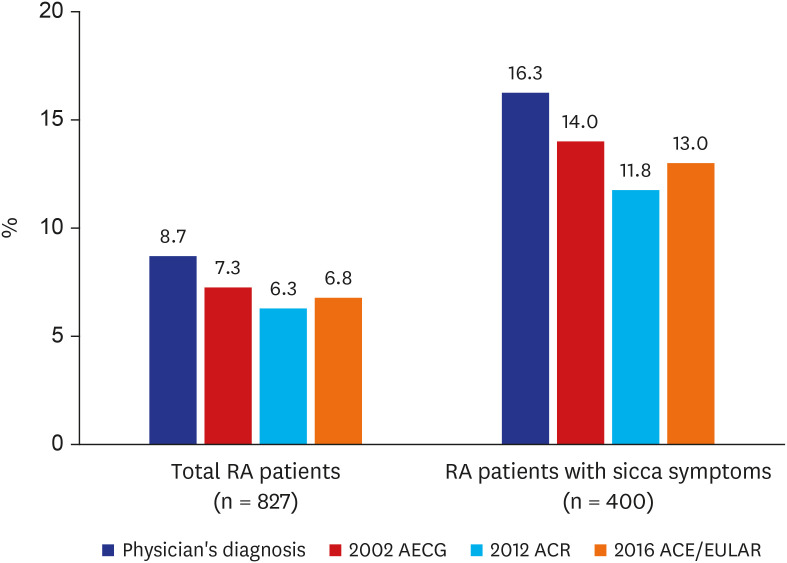
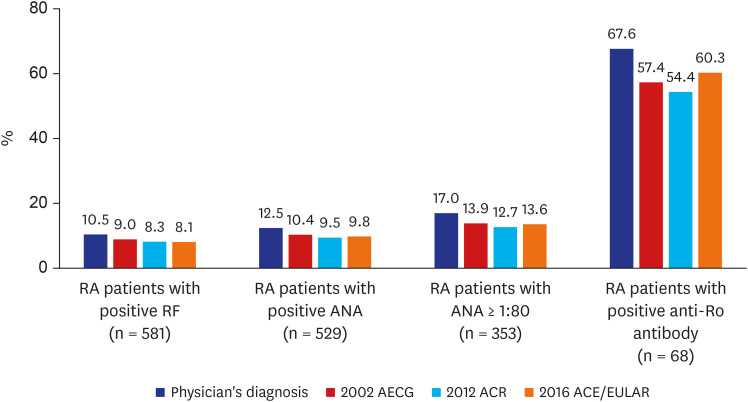
Among 827 RA patients, 72 patients (8.7%) were diagnosed with SS by a rheumatologist, though only 60 patients (7.3%) satisfied the 2002 AECG classification criteria for SS. Fifty-two patients (6.3%) and 56 patients (6.8%) fulfilled the 2012 ACR and 2016 ACR/EULAR classification criteria, respectively. The prevalence of SS in RA patients was 10.5%, 17.0%, and 67.6% in rheumatoid factor, antinuclear antibody (≥ 1:80), and anti-Ro antibody positive patients, respectively.
Conclusion
The prevalence of SS among RA patients was 8.7% according to rheumatologists' diagnosis. The presence of SS did not affect the treatment patterns of RA patients. However, the autoantibody profiles and demographics of RA patients with SS differed from those of patients without SS.
Figure
Cited by 1 articles
-
Epidemiology of Rheumatoid Arthritis in Korea
Hyoungyoung Kim, Yoon-Kyoung Sung
J Rheum Dis. 2021;28(2):60-67. doi: 10.4078/jrd.2021.28.2.60.
Reference
-
1. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61(6):554–558. PMID: 12006334.2. Voulgarelis M, Dafni UG, Isenberg DA, Moutsopoulos HM. Malignant lymphoma in primary Sjögren's syndrome: a multicenter, retrospective, clinical study by the European Concerted Action on Sjögren's Syndrome. Arthritis Rheum. 1999; 42(8):1765–1772. PMID: 10446879.
Article3. Manoussakis MN, Georgopoulou C, Zintzaras E, Spyropoulou M, Stavropoulou A, Skopouli FN, et al. Sjögren's syndrome associated with systemic lupus erythematosus: clinical and laboratory profiles and comparison with primary Sjögren's syndrome. Arthritis Rheum. 2004; 50(3):882–891. PMID: 15022331.
Article4. Gilboe IM, Kvien TK, Uhlig T, Husby G. Sicca symptoms and secondary Sjögren's syndrome in systemic lupus erythematosus: comparison with rheumatoid arthritis and correlation with disease variables. Ann Rheum Dis. 2001; 60(12):1103–1109. PMID: 11709451.5. Nossent JC, Swaak AJ. Systemic lupus erythematosus VII: frequency and impact of secondary Sjøgren's syndrome. Lupus. 1998; 7(4):231–234. PMID: 9643312.6. Alani H, Henty JR, Thompson NL, Jury E, Ciurtin C. Systematic review and meta-analysis of the epidemiology of polyautoimmunity in Sjögren's syndrome (secondary Sjögren's syndrome) focusing on autoimmune rheumatic diseases. Scand J Rheumatol. 2018; 47(2):141–154. PMID: 28927315.
Article7. Brown LE, Frits ML, Iannaccone CK, Weinblatt ME, Shadick NA, Liao KP. Clinical characteristics of RA patients with secondary SS and association with joint damage. Rheumatology (Oxford). 2015; 54(5):816–820. PMID: 25313147.
Article8. He J, Ding Y, Feng M, Guo J, Sun X, Zhao J, et al. Characteristics of Sjögren's syndrome in rheumatoid arthritis. Rheumatology (Oxford). 2013; 52(6):1084–1089. PMID: 23382356.9. Martens PB, Pillemer SR, Jacobsson LT, O'Fallon WM, Matteson EL. Survivorship in a population based cohort of patients with Sjögren's syndrome, 1976-1992. J Rheumatol. 1999; 26(6):1296–1300. PMID: 10381046.10. Turesson C, O'Fallon WM, Crowson CS, Gabriel SE, Matteson EL. Occurrence of extraarticular disease manifestations is associated with excess mortality in a community based cohort of patients with rheumatoid arthritis. J Rheumatol. 2002; 29(1):62–67. PMID: 11824973.11. Kim SM, Park E, Lee JH, Lee SH, Kim HR. The clinical significance of anti-cyclic citrullinated peptide antibody in primary Sjögren syndrome. Rheumatol Int. 2012; 32(12):3963–3967. PMID: 22205381.
Article12. Lee J, Koh JH, Kim JW, Sung YK, Lee SS, Choe JY, et al. Performance of the 2016 ACR-EULAR classification criteria for primary Sjogren's syndrome in a Korean cohort. Rheumatol Int. 2018; 38(9):1651–1660. PMID: 30030624.
Article13. Shiboski SC, Shiboski CH, Criswell L, Baer A, Challacombe S, Lanfranchi H, et al. American College of Rheumatology classification criteria for Sjögren's syndrome: a data-driven, expert consensus approach in the Sjögren's International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken). 2012; 64(4):475–487. PMID: 22563590.
Article14. Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren's syndrome: a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis. 2017; 76(1):9–16. PMID: 27789466.15. Haga HJ, Naderi Y, Moreno AM, Peen E. A study of the prevalence of sicca symptoms and secondary Sjögren's syndrome in patients with rheumatoid arthritis, and its association to disease activity and treatment profile. Int J Rheum Dis. 2012; 15(3):284–288. PMID: 22709490.
Article16. Calgüneri M, Ureten K, Akif Oztürk M, Onat AM, Ertenli I, Kiraz S, et al. Extra-articular manifestations of rheumatoid arthritis: results of a university hospital of 526 patients in Turkey. Clin Exp Rheumatol. 2006; 24(3):305–308. PMID: 16870099.17. Cimmino MA, Salvarani C, Macchioni P, Montecucco C, Fossaluzza V, Mascia MT, et al. Extra-articular manifestations in 587 Italian patients with rheumatoid arthritis. Rheumatol Int. 2000; 19(6):213–217. PMID: 11063290.
Article18. Kim SK, Park SH, Shin IH, Choe JY. Anti-cyclic citrullinated peptide antibody, smoking, alcohol consumption, and disease duration as risk factors for extraarticular manifestations in Korean patients with rheumatoid arthritis. J Rheumatol. 2008; 35(6):995–1001. PMID: 18464311.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Manifestations Like Multiple Sclerosis in a Paitent with Rheumatoid Arthritis and Sjogren's Syndrome
- A Case of Sjogren's Syndrome with Hyperthyroidism
- Primary Extranodal Marginal Zone B-cell Lymphoma of Mucosa-Associated Lymphoid Tissue-type in the Thymus of a Patient with Sjogren's Syndrome and Rheumatoid Arthritis
- Distal renal tubular acidosis in sjogren syndrome with rheumatoid arthritis
- A Case of Rheumatoid Nodules Involving the Larynx