Anesth Pain Med.
2020 Oct;15(4):434-440. 10.17085/apm.20055.
Change of inspired oxygen concentration in low flow anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- KMID: 2508405
- DOI: http://doi.org/10.17085/apm.20055
Abstract
- Background
There are several advantages of low flow anesthesia including safety, economics, and eco-friendliness. However, oxygen concentration of fresh gas flow and inspired gas are large different in low flow anesthesia. This is a hurdle to access to low flow anesthesia. In this study, we aimed to investigate the change in inhaled oxygen concentration in low flow anesthesia using oxygen and medical air.
Methods
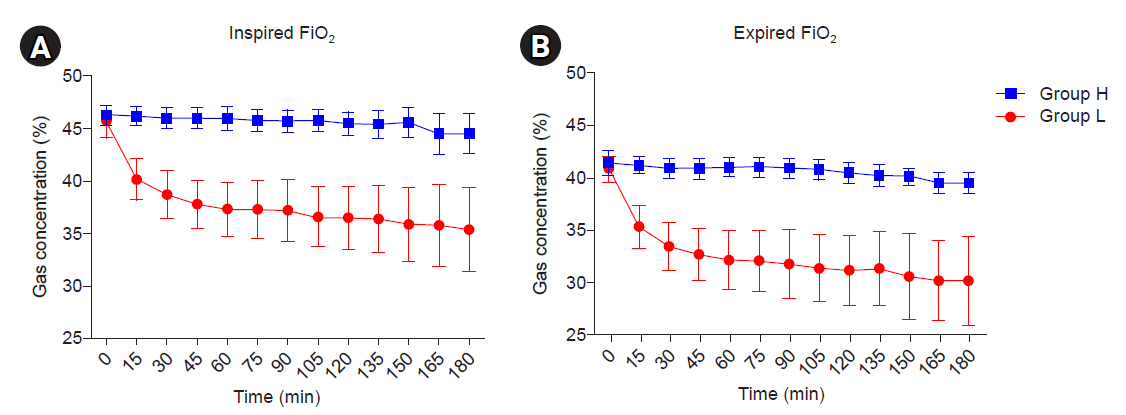
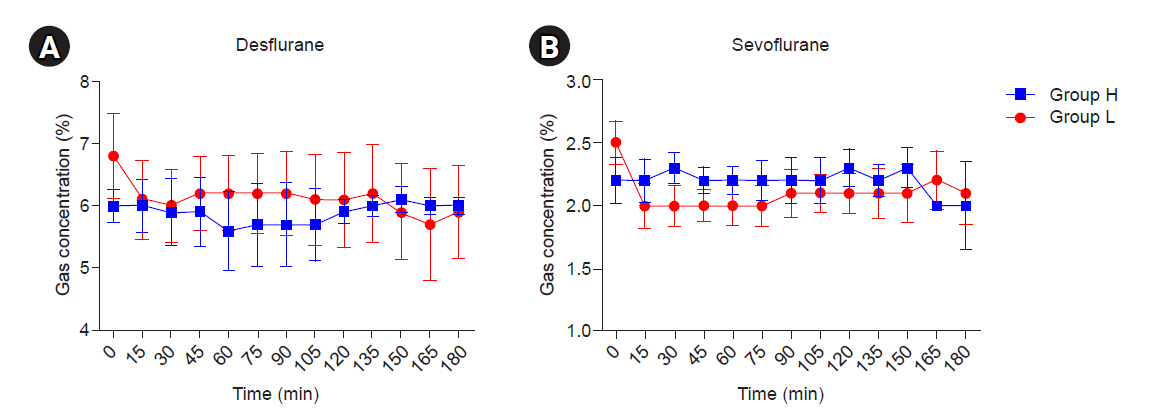
A total of 60 patients scheduled for elective surgery with an American Society of Anesthesiologist physical status I or II were enrolled and randomly allocated into two groups. Group H: Fresh gas flow rate (FGF) 4 L/min (FiO₂ 0.5). Group L: FGF 1 L/min (FiO₂ 0.5). FGF was applied 4 L/min in initial phase (10 min) after intubation. After initial phase FGF was adjusted according to groups. FGF continued at the end of surgery. Oxygen and inhalation anesthetic gas concentration were recorded for 180 min at 15 min interval.
Results
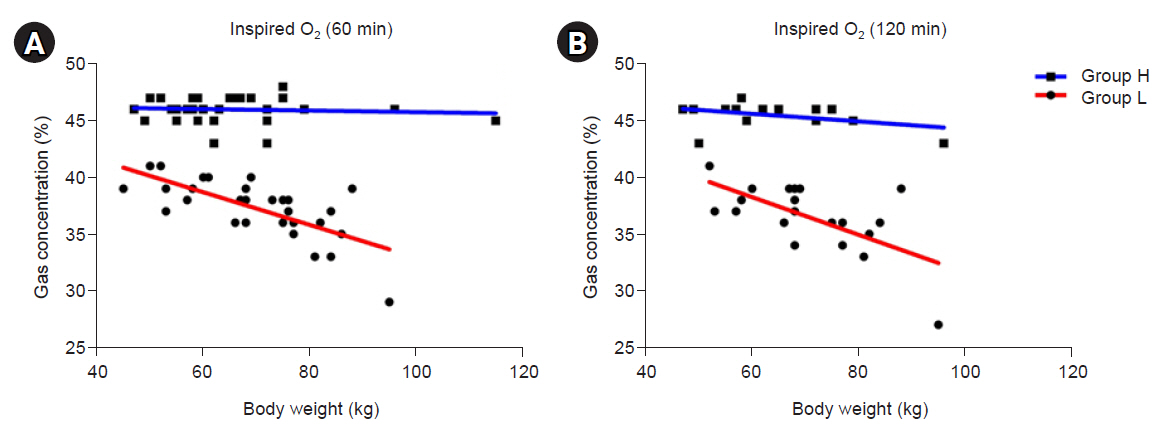
The inspired oxygen concentration decreased by 5.5% during the first 15 min in the group L. Inspired oxygen decreased by 1.5% during next 15 min. Inspired oxygen decreased by 1.4% for 30 to 60 min. The inspired oxygen of group L is 35.4 ± 4.0% in 180 min. The group H had little difference in inspired oxygen concentration over time and decreased by 1.8% for 180 min.
Conclusions
The inspired oxygen concentration is maintained at 30% or more for 180 min in patients under 90 kg. Despite some technical difficulties, low flow anesthesia may be considered.
Figure
Reference
-
1. Foldes FF, Ceravolo AJ, Carpenter SL. The administration of nitrous oxide-oxygen anesthesia in closed systems. Ann Surg. 1952; 136:978–81.2. Virtue RW. Minimal-flow nitrous oxide anesthesia. Anesthesiology. 1974; 40:196–8.3. Geoffrey N. Low-flow anaesthesia. Contin Educ Anaesth Crit Care Pain. 2008; 8:1–4.4. Hargasser S, Hipp R, Breinbauer B, Mielke L, Entholzner E, Rust M. A lower solubility recommends the use of desflurane more than isoflurane, halothane, and enflurane under low-flow conditions. J Clin Anesth. 1995; 7:49–53.5. Baum J. Low flow anaesthesia: the theory and practice of low flow, minimal flow and closed system anaesthesia. 2nd ed. Boston: Butterworth-Heinemann;2001. p. 195–234.6. Kim KO. Low-flow anesthesia in children: theory and clinical practice. Anesth Pain Med. 2012; 7:103–9.7. Kennedy RR, Hendrickx JF, Feldman JM. There are no dragons: low-flow anaesthesia with sevoflurane is safe. Anaesth Intensive Care. 2019; 47:223–5.8. Venkatachalapathy R, Cherian A, Panneerselvam S. Changes in gas composition during low flow anaesthesia without nitrous oxide. J Clin Diagn Res. 2017; 11:UC29–33.9. Fernández-Guisasola J, Gómez-Arnau JI, Cabrera Y, del Valle SG. Association between nitrous oxide and the incidence of postoperative nausea and vomiting in adults: a systematic review and meta-analysis. Anaesthesia. 2010; 65:379–87.10. Raymond JA. Prediction of inspired oxygen concentration within a circle anaesthetic system. Br J Anaesth. 1976; 48:217–23.11. Togal T, Demirbilek S, Koroglu A, Ersoy O. Minimal and medium flow anaesthesia with isoflurane and desflurane: effects on inspired and expired oxygen and anaesthetic gas concentrations. Internet J Anesthesiol. 2008; 18:1–21.12. Brody S. Bioenergetics and growth: with special reference to the efficiency complex in domestic animals. New York: Reinhold;1945. p. xii–1023.13. Okada K, Asano N, Kimura O, Okada H, Nishio S, Wakusawa R. [Low flow anesthesia using a fresh gas flow of 600 ml.min-1 for 5 hours]. Masui. 1997; 46:1321–8. Japanese.14. Bailey JM. The pharmacokinetics of volatile anesthetic agent elimination: a theoretical study. J Pharmacokinet Biopharm. 1989; 17:109–23.15. Mapleson WW. The theoretical ideal fresh-gas flow sequence at the start of low-flow anaesthesia. Anaesthesia. 1998; 53:264–72.16. Crawford ME, Carl P, Andersen RS, Mikkelsen BO. Comparison between midazolam and thiopentone-based balanced anaesthesia for day-case surgery. Br J Anaesth. 1984; 56:165–9.17. Sneyd JR, Whaley A, Dimpel HL, Andrews CJ. An open, randomized comparison of alfentanil, remifentanil and alfentanil followed by remifentanil in anaesthesia for craniotomy. Br J Anaesth. 1998; 81:361–4.18. Katoh T, Uchiyama T, Ikeda K. Effect of fentanyl on awakening concentration of sevoflurane. Br J Anaesth. 1994; 73:322–5.19. Kleemann PP. Humidity of anaesthetic gases with respect to low flow anaesthesia. Anaesth Intensive Care. 1994; 22:396–408.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Arterial/Alveolar Oxygen Tension Ratio as an Index of Prediction of New Arterial Oxygen Tension
- Change of inspired oxygen concentration and temperature in low flow anesthesia
- In reply: Change of inspired oxygen concentration and temperature in low flow anesthesia
- Uptake of Inhalation Anesthetics at the Different Inflow Rate in Semiclosed Circuit
- Arterial Oxygen Tension Measurements during Nitrous Oxide - Oxygen Anesthesia