Yeungnam Univ J Med.
2020 Oct;37(4):337-340. 10.12701/yujm.2020.00402.
Ureterosciatic hernia causing obstructive uropathy successfully managed with minimally invasive procedures
- Affiliations
-
- 1Department of Urology, Yeungnam University Hospital, Daegu, Korea
- 2Department of Radiology, Yeungnam University College of Medicine, Daegu, Korea
- 3Department of Urology, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2508181
- DOI: http://doi.org/10.12701/yujm.2020.00402
Abstract
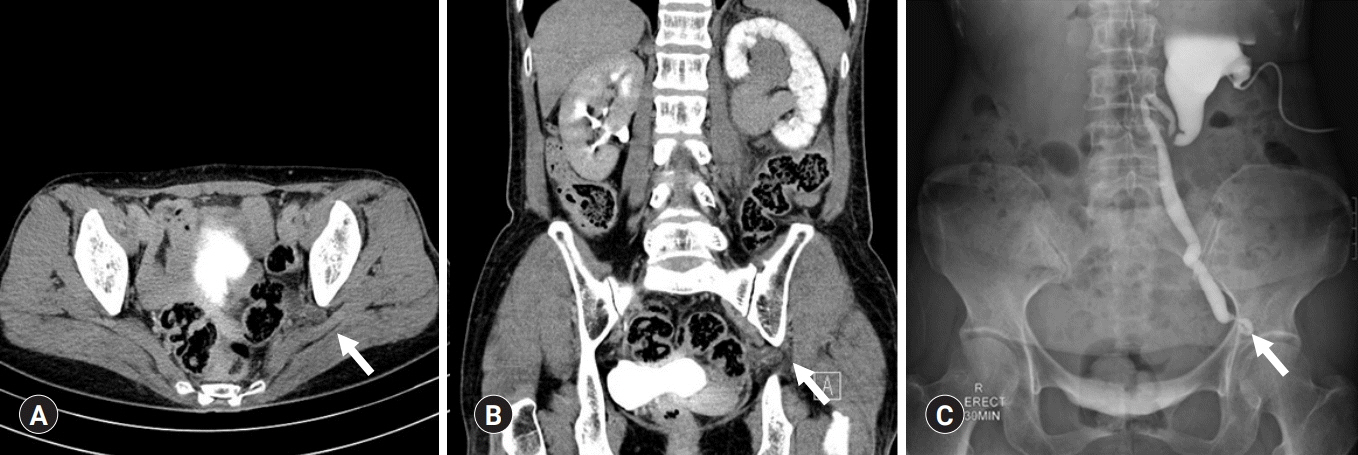
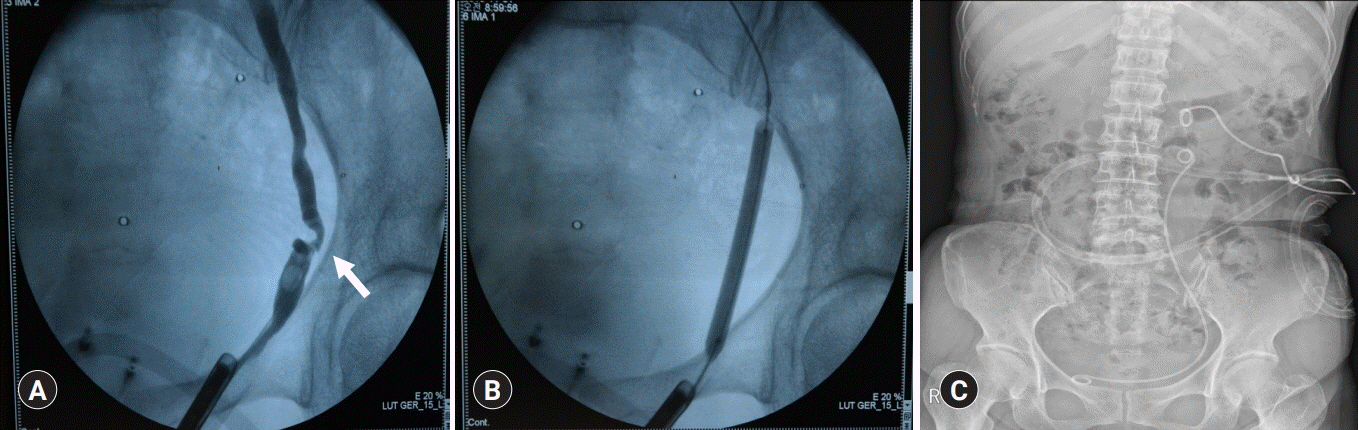
- Ureterosciatic hernia is extremely rare. In ureteral herniation, ureter prolapses occur through either the greater or lesser sciatic foramen. Atrophy of the piriformis muscle, hip joint diseases, and defects in the parietal pelvic fascia are predisposing factors for the development of ureterosciatic hernia. Most symptomatic patients have been treated surgically, with conservative treatment reserved only for asymptomatic patients. To the best of our knowledge, long-term follow-up outcomes after ureterosciatic hernia management are sparse. In this paper, we report the case of a 68-year-old woman who presented with colicky left abdominal pain. After computed tomography (CT) scan and anterograde pyelography, she was diagnosed ureterosciatic hernia with obstructive uropathy. We performed ureteral balloon dilatation and double-J ureteral stent placement. After this minimally invasive procedure, CT scan demonstrated that the left ureter had returned to its normal anatomical position without looping into the sciatic foramen. The patient remained asymptomatic with no adverse events 7 years after the minimally invasive procedures. This brief report describes ureterosciatic hernia successfully managed with minimally invasive procedures with long-term follow-up outcomes.
Figure
Reference
-
References
1. Witney-Smith C, Undre S, Salter V, Al-Akraa M. An unusual case of a ureteric hernia into the sciatic foramen causing urinary sepsis: successfully treated laparoscopically. Ann R Coll Surg Engl. 2007; 89:W10–2.
Article2. Nakazawa Y, Morita N, Chikazawa I, Miyazawa K. Ureterosciatic hernia treated with ureteral stent placement. BMJ Case Rep. 2018; 2018:bcr2017222908.
Article3. Rommel FM, Boline GB, Huffnagle HW. Ureterosciatic hernia: an anatomical radiographic correlation. J Urol. 1993; 150:1232–4.
Article4. Weintraub JL, Pappas GM, Romano WJ, Kirsch MJ, Spencer W. Percutaneous reduction of ureterosciatic hernia. AJR Am J Roentgenol. 2000; 175:181–2.
Article5. Hayashi N, Suwa T, Kimura F, Okuno A, Ishizuka M, Kakizaki S, et al. Radiographic diagnosis and surgical repair of a sciatic hernia: report of a case. Surg Today. 1995; 25:1066–8.
Article6. Tsuzaka Y, Saisu K, Tsuru N, Homma Y, Ihara H. Laparoscopic repair of a ureteric sciatic hernia: report of a case. Case Rep Urol. 2014; 2014:787528.
Article7. Losanoff JE, Basson MD, Gruber SA, Weaver DW. Sciatic hernia: a comprehensive review of the world literature (1900-2008). Am J Surg. 2010; 199:52–9.
Article8. Tsai PJ, Lin JT, Wu TT, Tsai CC. Ureterosciatic hernia causes obstructive uropathy. J Chin Med Assoc. 2008; 71:491–3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Trans-Mitral Septal Myectomy to Treat Hypertrophic Obstructive Cardiomyopathy
- A New Beginning for the Journal of Minimally Invasive Surgery for the International Recognition and Contribution of Scientific Development of Minimally Invasive Surgery
- Recent Advances in Adult Groin Hernioplasty
- Natural Orifice Transluminal Endoscopic Surgery in Korea
- A Late Adopter's Perspective on Minimally Invasive Surgery: Presidential Lecture at KSEL 2018