J Korean Med Sci.
2020 Oct;35(41):e355. 10.3346/jkms.2020.35.e355.
Trends of Cause of Death among Human Immunodeficiency Virus Patients and the Impact of Low CD4 Counts on Diagnosis to Death: a Retrospective Cohort Study
- Affiliations
-
- 1Division of Infectious Disease, Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2507827
- DOI: http://doi.org/10.3346/jkms.2020.35.e355
Abstract
- Background
Monitoring the full spectrum of causes of death among human immunodeficiency virus (HIV) patients has become increasingly important as survival improves because of highly active antiretroviral therapy. However, there are no recently published data regarding the changes in the causes of death among HIV patients based on year of HIV diagnosis, and the impact of low CD4 count at the time of HIV diagnosis on the clinical outcome is still unclear in Korea.
Methods
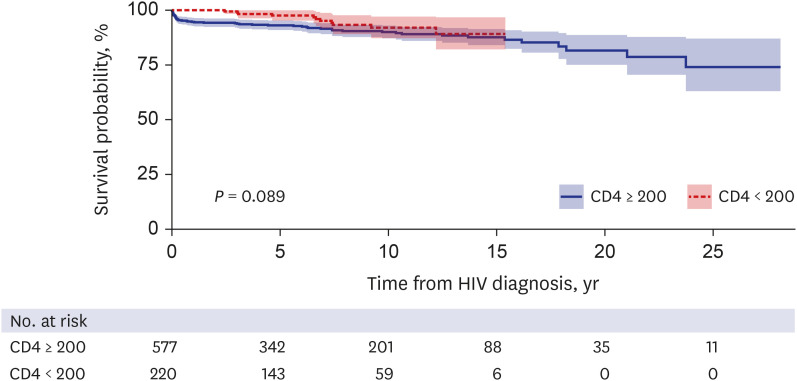
A retrospective cohort study was conducted with 801 patients with HIV infection who were followed up at a tertiary university hospital and diagnosed with HIV between July 1984 and October 2019. The causes of death were analyzed by descriptive analysis based on CD4 count and the year of HIV diagnosis. Kaplan–Meier and log rank tests were performed to compare the prognosis between the CD4 < 200 cells/mm 3 and CD4 ≥ 200 cells/mm 3 groups.
Results
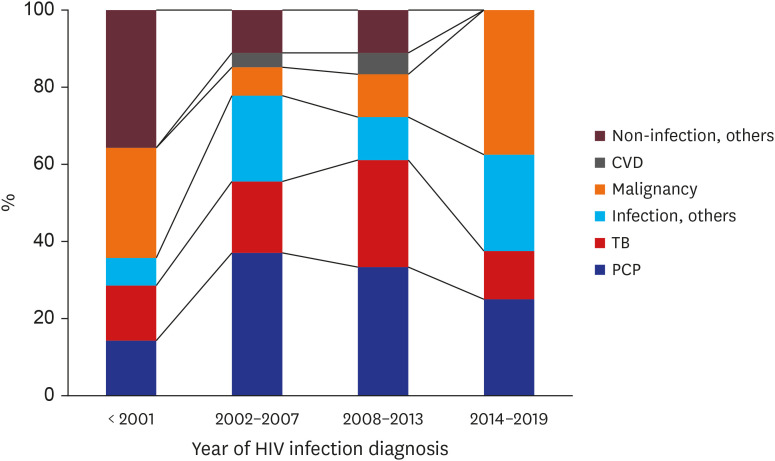
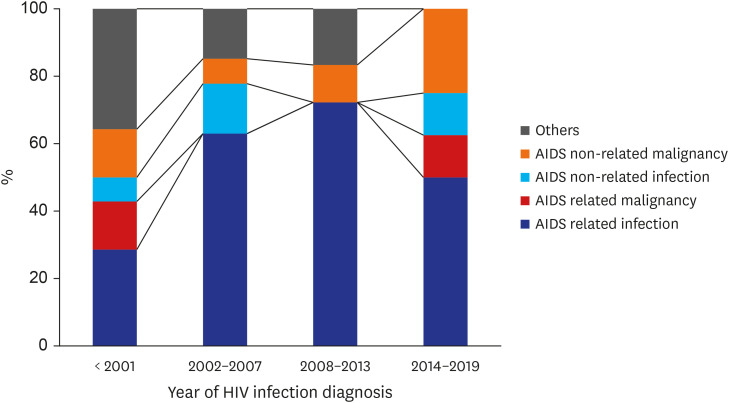
Among 801 patients, 67 patients were eligible for the death cause analysis. Infection-related death accounted for 44 patients (65.7%) and non-infection related death accounted for 23 patients (32.4%). Pneumocystis pneumonia (29.9%) was the single most common cause of death in both past and present cases, and tuberculosis (19.4%) was the second leading cause of death from infections, but the frequency has declined in recent years. Causes of infection-related death have decreased, whereas non-infection related causes of death have increased remarkably. Malignancy-related death was the most common cause of non-infection related death. Acquired immunodeficiency syndrome (AIDS) non-related malignancy accounted for 11.9%, whereas AIDS-related malignancy accounted for 6.0% of the total death among HIV patients. No significant statistical differences were found in mortality rate (P = 0.228), causes of death (P = 0.771), or survival analysis (P = 0.089) between the CD4 < 200 cells/mm3 and CD4 ≥ 200 cells/mm3 groups.
Conclusion
Being diagnosed with CD4 < 200 cells/mm3 at the time of HIV diagnosis was not an indicator of greater risk of death compared with the CD4 ≥ 200 cells/mm3 group. Malignant tumors have become an important cause of death in recent years, and an increasing tendency of AIDS-non-related malignancy causes has been observed.
Keyword
Figure
Reference
-
1. Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, d'Arminio Monforte A, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003; 362(9377):22–29. PMID: 12853195.
Article2. Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV outpatient study investigators. N Engl J Med. 1998; 338(13):853–860. PMID: 9516219.3. Samji H, Cescon A, Hogg RS, Modur SP, Althoff KN, Buchacz K, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One. 2013; 8(12):e81355. PMID: 24367482.
Article4. Mills EJ, Bakanda C, Birungi J, Chan K, Ford N, Cooper CL, et al. Life expectancy of persons receiving combination antiretroviral therapy in low-income countries: a cohort analysis from Uganda. Ann Intern Med. 2011; 155(4):209–216. PMID: 21768555.
Article5. Kee MK, Lee JH, Kim EJ, Lee J, Nam JG, Yoo BH, et al. Improvement in survival among HIV-infected individuals in the Republic of Korea: need for an early HIV diagnosis. BMC Infect Dis. 2009; 9(1):128. PMID: 19671189.
Article6. Lee SH, Kim KH, Lee SG, Chen DH, Jung DS, Moon CS, et al. Trends of mortality and cause of death among HIV-infected patients in Korea, 1990–2011. J Korean Med Sci. 2013; 28(1):67–73. PMID: 23341714.
Article7. Yun JW, Son M. Forecasting cause-specific mortality in Korea up to year 2032. J Korean Med Sci. 2016; 31(8):1181–1189. PMID: 27478326.
Article8. Choi Y, Choi BY, Kim SM, Kim SI, Kim J, Choi JY, et al. Epidemiological characteristics of HIV infected Korean: Korea HIV/AIDS cohort study. Epidemiol Health. 2019; 41:e2019037. PMID: 31623426.
Article9. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009; 24(1):63–71. PMID: 19004861.
Article10. From the Centers for Disease Control and Prevention. From the Centers for Disease Control and Prevention. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. JAMA. 1993; 269(6):729–730. PMID: 8093740.11. Weinberg JL, Kovarik CL. The WHO clinical staging system for HIV/AIDS. Virtual Mentor. 2010; 12(3):202–206. PMID: 23140869.12. Zhang F, Dou Z, Ma Y, Zhao Y, Liu Z, Bulterys M, et al. Five-year outcomes of the China national free antiretroviral treatment program. Ann Intern Med. 2009; 151(4):241–251. PMID: 19687491.
Article13. Zhang G, Gong Y, Wang Q, Deng L, Zhang S, Liao Q, et al. Outcomes and factors associated with survival of patients with HIV/AIDS initiating antiretroviral treatment in Liangshan Prefecture, southwest of China: a retrospective cohort study from 2005 to 2013. Medicine (Baltimore). 2016; 95(27):e3969. PMID: 27399071.14. de Olalla PG, Manzardo C, Sambeat MA, Ocaña I, Knobel H, Humet V, et al. Epidemiological characteristics and predictors of late presentation of HIV infection in Barcelona (Spain) during the period 2001–2009. AIDS Res Ther. 2011; 8(1):22. PMID: 21729332.
Article15. Egger M, May M, Chêne G, Phillips AN, Ledergerber B, Dabis F, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002; 360(9327):119–129. PMID: 12126821.
Article16. May MT, Vehreschild JJ, Trickey A, Obel N, Reiss P, Bonnet F, et al. Mortality according to CD4 count at start of combination antiretroviral therapy among HIV-infected patients followed for up to 15 years after start of treatment: collaborative cohort study. Clin Infect Dis. 2016; 62(12):1571–1577. PMID: 27025828.
Article17. Ren L, Li J, Zhou S, Xia X, Xie Z, Liu P, et al. Prognosis of HIV patients receiving antiretroviral therapy according to CD4 counts: a long-term follow-up study in Yunnan, China. Sci Rep. 2017; 7(1):9595. PMID: 28852017.
Article18. Nishijima T, Inaba Y, Kawasaki Y, Tsukada K, Teruya K, Kikuchi Y, et al. Mortality and causes of death in people living with HIV in the era of combination antiretroviral therapy compared with the general population in Japan. AIDS. 2020; 34(6):913–921. PMID: 32039993.
Article19. Garriga C, García de Olalla P, Miró JM, Ocaña I, Knobel H, Barberá MJ, et al. Mortality, causes of death and associated factors relate to a large HIV population-based cohort. PLoS One. 2015; 10(12):e0145701. PMID: 26716982.
Article20. Burch LS, Smith CJ, Anderson J, Sherr L, Rodger AJ, O'Connell R, et al. Socioeconomic status and treatment outcomes for individuals with HIV on antiretroviral treatment in the UK: cross-sectional and longitudinal analyses. Lancet Public Health. 2016; 1(1):e26–36. PMID: 28299369.
Article21. Gilks CF, Crowley S, Ekpini R, Gove S, Perriens J, Souteyrand Y, et al. The WHO public-health approach to antiretroviral treatment against HIV in resource-limited settings. Lancet. 2006; 368(9534):505–510. PMID: 16890837.
Article22. Antiretroviral Therapy Cohort Collaboration. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017; 4(8):e349–56. PMID: 28501495.23. Nachega JB, Parienti JJ, Uthman OA, Gross R, Dowdy DW, Sax PE, et al. Lower pill burden and once-daily antiretroviral treatment regimens for HIV infection: a meta-analysis of randomized controlled trials. Clin Infect Dis. 2014; 58(9):1297–1307. PMID: 24457345.
Article24. Burchell AN, Raboud J, Donelle J, Loutfy MR, Rourke SB, Rogers T, et al. Cause-specific mortality among HIV-infected people in Ontario, 1995–2014: a population-based retrospective cohort study. CMAJ Open. 2019; 7(1):E1–7.
Article25. Adih WK, Selik RM, Hall HI, Babu AS, Song R. Associations and trends in cause-specific rates of death among persons reported with HIV infection, 23 U.S. jurisdictions, through 2011. Open AIDS J. 2016; 10(1):144–157. PMID: 27708746.
Article26. Smith CJ, Ryom L, Weber R, Morlat P, Pradier C, Reiss P, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet. 2014; 384(9939):241–248. PMID: 25042234.
Article27. Weber R, Ruppik M, Rickenbach M, Spoerri A, Furrer H, Battegay M, et al. Decreasing mortality and changing patterns of causes of death in the Swiss HIV Cohort Study. HIV Med. 2013; 14(4):195–207. PMID: 22998068.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trend in CD4+ Cell Counts at Diagnosis in Human Immunodeficiency Virus-Infected Persons in Korea
- Safety and Effectiveness of Darunavir in Korean Patients with Human Immunodeficiency Virus 1 Infection: A Post-Marketing Observational Study
- The Prognostic Factors in Human Immunodeficiency Virus Infected Patients
- Trend of CD4+ Cell Counts at Diagnosis and Initiation of Highly Active Antiretroviral Therapy (HAART): Korea HIV/AIDS Cohort Study, 1992-2015
- The Gastrointestinal Infections in Korean Patients with Human Immunodeficiency Virus Infection