J Korean Med Sci.
2020 Nov;35(43):e356. 10.3346/jkms.2020.35.e356.
Practical Utility of D-dimer Test for Venous Thromboembolism in Systemic Lupus Erythematosus Depends on Disease Activity: a Retrospective Cohort Study
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Division of Rheumatology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Molecular Medicine and Biopharmaceutical Sciences, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea
- 5Wide River Institute of Immunology, Seoul National University College of Medicine, Hongcheon, Korea
- KMID: 2508498
- DOI: http://doi.org/10.3346/jkms.2020.35.e356
Abstract
- Background
The D-dimer test is a screening tool for venous thromboembolism (VTE); however, its utility for patients with systemic lupus erythematosus (SLE) remains unclear. Here, we examined the utility of the D-dimer test as a screening tool for VTE in SLE patients.
Methods
SLE patients (n = 276) and age- and sex-matched patients with non-rheumatic disease (n = 1,104), all of whom underwent D-dimer testing to screen for VTE, were enrolled. The sensitivity and specificity and receiver operating characteristics curve of the D-dimer test were compared in both groups. Then, subgroup of SLE patients in whom the D-dimer test can be useful was sought.
Results
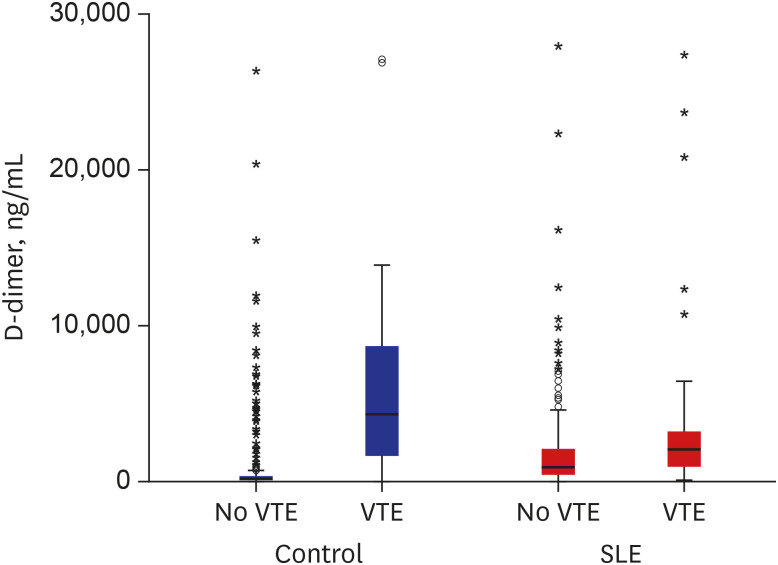
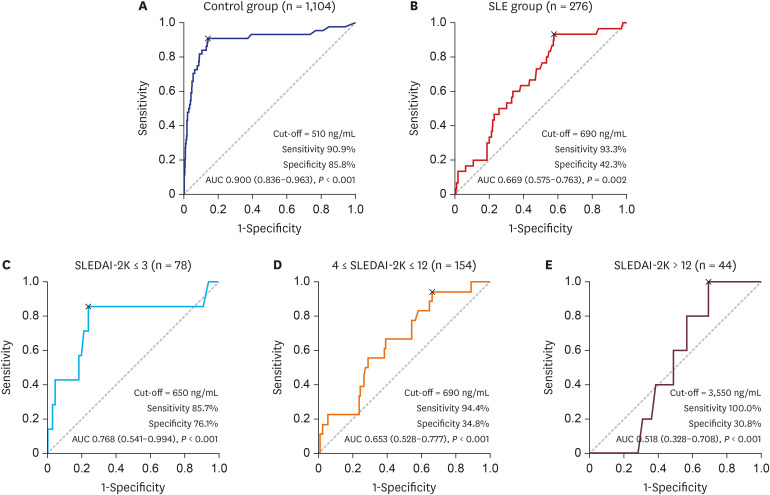
The incidence of VTE was more common in SLE patients than controls (10.9% vs. 4.0%). Although the sensitivity of the D-dimer test was comparable between SLE patients and controls (93.3% vs. 90.9%), the specificity of the test was profoundly lower in SLE patients compared to controls (28.4% vs. 84.4%). The area under the curve (AUC) of the D-dimer for VTE was 0.669 in SLE patients and 0.90 in control group. Multiple linear regression analysis demonstrated that SLE disease activity index-2000 (SLEDAI-2K) was significantly associated with D-dimer levels in SLE patients (β = 0.155; P = 0.022). Subgroup analysis showed that the AUC is moderate (0.768) with low disease activity, while it is low (0.518) with high SLEDAI-2K.
Conclusion
The D-dimer test may not be a useful screening tool for VTE in patients with active SLE. D-dimer test for predicting VTE in SLE patients should be differentially applied according to disease activity of SLE.
Figure
Reference
-
1. Tagalakis V, Patenaude V, Kahn SR, Suissa S. Incidence of and mortality from venous thromboembolism in a real-world population: the Q-VTE Study Cohort. Am J Med. 2013; 126(9):832.e13–832.e21.
Article2. Stein PD, Matta F. Epidemiology and incidence: the scope of the problem and risk factors for development of venous thromboembolism. Clin Chest Med. 2010; 31(4):611–628. PMID: 21047571.
Article3. Righini M, Robert-Ebadi H, Le Gal G. Diagnosis of acute pulmonary embolism. J Thromb Haemost. 2017; 15(7):1251–1261. PMID: 28671347.
Article4. Kline JA. Diagnosis and exclusion of pulmonary embolism. Thromb Res. 2018; 163:207–220. PMID: 28683951.
Article5. Wells PS, Ihaddadene R, Reilly A, Forgie MA. Diagnosis of venous thromboembolism: 20 years of progress. Ann Intern Med. 2018; 168(2):131–140. PMID: 29310137.
Article6. Geersing GJ, Janssen KJ, Oudega R, Bax L, Hoes AW, Reitsma JB, et al. Excluding venous thromboembolism using point of care D-dimer tests in outpatients: a diagnostic meta-analysis. BMJ. 2009; 339:b2990. PMID: 19684102.
Article7. Kabrhel C, Mark Courtney D, Camargo CA Jr, Plewa MC, Nordenholz KE, Moore CL, et al. Factors associated with positive D-dimer results in patients evaluated for pulmonary embolism. Acad Emerg Med. 2010; 17(6):589–597. PMID: 20624138.
Article8. Lee S, Hwang JI, Kim Y, Yoon PW, Ahn J, Yoo JJ. Venous thromboembolism following hip and knee replacement arthroplasty in Korea: a nationwide study based on claims registry. J Korean Med Sci. 2016; 31(1):80–88. PMID: 26770042.
Article9. Hartman EA, van Royen-Kerkhof A, Jacobs JW, Welsing PM, Fritsch-Stork RD. Performance of the 2012 Systemic Lupus International Collaborating Clinics classification criteria versus the 1997 American College of Rheumatology classification criteria in adult and juvenile systemic lupus erythematosus. A systematic review and meta-analysis. Autoimmun Rev. 2018; 17(3):316–322. PMID: 29366725.
Article10. Aviña-Zubieta JA, Vostretsova K, De Vera MA, Sayre EC, Choi HK. The risk of pulmonary embolism and deep venous thrombosis in systemic lupus erythematosus: a general population-based study. Semin Arthritis Rheum. 2015; 45(2):195–201. PMID: 26364556.
Article11. Linkins LA, Takach Lapner S. Review of D-dimer testing: good, bad, and ugly. Int J Lab Hematol. 2017; 39 Suppl 1:98–103. PMID: 28447414.
Article12. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997; 40(9):1725.
Article13. Geersing GJ, Zuithoff NP, Kearon C, Anderson DR, Ten Cate-Hoek AJ, Elf JL, et al. Exclusion of deep vein thrombosis using the Wells rule in clinically important subgroups: individual patient data meta-analysis. BMJ. 2014; 348:g1340. PMID: 24615063.
Article14. Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012; 379(9828):1835–1846. PMID: 22494827.
Article15. Lee YS, Lee YK, Han SB, Nam CH, Parvizi J, Koo KH. Natural progress of D-dimer following total joint arthroplasty: a baseline for the diagnosis of the early postoperative infection. J Orthop Surg. 2018; 13(1):36.
Article16. Righini M, Nendaz M, Le Gal G, Bounameaux H, Perrier A. Influence of age on the cost-effectiveness of diagnostic strategies for suspected pulmonary embolism. J Thromb Haemost. 2007; 5(9):1869–1877. PMID: 17596141.
Article17. Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002; 29(2):288–291. PMID: 11838846.18. Mok CC, Ho LY, Yu KL, To CH. Venous thromboembolism in southern Chinese patients with systemic lupus erythematosus. Clin Rheumatol. 2010; 29(6):599–604. PMID: 20101427.
Article19. Sarabi ZS, Chang E, Bobba R, Ibanez D, Gladman D, Urowitz M, et al. Incidence rates of arterial and venous thrombosis after diagnosis of systemic lupus erythematosus. Arthritis Rheum. 2005; 53(4):609–612. PMID: 16082635.
Article20. Zaldívar-Alcántara H, Herrera-Jiménez LE, Dehesa-López E, Correa-Rotter R. Risk factors for the development of thrombotic complication in patients with lupus erythematosus and lupus nephropatic. Rev Invest Clin. 2013; 65(3):199–208. PMID: 23877806.21. Xu J, Lupu F, Esmon CT. Inflammation, innate immunity and blood coagulation. Hamostaseologie. 2010; 30(1):5–6. 8–9. PMID: 20162248.
Article22. Lundström E, Gustafsson JT, Jönsen A, Leonard D, Zickert A, Elvin K, et al. HLA-DRB1*04/*13 alleles are associated with vascular disease and antiphospholipid antibodies in systemic lupus erythematosus. Ann Rheum Dis. 2013; 72(6):1018–1025. PMID: 22893315.
Article23. Dhillon PK, Adams MJ. Thrombosis in systemic lupus erythematosus: role of impaired fibrinolysis. Semin Thromb Hemost. 2013; 39(4):434–440. PMID: 23504607.
Article24. Meesters EW, Hansen H, Spronk HM, Hamulyak K, Rosing J, Rowshani AT, et al. The inflammation and coagulation cross-talk in patients with systemic lupus erythematosus. Blood Coagul Fibrinolysis. 2007; 18(1):21–28. PMID: 17179822.
Article25. Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000; 83(3):416–420. PMID: 10744147.
Article26. Wells PS, Owen C, Doucette S, Fergusson D, Tran H. Does this patient have deep vein thrombosis? JAMA. 2006; 295(2):199–207. PMID: 16403932.
Article27. Park R, Seo YI, Yoon SG, Choi TY, Shin JW, Uh ST, et al. Utility of D-dimer assay for diagnosing pulmonary embolism: single institute study. Korean J Lab Med. 2008; 28(6):419–424. PMID: 19127105.
Article28. Kim JY, Kim KH, Cho JY, Sim DS, Yoon HJ, Yoon NS, et al. D-dimer/troponin ratio in the differential diagnosis of acute pulmonary embolism from non-ST elevation myocardial infarction. Korean J Intern Med. 2019; 34(6):1263–1271. PMID: 30685960.29. Kim SA, Yhim HY, Bang SM. Current management of cancer-associated venous thromboembolism: focus on direct oral anticoagulants. J Korean Med Sci. 2019; 34(6):e52. PMID: 30787683.
Article30. Lozano-Polo L, Puig-Campmany M, Herrera-Mateo S, Mateo-Roca M, Santos-Rodríguez JA, Benito-Vales S. Diagnosis of pulmonary embolism in the elderly: adherence to guidelines and age-adjusted D-dimer concentration values. Emergencias. 2018; 30(5):321–327. PMID: 30260116.31. Alvarez-Perez FJ, Castelo-Branco M, Alvarez-Sabin J. Usefulness of measurement of fibrinogen, D-dimer, D-dimer/fibrinogen ratio, C reactive protein and erythrocyte sedimentation rate to assess the pathophysiology and mechanism of ischaemic stroke. J Neurol Neurosurg Psychiatry. 2011; 82(9):986–992. PMID: 21296900.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Of Systemic Lupus Erythematosus Associated With Hyperthyroidism And Severe Retinopathy
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A Case of Lupus Enteritis That Developed during the Treatment of Systemic Lupus Erythematosus
- Pulmonary Thromboendarterectomy for Chronic Thromboembolic Pulmonary Hypertension in a Patient with Antiphospholipid Syndrome and Systemic Lupus Erythematosus
- A Case of Systemic Lupus Erythematosus Diagnosed by Initial Presentation of Digital Gangrene