Cancer Res Treat.
2020 Oct;52(4):1010-1018. 10.4143/crt.2020.254.
Nomogram for Predicting Central Lymph Node Metastasis in Papillary Thyroid Cancer: A Retrospective Cohort Study of Two Clinical Centers
- Affiliations
-
- 1Department of General Surgery, Shanghai Jiaotong University School of Medicine Affiliated Ruijin Hospital, Shanghai, China
- 2ENT Institute and Department of Otorhinolaryngology, Eye & ENT Hospital, Fudan University, Shanghai, China
- KMID: 2507928
- DOI: http://doi.org/10.4143/crt.2020.254
Abstract
- Purpose
Central lymph node metastasis (CNM) are highly prevalent but hard to detect preoperatively in papillary thyroid carcinoma (PTC) patients, while the significance of prophylactic compartment central lymph node dissection (CLND) remains controversial as a treatment option. We aim to establish a nomogram assessing risks of CNM in PTC patients, and explore whether prophylactic CLND should be recommended.
Materials and Methods
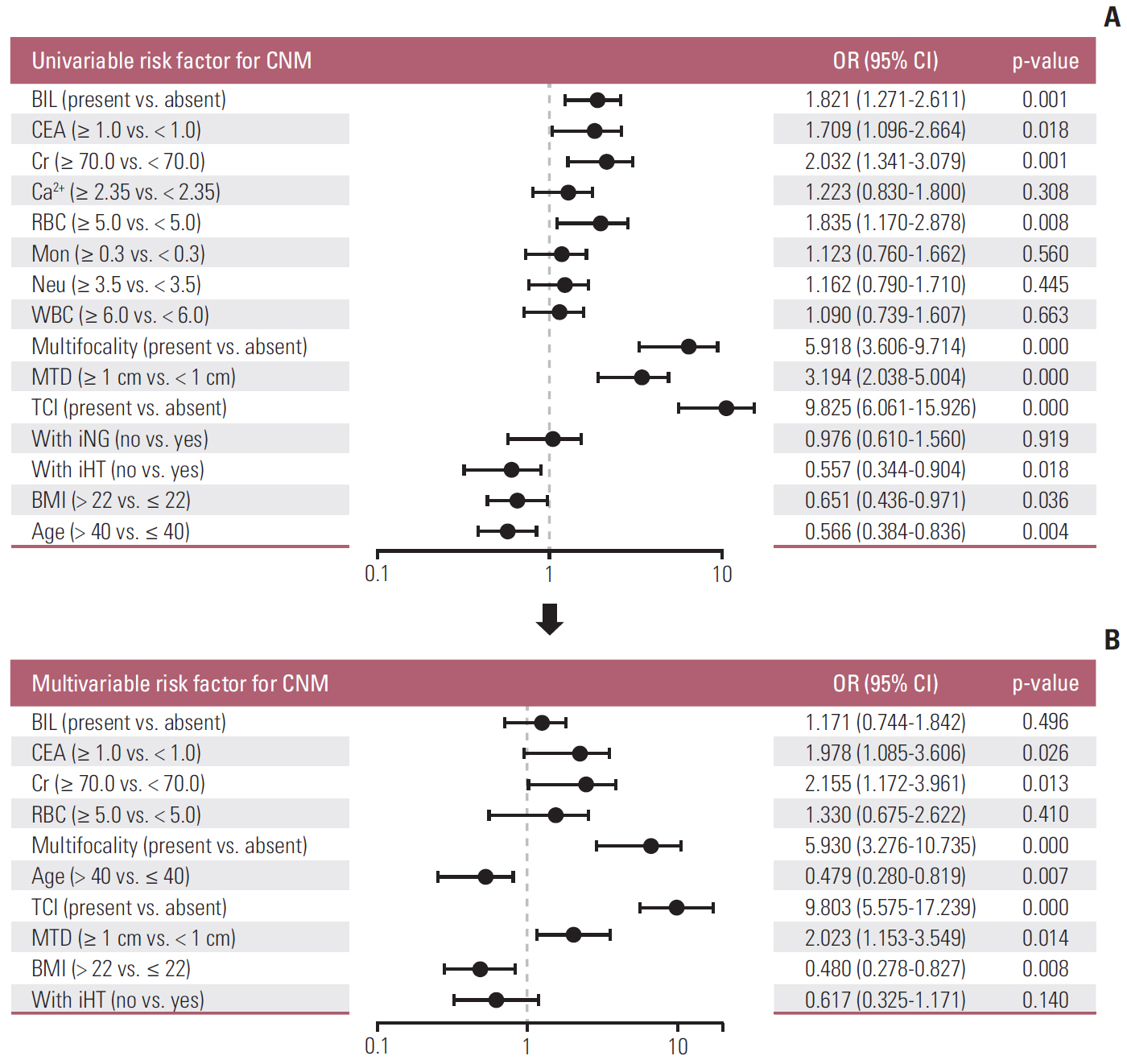
One thousand four hundred thirty-eight patients from two clinical centers that underwent thyroidectomy with CLND for PTC within the period 2016–2019 were retrospectively analyzed. Univariate and multivariate analysis were performed to examine risk factors associated with CNM. A nomogram for predicting CNM was established, thereafter internally and externally validated.
Results
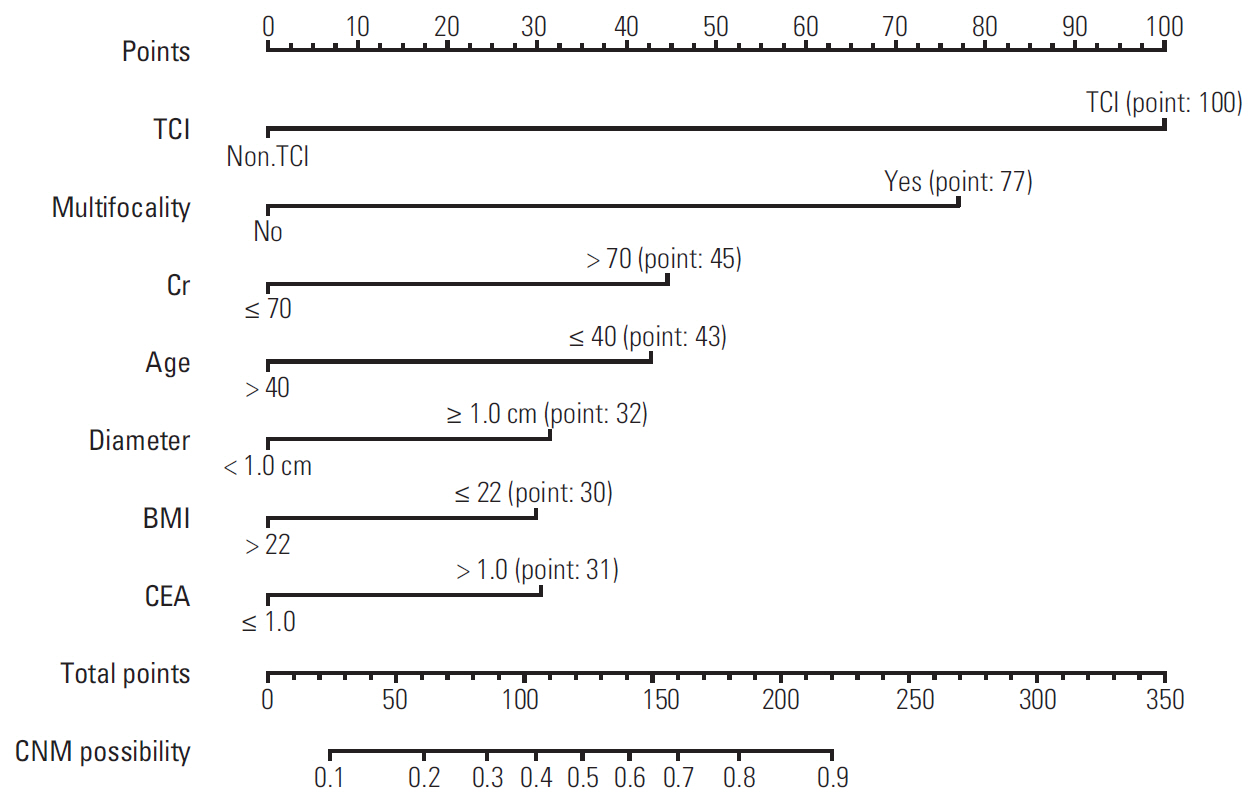
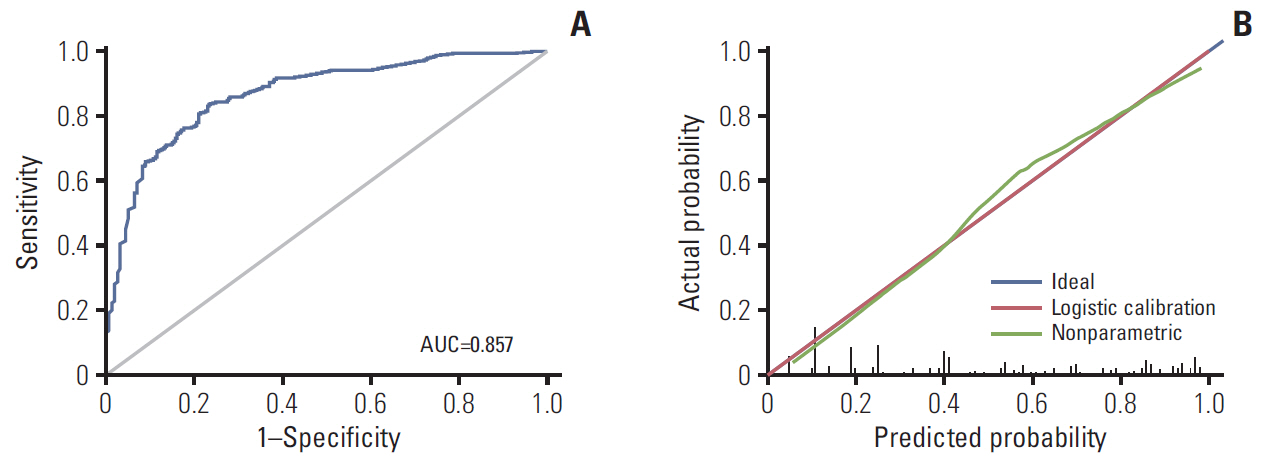
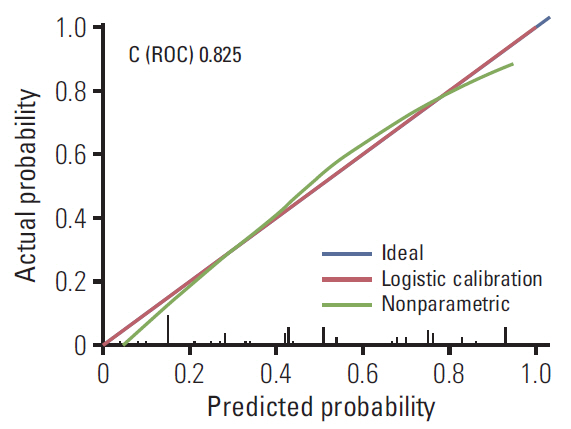
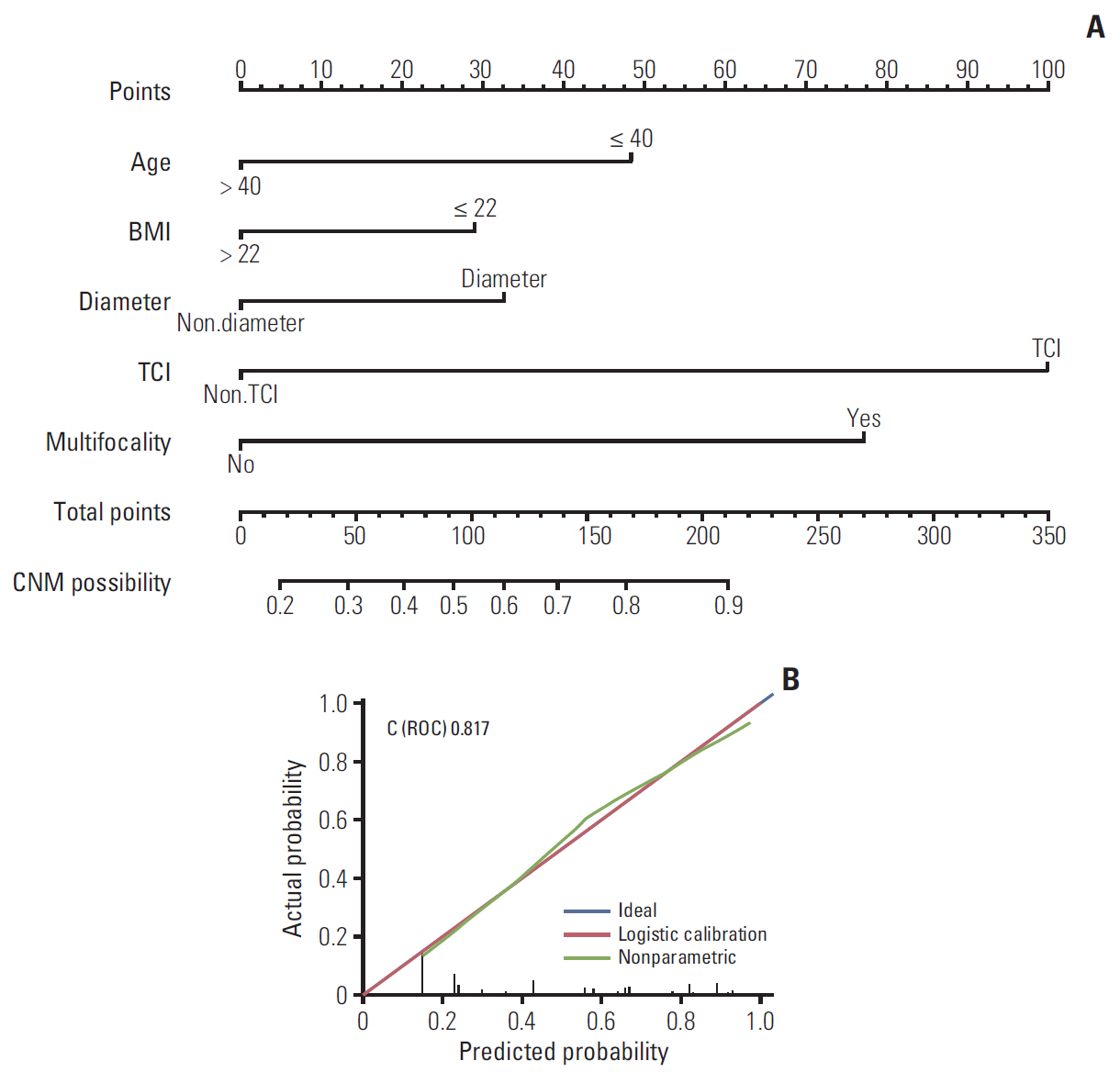
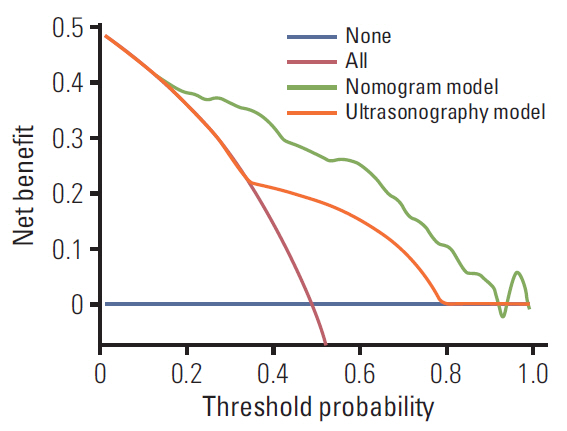
Seven variables were found to be significantly associated with CNM and were used to construct the model. These were as follows: thyroid capsular invasion, multifocality, creatinine > 70 μmol/L, age < 40, tumor size > 1 cm, body mass index < 22, and carcinoembryonic antigen > 1 ng/mL. The nomogram had good discrimination with a concordance index of 0.854 (95% confidence interval [CI], 0.843 to 0.867), supported by an external validation point estimate of 0.825 (95% CI, 0.793 to 0.857). A decision curve analysis was made to evaluate nomogram and ultrasonography for predicting CNM.
Conclusion
A validated nomogram utilizing readily available preoperative variables was developed to predict the probability of central lymph node metastases in patients presenting with PTC. This nomogram may help surgeons make appropriate surgical decisions in the management of PTC, especially in terms of whether prophylactic CLND is warranted.
Figure
Cited by 1 articles
-
Risk factors for central and lateral lymph node metastasis in papillary thyroid carcinoma
Ji Hyun Ahn, Hee Kyung Chang
Kosin Med J. 2022;37(4):311-319. doi: 10.7180/kmj.22.136.
Reference
-
References
1. Maino F, Forleo R, Pacini F. Prognostic indicators for papillary thyroid carcinoma. Expert Rev Endocrinol Metab. 2017; 12:101–8.
Article2. Al Afif A, Williams BA, Rigby MH, Bullock MJ, Taylor SM, Trites J, et al. Multifocal papillary thyroid cancer increases the risk of central lymph node metastasis. Thyroid. 2015; 25:1008–12.
Article3. Bernet V. Approach to the patient with incidental papillary microcarcinoma. J Clin Endocrinol Metab. 2010; 95:3586–92.
Article4. Stulak JM, Grant CS, Farley DR, Thompson GB, van Heerden JA, Hay ID, et al. Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg. 2006; 141:489–94.
Article5. Kim SK, Woo JW, Lee JH, Park I, Choe JH, Kim JH, et al. Prophylactic central neck dissection might not be necessary in papillary thyroid carcinoma: analysis of 11,569 cases from a single institution. J Am Coll Surg. 2016; 222:853–64.
Article6. Thompson AM, Turner RM, Hayen A, Aniss A, Jalaty S, Learoyd DL, et al. A preoperative nomogram for the prediction of ipsilateral central compartment lymph node metastases in papillary thyroid cancer. Thyroid. 2014; 24:675–82.
Article7. Egelmeer AG, Velazquez ER, de Jong JM, Oberije C, Geussens Y, Nuyts S, et al. Development and validation of a nomogram for prediction of survival and local control in laryngeal carcinoma patients treated with radiotherapy alone: a cohort study based on 994 patients. Radiother Oncol. 2011; 100:108–15.
Article8. Wan G, Gao F, Chen J, Li Y, Geng M, Sun L, et al. Nomogram prediction of individual prognosis of patients with hepatocellular carcinoma. BMC Cancer. 2017; 17:91.
Article9. Tuttle RM, Haugen B, Perrier ND. Updated American Joint Committee on Cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid. 2017; 27:751–6.
Article10. Mo S, Dai W, Xiang W, Li Q, Wang R, Cai G. Predictive factors of synchronous colorectal peritoneal metastases: Development of a nomogram and study of its utilities using decision curve analysis. Int J Surg. 2018; 54(Pt A):149–55.
Article11. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.
Article12. Perrino M, Vannucchi G, Vicentini L, Cantoni G, Dazzi D, Colombo C, et al. Outcome predictors and impact of central node dissection and radiometabolic treatments in papillary thyroid cancers < or =2 cm. Endocr Relat Cancer. 2009; 16:201–10.13. Popadich A, Levin O, Lee JC, Smooke-Praw S, Ro K, Fazel M, et al. A multicenter cohort study of total thyroidectomy and routine central lymph node dissection for cN0 papillary thyroid cancer. Surgery. 2011; 150:1048–57.
Article14. Goropoulos A, Karamoshos K, Christodoulou A, Ntitsias T, Paulou K, Samaras A, et al. Value of the cervical compartments in the surgical treatment of papillary thyroid carcinoma. World J Surg. 2004; 28:1275–81.
Article15. Lee YS, Kim SW, Kim SW, Kim SK, Kang HS, Lee ES, et al. Extent of routine central lymph node dissection with small papillary thyroid carcinoma. World J Surg. 2007; 31:1954–9.
Article16. Moo TA, McGill J, Allendorf J, Lee J, Fahey T 3rd, Zarnegar R. Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg. 2010; 34:1187–91.
Article17. Sancho JJ, Lennard TW, Paunovic I, Triponez F, Sitges-Serra A. Prophylactic central neck disection in papillary thyroid cancer: a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg. 2014; 399:155–63.
Article18. Kim BW, Yousman W, Wong WX, Cheng C, McAninch EA. Less is more: comparing the 2015 and 2009 American Thyroid Association guidelines for thyroid nodules and cancer. Thyroid. 2016; 26:759–64.
Article19. Thomas SN, Rohner NA, Edwards EE. Implications of lymphatic transport to lymph nodes in immunity and immunotherapy. Annu Rev Biomed Eng. 2016; 18:207–33.
Article20. Lee YS, Lim YS, Woo CG, Lee JC, Wang SG, Lee KD, et al. PP049: growth pattern of micropapillary thyroid cancer without extrathyroidal extension predicts central lymph node metastasis. Oral Oncol. 2013; 49(Suppl 1):S110.21. Usluogullari CA, Onal ED, Ozdemir E, Ucler R, Kiyak G, Ersoy PE, et al. A retrospective analysis of prognostic factors predictive of lymph-node metastasis and recurrence in thyroid papillary microcarcinoma. Minerva Endocrinol. 2015; 40:15–22.22. Grebe SK, Hay ID. Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am. 1996; 5:43–63.
Article23. Wang Y, Guan Q, Xiang J. Nomogram for predicting central lymph node metastasis in papillary thyroid microcarcinoma: a retrospective cohort study of 8668 patients. Int J Surg. 2018; 55:98–102.
Article24. Kim SK, Chai YJ, Park I, Woo JW, Lee JH, Lee KE, et al. Nomogram for predicting central node metastasis in papillary thyroid carcinoma. J Surg Oncol. 2017; 115:266–72.
Article25. Wu C, Wang L, Chen W, Zou S, Yang A. Associations between body mass index and lymph node metastases of patients with papillary thyroid cancer: a retrospective study. Medicine (Baltimore). 2017; 96:e6202.26. Dieringer P, Klass EM, Caine B, Smith-Gagen J. Associations between body mass and papillary thyroid cancer stage and tumor size: a population-based study. J Cancer Res Clin Oncol. 2015; 141:93–8.
Article27. Mete O, Rotstein L, Asa SL. Controversies in thyroid pathology: thyroid capsule invasion and extrathyroidal extension. Ann Surg Oncol. 2010; 17:386–91.
Article28. Kim ES, Lim DJ, Lee K, Jung CK, Bae JS, Jung SL, et al. Absence of galectin-3 immunostaining in fine-needle aspiration cytology specimens from papillary thyroid carcinoma is associated with favorable pathological indices. Thyroid. 2012; 22:1244–50.
Article29. Furlan JC, Bedard YC, Rosen IB. Significance of tumor capsular invasion in well-differentiated thyroid carcinomas. Am Surg. 2007; 73:484–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Pattern of Cervical Lymph Node Metastases in Papillary Thyroid Cancer
- Central Neck Lymph Node Metastasis from Papillary Thyroid Cancers
- A Case of Cystic Lymph Node Metastasis from Thyroid Papillary Microcarcinoma
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer
- A Clinical Review of Lymph Node Metastases for Papillary Thyroid Cancer