Anesth Pain Med.
2020 Oct;15(4):409-416. 10.17085/apm.20076.
Management of massive hemorrhage in pregnant women with placenta previa
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2508402
- DOI: http://doi.org/10.17085/apm.20076
Abstract
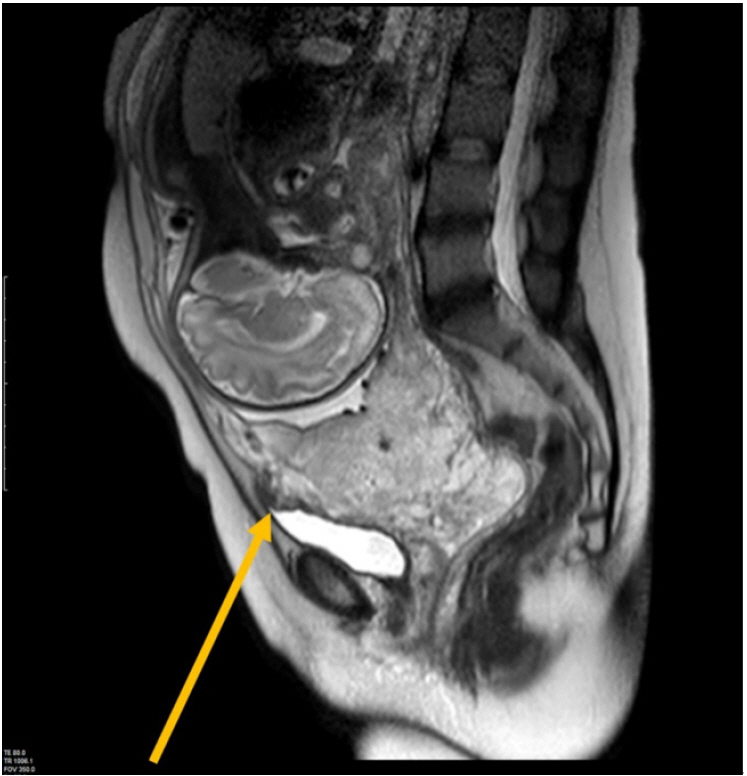
- Patients with placenta previa are at risk for intra- and postpartum massive blood loss as well as increased risk of placenta accreta, a type of abnormal placental implantation. This condition can lead to serious obstetric complications, including maternal mortality and morbidity. The risk factors for previa include prior cesarean section, multiparity, advanced maternal age, prior placenta previa history, prior uterine surgery, and smoking. The prevalence of previa parturients has increased due to the rising rates of cesarean section and advanced maternal age. For these reasons, we need to identify the risk factors for previa and identify adequate management strategies to respond to blood loss during surgery. This review evaluated the diagnosis of placenta previa and placenta accreta and assessed the risk factors for previa-associated bleeding prior to cesarean section. We then presented intraoperative anesthetic management and other interventions to control bleeding in patients with previa expected to experience massive hemorrhage and require transfusion.
Keyword
Figure
Reference
-
1. Lal AK, Hibbard JU. Placenta previa: an outcome-based cohort study in a contemporary obstetric population. Arch Gynecol Obstet. 2015; 292:299–305.2. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014; 2:e323–33.3. Fan D, Xia Q, Liu L, et al. The incidence of postpartum hemorrhage in pregnant women with placenta previa: a systematic review and meta-analysis. PLoS One. 2017; 12:e0170194.4. Crane JM, Van den Hof MC, Dodds L, Armson BA, Liston R. Maternal complications with placenta previa. Am J Perinatol. 2000; 17:101–5.5. Young BC, Nadel A, Kaimal A. Does previa location matter? Surgical morbidity associated with location of a placenta previa. J Perinatol. 2014; 34:264–7.6. Hasegawa J, Matsuoka R, Ichizuka K, Mimura T, Sekizawa A, Farina A, et al. Predisposing factors for massive hemorrhage during cesarean section in patients with placenta previa. Ultrasound Obstet Gynecol. 2009; 34:80–4.7. Rac MW, Dashe JS, Wells CE, Moschos E, McIntire DD, Twickler DM. Ultrasound predictors of placental invasion: the Placenta Accreta Index. Am J Obstet Gynecol. 2015; 212:343.e1-7.8. Finberg HJ, Williams JW. Placenta accreta: prospective sonographic diagnosis in patients with placenta previa and prior cesarean section. J Ultrasound Med. 1992; 11:333–43.9. Hasegawa J, Nakamura M, Hamada S, Matsuoka R, Ichizuka K, Sekizawa A, et al. Prediction of hemorrhage in placenta previa. Taiwan J Obstet Gynecol. 2012; 51:3–6.10. Bowman ZS, Eller AG, Kennedy AM, Richards DS, Winter TC 3rd, Woodward PJ, et al. Accuracy of ultrasound for the prediction of placenta accreta. Am J Obstet Gynecol. 2014; 211:177.e1-7.11. D'Antonio F, Iacovella C, Palacios-Jaraquemada J, Bruno CH, Manzoli L, Bhide A. Prenatal identification of invasive placentation using magnetic resonance imaging: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2014; 44:8–16.12. Dwyer BK, Belogolovkin V, Tran L, Rao A, Carroll I, Barth R, et al. Prenatal diagnosis of placenta accreta: sonography or magnetic resonance imaging? J Ultrasound Med. 2008; 27:1275–81.13. Rao KP, Belogolovkin V, Yankowitz J, Spinnato JA 2nd. Abnormal placentation: evidence-based diagnosis and management of placenta previa, placenta accreta, and vasa previa. Obstet Gynecol Surv. 2012; 67:503–19.14. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997; 177:210–4.15. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006; 107:1226–32.16. Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol. 2006; 107:927–41.17. Ohkuchi A, Onagawa T, Usui R, Koike T, Hiratsuka M, Izumi A, et al. Effect of maternal age on blood loss during parturition: a retrospective multivariate analysis of 10,053 cases. J Perinat Med. 2003; 31:209–15.18. Giambattista E, Ossola MW, Duiella SF, Crovetto F, Acaia B, Somigliana E, et al. Predicting factors for emergency peripartum hysterectomy in women with placenta previa. Arch Gynecol Obstet. 2012; 285:901–6.19. Baba Y, Ohkuchi A, Usui R, Suzuki H, Kuwata T, Matsubara S. Calculating probability of requiring allogeneic blood transfusion using three preoperative risk factors on cesarean section for placenta previa. Arch Gynecol Obstet. 2015; 291:281–5.20. Kim JW, Lee YK, Chin JH, Kim SO, Lee MY, Won HS, et al. Development of a scoring system to predict massive postpartum transfusion in placenta previa totalis. J Anesth. 2017; 31:593–600.21. Lee JY, Ahn EH, Kang S, Moon MJ, Jung SH, Chang SW, et al. Scoring model to predict massive post-partum bleeding in pregnancies with placenta previa: a retrospective cohort study. J Obstet Gynaecol Res. 2018; 44:54–60.22. Liu B, Deng S, Lin M, Chen Y, Cai J, Yang J, et al. Prediction of cesarean hysterectomy in placenta previa complicated with prior cesarean: a retrospective study. BMC Pregnancy Childbirth. 2020; 20:81.23. Shnider SM, Levinson G. Anesthesia for obstetrics. In: Anesthesia. 2nd ed. Edited by Miller RD: New York, Churchill Livingstone. 1986, pp 1661-728.24. Shnider SM, Levinson G. Anesthesia for obstetrics. 3rd ed. Baltimore: Williams & Wilkins;1993. p. 385–94.25. Bonner SM, Haynes SR, Ryall D. The anaesthetic management of caesarean section for placenta praevia: a questionnaire survey. Anaesthesia. 1995; 50:992–4.26. Parekh N, Husaini SW, Russell IF. Caesarean section for placenta praevia: a retrospective study of anaesthetic management. Br J Anaesth. 2000; 84:725–30.27. Shibata K, Yamamoto Y, Murakami S. Effects of epidural anesthesia on cardiovascular response and survival in experimental hemorrhagic shock in dogs. Anesthesiology. 1989; 71:953–9.28. McShane PM, Heyl PS, Epstein MF. Maternal and perinatal morbidity resulting from placenta previa. Obstet Gynecol. 1985; 65:176–82.29. LaPlatney DR, O'Leary JA. Anesthetic considerations in cesarean hysterectomy. Anesth Analg. 1970; 49:328–30.30. Chestnut DH, Dewan DM, Redick LF, Caton D, Spielman FJ. Anesthetic management for obstetric hysterectomy: a multi-institutional study. Anesthesiology. 1989; 70:607–10.31. Yamamoto Y, Yamashita T, Tsuno NH, Nagamatsu T, Okochi N, Hyodo H, et al. Safety and efficacy of preoperative autologous blood donation for high-risk pregnant women: experience of a large university hospital in Japan. J Obstet Gynaecol Res. 2014; 40:1308–16.32. Muñoz M, Stensballe J, Ducloy-Bouthors AS, Bonnet MP, De Robertis E, Fornet I, et al. Patient blood management in obstetrics: prevention and treatment of postpartum haemorrhage. A NATA consensus statement. Blood Transfus. 2019; 17:112–36.33. Green L, Knight M, Seeney F, Hopkinson C, Collins PW, Collis RE, et al. The haematological features and transfusion management of women who required massive transfusion for major obstetric haemorrhage in the UK: a population based study. Br J Haematol. 2016; 172:616–24.34. Toledano RD, Leffert LR. Anesthetic and obstetric management of placenta accreta: clinical experience and available evidence. Curr Anesthesiol Rep. 2017; 7:93–102.35. Burtelow M, Riley E, Druzin M, Fontaine M, Viele M, Goodnough LT. How we treat: management of life-threatening primary postpartum hemorrhage with a standardized massive transfusion protocol. Transfusion. 2007; 47:1564–72.36. Wikkelsø AJ, Edwards HM, Afshari A, Stensballe J, Langhoff-Roos J, Albrechtsen C, FIB-PPH trial group, et al. Pre-emptive treatment with fibrinogen concentrate for postpartum haemorrhage: randomized controlled trial. Br J Anaesth. 2015; 114:623–33.37. Yokoyama K, Suzuki M, Shimada Y, Matsushima T, Bito H, Sakamoto A. Effect of administration of pre-warmed intravenous fluids on the frequency of hypothermia following spinal anesthesia for Cesarean delivery. J Clin Anesth. 2009; 21:242–8.38. Ngan Kee WD, Lee SW, Ng FF, Tan PE, Khaw KS. Randomized double-blinded comparison of norepinephrine and phenylephrine for maintenance of blood pressure during spinal anesthesia for cesarean delivery. Anesthesiology. 2015; 122:736–45.39. Sekhavat L, Tabatabaii A, Dalili M, Farajkhoda T, Tafti AD. Efficacy of tranexamic acid in reducing blood loss after cesarean section. J Matern Fetal Neonatal Med. 2009; 22:72–5.40. WOMAN Trial Collaborators. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017; 389:2105–16.41. Imbesi S, Nettis E, Minciullo PL, Di Leo E, Saija A, Vacca A, et al. Hypersensitivity to tranexamic acid: a wide spectrum of adverse reactions. Pharm World Sci. 2010; 32:416–9.42. Holst LB, Petersen MW, Haase N, Perner A, Wetterslev J. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ. 2015; 350:h1354.43. Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013; 368:11–21.44. Prick BW, Jansen AJ, Steegers EA, Hop WC, Essink-Bot ML, Uyl-de Groot CA, et al. Transfusion policy after severe postpartum haemorrhage: a randomised non-inferiority trial. BJOG. 2014; 121:1005–14.45. British Committee for Standards in Haematology, Stainsby D, MacLennan S, Thomas D, Isaac J, Hamilton PJ. Guidelines on the management of massive blood loss. Br J Haematol. 2006; 135:634–41.46. Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H, PPH Study Group, et al. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007; 5:266–73.47. Jensen NH, Stensballe J, Afshari A. Comparing efficacy and safety of fibrinogen concentrate to cryoprecipitate in bleeding patients: a systematic review. Acta Anaesthesiol Scand. 2016; 60:1033–42.48. Mallaiah S, Barclay P, Harrod I, Chevannes C, Bhalla A. Introduction of an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage. Anaesthesia. 2015; 70:166–75.49. Heaston DK, Mineau DE, Brown BJ, Miller FJ Jr. Transcatheter arterial embolization for control of persistent massive puerperal hemorrhage after bilateral surgical hypogastric artery ligation. AJR Am J Roentgenol. 1979; 133:152–4.50. Evans S, McShane P. The efficacy of internal iliac artery ligation in obstetric hemorrhage. Surg Gynecol Obstet. 1985; 160:250–3.51. Likis FE, Sathe NA, Morgans AK, Hartmann KE, Young JL, Carlson-Bremer D, et al. Management of postpartum hemorrhage. Rockville, U.S. Department of Health and Human Services;2015.52. Pelage JP, Le Dref O, Mateo J, Soyer P, Jacob D, Kardache M, et al. Life-threatening primary postpartum hemorrhage: treatment with emergency selective arterial embolization. Radiology. 1998; 208:359–62.53. Lee JW, Song IA, Ryu J, Park HP, Jeon YT, Hwang JW. Anesthetic management of a parturient with placenta previa totalis undergoing preventive uterine artery embolization before placental expulsion during cesarean delivery: a case report. Korean J Anesthesiol. 2014; 67:279–82.54. Shrivastava V, Nageotte M, Major C, Haydon M, Wing D. Case-control comparison of cesarean hysterectomy with and without prophylactic placement of intravascular balloon catheters for placenta accreta. Am J Obstet Gynecol. 2007; 197:402.e1-5.55. Bishop S, Butler K, Monaghan S, Chan K, Murphy G, Edozien L. Multiple complications following the use of prophylactic internal iliac artery balloon catheterisation in a patient with placenta percreta. Int J Obstet Anesth. 2011; 20:70–3.56. Cho YJ, Oh YT, Kim SY, Kim JY, Jung SY, Chon SJ, et al. The efficacy of pre-delivery prophylactic trans-catheter arterial balloon occlusion of bilateral internal iliac artery in patients with suspected placental adhesion. Obstet Gynecol Sci. 2017; 60:18–25.57. Cali G, Forlani F, Giambanco L, Amico ML, Vallone M, Puccio G, et al. Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. Eur J Obstet Gynecol Reprod Biol. 2014; 179:36–41.58. Carnevale FC, Kondo MM, de Oliveira Sousa W Jr, Santos AB, da Motta Leal Filho JM, Moreira AM, et al. Perioperative temporary occlusion of the internal iliac arteries as prophylaxis in cesarean section at risk of hemorrhage in placenta accreta. Cardiovasc Intervent Radiol. 2011; 34:758–64.59. Ji SM, Cho C, Choi G, Song J, Kwon MA, Park JH, et al. Successful management of uncontrolled postpartum hemorrhage due to morbidly adherent placenta with Resuscitative endovascular balloon occlusion of the aorta during emergency cesarean section - a case report -. Anesth Pain Med. 2020; 15:314–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictive Model of Massive Hemorrhage in Pregnant Women of Previous Cesarean Section with Placenta Previa
- One Case of Placenta Previa Percreta with Bladder Invasion - One Case Report -
- Probability Model of Massive Hemorrhage in Patients with Placenta Previa
- A Case of Placenta Percreta Involving the Urinary Bladder
- Clinical Association of Unexplained Elevated Maternal Serum Alpha-Fetoprotein with Adverse Outcomes in Pregnancies Complicated by Placenta Previa